Abstract
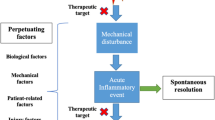
Osteoarthritis is considered an illness in which a complex interaction between the tissues of the joint plays a significant role in the initiation and/or progression of this pathophysiology. We do not yet completely understand all the factors that are responsible for initiating the degradation and loss of the articular tissues. This paper summarizes the novelties of three such mechanisms. The first one points to some factors involved in the regulation of one growth factor family, the bone morphogenetic proteins, the second, the regulation of prostaglandin E2 synthesis, and the third the factors involved in subchondral bone remodeling, all of which could be very significant events for osteoarthritis. This paper should help the reader better understand the most recent advances regarding the roles of these factors in this disease process, and how new therapeutic targets may be identified.
Similar content being viewed by others
References and Recommended Reading
Nakase T, Miyaji T, Tomita T, et al.: Localization of bone morphogenetic protein-2 in human osteoarthritic cartilage and osteophyte. Osteoarthritis Cartilage 2003, 11:278–284.
Bau B, Haag J, Schmid E, et al.: Bone morphogenetic proteinmediating receptor-associated Smads as well as common Smad are expressed in human articular chondrocytes but not up-regulated or down-regulated in osteoarthritic cartilage. J Bone Miner Res 2002, 17:2141–2150.
Matsuda S, Rouault J, Magaud J, et al.: In search of a function for the TIS21/PC3/BTG1/TOB family. FEBS Lett 2001, 497:67–72.
Yoshida Y, Tanaka S, Umemori H, et al.: Negative regulation of BMP/Smad signaling by Tob in osteoblasts. Cell 2000, 103:1085–1097.
Yoshida Y, von Bubnoff A, Ikematsu N, et al.: Tob proteins enhance inhibitory Smad-receptor interactions to repress BMP signaling. Mech Dev 2003, 120:629–637.
Gebauer M, Saas J, Haag J, et al.: Repression of anti-proliferative factor Tob1 in osteoarthritic cartilage. Arthritis Res Ther 2005, 7:R274-R284.
Tardif G, Hum D, Pelletier JP, et al.: Differential gene expression and regulation of the bone morphogenetic protein antagonists follistatin and gremlin in normal and osteoarthritic human chondrocytes and synovial.broblasts. Arthritis Rheum 2004, 50:2521–2530. This is the.rst report on the involvement of bone morphogenetic protein antagonists in osteoarthritis.
Tardif G, Pelletier JP, Hum D, et al.: Differential regulation of the BMP antagonist chordin in human normal and osteoarthritic chondrocytes. Ann Rheum Dis 2005, In press.
Nakayama N, Han CY, Cam L, et al.: A novel chordinlike BMP inhibitor, CHL2, expressed preferentially in chondrocytes of developing cartilage and osteoarthritic joint cartilage. Development 2004, 131:229–240.
Kawabata D, Tanaka M, Fujii T, et al.: Ameliorative effects of follistatin-related protein/TSC-36/FSTL1 on joint inflammation in a mouse model of arthritis. Arthritis Rheum 2004, 50:660–668.
Ijiri K, Zerbini LF, Peng H, et al.: A novel role for GADD45beta as a mediator of MMP-13 gene expression during chondrocyte terminal differentiation. J Biol Chem 2005, (online).
Fan Z, Tardif G, Boileau C, et al.: Identification in osteoarthritic chondrocytes of proteins binding to the novel regulatory site AGRE in the human MMP-13 proximal promoter [abstract]. Arthritis Rheum 2005, 52:S58.
Tanioka T, Nakatani Y, Semmyo N, et al.: Molecular identification of cytosolic prostaglandin E2 synthase that is functionally coupled with cyclooxygenase-1 in immediate prostaglandin E2 biosynthesis. J Biol Chem 2000, 275:32775–32782.
Murakami M, Naraba H, Tanioka T, et al.: Regulation of prostaglandin E2 biosynthesis by inducible membraneassociated prostaglandin E2 synthase that acts in concert with cyclooxygenase-2. J Biol Chem 2000, 275:32783–32792.
Li X, A.f H, Cheng S, et al.: Expression and regulation of microsomal prostaglandin E synthase-1 in human osteoarthritic cartilage and chondrocytes. J Rheumatol 2005, 32:887–895.
Masuko-Hongo K, Berenbaum F, Humbert L, et al.: Upregulation of microsomal prostaglandin E synthase 1 in osteoarthritic human cartilage: critical roles of the ERK-1/2 and p38 signaling pathways. Arthritis Rheum 2004, 50:2829–2838.
Kojima F, Naraba H, Miyamoto S, et al.: Membraneassociated prostaglandin E synthase-1 is upregulated by proinflammatory cytokines in chondrocytes from patients with osteoarthritis. Arthritis Res Ther 2004, 6:R355-R365.
Westman M, Korotkova M, af Klint E, et al.: Expression of microsomal prostaglandin E synthase 1 in rheumatoid arthritis synovium. Arthritis Rheum 2004, 50:1774–1780.
Kojima F, Naraba H, Sasaki Y, et al.: Prostaglandin E2 is an enhancer of interleukin-1beta-induced expression of membrane-associated prostaglandin E synthase in rheumatoid synovial.broblasts. Arthritis Rheum 2003, 48:2819–2828.
Cheng S, A.f H, Martel-Pelletier J, et al.: Activation of peroxisome proliferator-activated receptor γ inhibits interleukin-1β-induced mPGES-1 expression in human synovial.broblasts by interfering with Egr-1. J Biol Chem 2004, 279:22057–22065.
Claveau D, Sirinyan M, Guay J, et al.: Microsomal prostaglandin E synthase-1 is a major terminal synthase that is selectively up-regulated during cyclooxygenase- 2-dependent prostaglandin E2 production in the rat adjuvant-induced arthritis model. J Immunol 2003, 170:4738–4744. This is an elegant study demonstrating, among others, that increased expression of mPGES-1 correlates with enhanced PGE2 synthesis in a rat model of adjuvant-induced arthritis.
Uematsu S, Matsumoto M, Takeda K, et al.: Lipopolysaccharide- dependent prostaglandin E(2) production is regulated by the glutathione-dependent prostaglandin E(2) synthase gene induced by the Toll-like receptor 4/MyD88/NF-IL6 pathway. J Immunol 2002, 168:5811–5816.
Trebino CE, Stock JL, Gibbons CP, et al.: Impaired inflammatory and pain responses in mice lacking an inducible prostaglandin E synthase. Proc Natl Acad Sci U S A 2003, 100:9044–9049.
Kamei D, Yamakawa K, Takegoshi Y, et al.: Reduced pain hypersensitivity and inflammation in mice lacking microsomal prostaglandin e synthase-1. J Biol Chem 2004, 279:33684–33695. An important study supporting the role of mPGES-1 in mediating pain and inflammation. Moreover, this study confirms a critical role of mPGES-1 in the pathogenesis of arthritis.
Engblom D, Saha S, Engstrom L, et al.: Microsomal prostaglandin E synthase-1 is the central switch during immune-induced pyresis. Nat Neurosci 2003, 6:1137–1138.
Carlson CS, Loeser RF, Purser CB, et al.: Osteoarthritis in cynomolgus macaques. III: effects of age, gender, and subchondral bone thickness on the severity of disease. J Bone Miner Res 1996, 11:1209–1217.
Huebner JL, Hanes MA, Beekman B, et al.: A comparative analysis of bone and cartilage metabolism in two strains of guinea-pig with varying degrees of naturally occurring osteoarthritis. Osteoarthritis Cartilage 2002, 10:758–767.
Dieppe P, Cushnaghan J, Young P, et al.: Prediction of the progression of joint space narrowing in osteoarthritis of the knee by bone scintigraphy. Ann Rheum Dis 1993, 52:557–563.
Ferguson VL, Bushby AJ, Boyde A: Nanomechanical properties and mineral concentration in articular calcified cartilage and subchondral bone. J Anat 2003, 203:191–202.
Bailey AJ, Sims TJ, Knott L: Phenotypic expression of osteoblast collagen in osteoarthritic bone: production of type I homotrimer. Int J Biochem Cell Biol 2002, 34:176–182.
Li B, Aspden RM: Mechanical and material properties of the subchondral bone plate from the femoral head of patients with osteoarthritis or osteoporosis. Ann Rheum Dis 1997, 56:247–254.
Messent EA, Buckland-Wright JC, Blake GM: Fractal analysis of trabecular bone in knee osteoarthritis (OA) is a more sensitive marker of disease status than bone mineral density (BMD). Calcif Tissue Int 2005, 76:419–425. Bone mineral density has long been described as elevated in osteoarthritic patients, but we now know that this may be misleading as the tissue is sclerotic yet undermineralized. The proposed approach evaluates the bone tissue quality, which provides much better information on the tissue and its spatial variation than the overall evaluation of BMD.
Conaghan PG, Vanharanta H, Dieppe PA: Is progressive osteoarthritis an atheromatous vascular disease? Ann Rheum Dis 2005, 64:1539–1541. This is the.rst comprehensive overview of the hypothesis that osteoarthritis may be a vascular disease. The comments focus on different key data of the literature demonstrating that abnormal vascular functions are observed in osteoarthritic and may be more than circumstantial.
Shibakawa A, Yudoh K, Masuko-Hongo K, et al.: The role of subchondral bone resorption pits in osteoarthritis: MMP production by cells derived from bone marrow. Osteoarthritis Cartilage 2005, 13:679–687. This manuscript offers an explanation of the possible cross-talk between the subchondral bone plate and the articular cartilage. It suggests what could be the biologic information between the two tissues and how it is carried over between them.
Aspden RM, Scheven BA, Hutchison JD: Osteoarthritis as a systemic disorder including stromal cell differentiation and lipid metabolism. Lancet 2001, 357:1118–1120.
Murphy JM, Dixon K, Beck S, et al.: Reduced chondrogenic and adipogenic activity of mesenchymal stem cells from patients with advanced osteoarthritis. Arthritis Rheum 2002, 46:704–713.
Thomas T, Gori F, Khosla S, et al.: Leptin acts on human marrow stromal cells to enhance differentiation to osteoblasts and to inhibit differentiation to adipocytes. Endocrinology 1999, 140:1630–1638.
Dumond H, Presle N, Terlain B, et al.: Evidence for a key role of leptin in osteoarthritis. Arthritis Rheum 2003, 48:3118–3129.
Lajeunesse D, Delalandre A, Fernandes J: Subchondral osteoblasts from osteoarthritic patients show abnormal expression and production of leptin: possible role in cartilage degradation [abstract]. J Bone Miner Res 2004, 19:S149.
Plumb MS, Aspden RM: High levels of fat and (n-6) fatty acids in cancellous bone in osteoarthritis. Lipids Health Dis 2004, 3:12 (online). It was a well-known fact, yet unpublished, that bone marrow and bone tissue of osteoarthritic patients was "fatty." This study evaluated the amount of lipids in cancellous bone tissue of osteoarthritic patients and shows that it is clearly elevated in (n-6) fatty acids leading to arachidonic acid. This could then explain the elevated amounts of prostaglandins observed in osteoarthritic joint tissues.
Barton M, Carmona R, Ortmann J, et al.: Obesity-associated activation of angiotensin and endothelin in the cardiovascular system. Int J Biochem Cell Biol 2003, 35:826–837.
Quehenberger P, Exner M, Sunder-Plassmann R, et al.: Leptin induces endothelin-1 in endothelial cells in vitro. Circ Res 2002, 90:711–718.
Xu FP, Chen MS, Wang YZ, et al.: Leptin induces hypertrophy via endothelin-1-reactive oxygen species pathway in cultured neonatal rat cardiomyocytes. Circulation 2004, 110:1269–1275.
van den Brink GR, O’Toole T, Hardwick JC, et al.: Leptin signaling in human peripheral blood mononuclear cells, activation of p38 and p42/44 mitogen-activated protein (MAP) kinase and p70 S6 kinase. Mol Cell Biol Res Commun 2000, 4:144–150.
Kadam UT, Jordan K, Croft PR: Clinical comorbidity in patients with osteoarthritis: a case-control study of general practice consulters in England and Wales. Ann Rheum Dis 2004, 63:408–414.
Marks R, Allegrante JP: Comorbid disease profiles of adults with end-stage hip osteoarthritis. Med Sci Monit 2002, 8:CR305–309.
Singh G, Miller JD, Lee FH, et al.: Prevalence of cardiovascular disease risk factors among US adults with self-reported osteoarthritis: data from the Third National Health and Nutrition Examination Sur vey. Am J Manag Care 2002, 8:S383–391.
Kougias P, Chai H, Lin PH, et al.: Effects of adipocytederived cytokines on endothelial functions: implication of vascular disease. J Surg Res 2005, 126:121–129. Since osteoarthritis may be considered a vascular disease, this study shows that adipocyte-derived cytokines such as leptin may be involved in this abnormal function. In addition to the potential direct effect of these adipocytes on joint tissues, it offers a new perspective to evaluate or follow osteoarthritis.
49.Smith AJ, Gidley J, Sandy JR, et al.: Haplotypes of the low-density lipoprotein receptor-related protein 5 (LRP5) gene: are they a risk factor in osteoarthritis? Osteoarthritis Cartilage 2005, 13:608–613. Since we now believe that bone tissue is a key factor in the onset of osteoarthritis, this study illustrates that bone-speci.c genes are altered in osteoarthritic bone tissue. Hence, the LRP5 gene may be a potential target for future research on the cause of osteoarthritis through the bone hypothesis. The paper also offers other potential key target bone genes involved in the disease.
Raynauld JP, Kauffmann C, Beaudoin G, et al.: Reliability of a quantification imaging system using magnetic resonance images to measure cartilage thickness and volume in human normal and osteoarthritic knees. Osteoarthritis Cartilage 2003, 11:351–360.
Raynauld JP, Martel-Pelletier J, Berthiaume MJ, et al.: Quantitative magnetic resonance imaging evaluation of knee osteoarthritis progression over two years and correlation with clinical symptoms and radiologic changes. Arthritis Rheum 2004, 50:476–487. This is the.rst longitudinal study in a large cohort of knee osteoarthritic patients that provides major insight into the predominant risk factors associated with disease progression.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martel-Pelletier, J., Lajeunesse, D., Fahmi, H. et al. New thoughts on the pathophysiology of osteoarthritis: One more step toward new therapeutic targets. Curr Rheumatol Rep 8, 30–36 (2006). https://doi.org/10.1007/s11926-006-0022-6
Issue Date:
DOI: https://doi.org/10.1007/s11926-006-0022-6