Abstract
Purpose of Review
Marijuana use presents a unique challenge to bariatric surgery programs. We review the recent evidence examining marijuana use on outcomes following bariatric surgery.
Recent Findings
Recent studies have not demonstrated an increased risk of short-term surgical complications or differences in up to 2-year weight loss following surgery among marijuana users. However, studies have demonstrated increased risks in two areas: pain management and problematic eating behaviors. Additionally, preoperative marijuana use has been linked to increased postoperative marijuana use which may undermine weight loss and increase risk for weight regain.
Summary
There are still many unanswered questions regarding marijuana use and bariatric surgery, and the limited literature base has produced mixed results when considering marijuana as a contraindication for bariatric surgery. Programs must take into consideration the laws of their state, individual patterns of use, and route of administration when considering whether marijuana is a contraindication for surgery.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hales CM, Fryar CD, Carroll MD, Freedman DS, Aoki Y, Ogden CL. Differences in obesity prevalence by demographic characteristics and urbanization level among adults in the United States, 2013–2016. JAMA 2018: 319:2419–2429. https://doi.org/10.1001/jama.2018.7270
Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. Int J Obes. 2013;37:889–91.
Nguyen NT. Blackstone RP. Ponce J, Rosenthal RJ. The ASMBS textbook of bariatric surgery. Springer: Morton JM; 2015.
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
ASMBS. New procedure estimates for bariatric surgery: what the numbers reveal. 2014; http://connect.asmbs.org/may-2014-bariatric-surgery-growth.html, 2016.
Nguyen NT, Nguyen B, Smith B, Reavis KM, Elliott C, Hohmann S. Proposal for a bariatric mortality risk classification system for patients undergoing bariatric surgery. Surg Obes Relat Dis. 2013;2103(9):239–46.
Adams TD, Davidson LE, Litwin SE, Kim J, Kolotkin RL, Nanjee MN, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;2017(377):1143–55. https://doi.org/10.1056/NEJMoa1700459.
Courcoulas AP, King WC, Belle SH, Berk P, Flum DR, Garcia L, et al. Seven-year weight trajectories and health outcomes in the longitudinal assessment of bariatric surgery (LABS) study. JAMA. 2018;153:427–34. https://doi.org/10.1001/jamasurg.2017.5025.
Courcoulas AP, Christian NJ, Belle SH, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310:2416–25. https://doi.org/10.1001/jama.2013.280928.
Puzziferri N, Roshek TB III, Mayo HG, Gallagher R, Belle SH, Livingston EH. Long-term follow-up after bariatric surgery a systematic review. JAMA. 2014;312(9):934–42.
Karmali S, Brar B, Shi X, Sharma AM, de Gara C, Birch DW. Weight recidivism post-bariatric surgery: a systematic review. Obes Surg. 2013;23(11):1922–33.
Sarwer DB, Heinberg LJ. A review of the psychosocial aspects of clinically severe obesity and bariatric surgery. Am Psychol. 2020;75(2):252–64.
Mechanick JI, Youdim A, Jones DB, et al. Clinical Practice Guidelines for the Perioperative Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery Patient—2013 Update: Cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity 2013:21(0 1):S1–27.
Health NIo. Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr. 1992:55(2 Suppl):615s–619s.
Bauchowitz AU, Gonder-Frederick LA, Oblrisch M, et al. Psychosocial evaluation of bariatric surgery candidates: a survey of present practices. Psychosom Med. 2005;67:825–32.
Heinberg LJ, Pudalov L, Alameddin H, Steffen K. Opioids and bariatric surgery: a review and suggested recommendations for assessment and risk reduction. Surg Obes Relat Dis. 2019;15:314–21.
Rummell C, Heinberg LJ. Assessing marijuana use in bariatric surgery candidates: Should it be a contraindication? Obes Surg 2014:24(10):1764–1770. There is no consensus on effects of cannabis use on bariatric surgery outcomes.
King WC, Chen JY, Mitchell JE, Kalarchian MA, Steffen KJ, Engel SG, et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012;307:2516–25.
Mitchell JE, Selzer F, Kalarchian MA, Devlin MJ, Strain GW, Elder KA, et al. Psychopathology before surgery in the longitudinal assessment of bariatric surgery-3 (LABS-3) psychosocial study. Surg Obes Relat Dis. 2012;8:533–41.
Kalarchian MA, Marcus MD, Levine MD, et al. Psychiatric disorders among bariatric surgery candidates: relationship to obesity and functional health status. Am J Psychiatry. 2007;164:328–34.
Clark MM, Balsiger BM, Sletten CD, Dahlman KL, Ames G, Williams DE, et al. Psychosocial factors and 2-year outcome following bariatric surgery for weight loss. Obes Surg. 2012;13:739–45. https://doi.org/10.1381/096089203322509318.
Heinberg LJ, Ashton K. History of substance abuse relates to improved postbariatric body mass index outcomes. Surg Obes Relat Dis 2012:6:417–421. https://doi.org/10.1016/j.soard .2010.04.001.
DrugFacts: marijuana [Internet]. Rockville (MD): National Institute on Drug Abuse (US), National Institutes of Health; 2019 [cited 2020 Aug 25]. Available from: http://www.drugabuse.gov/publications/ drugfacts/marijuana.
Hudak J. 2014, a make or break year for legal pot [internet]. Washington DC: CNN Opinion; 2013. [cited 2020 Aug 25] Available from: http://www.cnn.com/2013/12/30/opinion/hudakmarijuana-2014/
Kumar N, Puljević C, Ferris J, Winstock A, Barratt MJ. Cannabis use patterns at the dawn of US cannabis reform. Journal of Cannabis Research. 2019 Dec;1(1):1–6.
Goel A, McGuinness B, Jivraj NK, Wijeysundera DN, Mittleman MA, Bateman BT, et al. Cannabis use disorder and perioperative outcomes in major elective surgeries. A retrospective cohort analysis. Anesthesiology: The Journal of the American Society of Anesthesiologists. 2020 Apr 1;132(4):625–35.
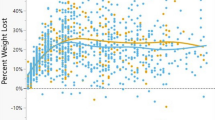
Bauer FL, Donahoo WT, Hollis Jr HW, Tsai AG, Pottorf BJ, Johnson JM, Silveira LJ, Husain FA. Marijuana’s influence on pain scores, initial weight loss, and other bariatric surgical outcomes. The Permanente Journal. 2018; 22. The authors conclude that surgical outcomes at 30 days, improvement in medical conditions, and percentage of total body loss were not affected by marijuana use.
Ambwani S, Boeka AG, Brown JD, Byrne TK, Budak AR, Sarwer DB, et al. Socially desirable responding by bariatric surgery candidates during psychological assessment. Surg Obes Relat Dis. 2013 Mar 1;9(2):300–5.
Shockcor N, Adnan SM, Siegel A, Wise E, Zafar SN, Kligman M. Marijuana use does not affect the outcomes of bariatric surgery. Surgical endoscopy. 2020 Mar 12:1–5. No differences were found in the rate of 30-day postoperative complications or excess BMI lost from 3 weeks-2 years after surgery between marijuana users and non-users.
Vidot DC, Prado G, De La Cruz-Munoz MD, Spadola C, Cuesta M, Messiah SE. Postoperative marijuana use and disordered eating among bariatric surgery patients. Surg Obes Relat Dis 2016:12:171–179. Results suggest that there is a subset of patients who engage in marijuana use after surgery despite recommendations against use. Increased or recent marijuana use was found to predict greater eating disordered behaviors.
Huson HB, Granados TM, Rasko Y. Surgical considerations of marijuana use in elective procedures. Heliyon. 2018 Sep 1;4(9):e00779.
Russell C, Rueda S, Room R, Tyndall M, Fischer B. Routes of administration for cannabis use–basic prevalence and related health outcomes: a scoping review and synthesis. Int J Drug Policy. 2018 Feb 1;52:87–96.
Abrams DI, Vizoso HP, Shade SB, Jay C, Kelly ME, Benowitz NL. Vaporization as a smokeless cannabis delivery system: a pilot study. Clinical Pharmacology & Therapeutics. 2007 Nov;82(5):572–8.
Loflin M, Earleywine M. No smoke, no fire: what the initial literature suggests regarding vapourized cannabis and respiratory risk. Canadian Journal of Respiratory Therapy: CJRT= Revue Canadienne de la Thérapie Respiratoire: RCTR. 2015;51(1):7.
Ghosh TS, Van Dyke M, Maffey A, Whitley E, Erpelding D, Wolk L. Medical marijuana’s public health lessons—implications for retail marijuana in Colorado. N Engl J Med. 2015 Mar 12;372(11):991–3.
MacCoun RJ, Mello MM. Half-baked—the retail promotion of marijuana edibles. N Engl J Med. 2015 Mar 12;372(11):989–91.
Geshtakovska G, Stefkov G. Routes of cannabis administration: a brief review. Your hosts Macedonian Pharmaceutical Association and Faculty of Pharmacy, Ss Cyril and Methodius University in Skopje. 2016;515.
Grotenhermen F. Cannabinoids for therapeutic use. American Journal of Drug Delivery. 2004 Dec 1;2(4):229–40.
Shiplo S, Asbridge M, Leatherdale ST, Hammond D. Medical cannabis use in Canada: vapourization and modes of delivery. Harm Reduct J. 2016 Dec 1;13(1):30.
National Institute on Drug Abuse (US). Marijuana abuse [Internet]. Rockville (MD): National Institutes of Health (US); 2012 July. 12 p. Publication No.: 12–3859.
Allsop DJ, Norberg MM, Copeland J, Fu S, Budney AJ. The Cannabis Withdrawal Scale development: patterns and predictors of cannabis withdrawal and distress. Drug Alcohol Depend. 2011;119:123–9.
Respiratory effects of marijuana [Internet]. Seattle (WA): University of Washington Alcohol and Drug Abuse Institute (US); 2013 Aug [cited 2020 Aug 25]. Available from: http://adai.washington.edu/ mariuana/factsheets/respiratoryeffects.pdf.
Tetrault JM, Crothers K, Moore BA, Mehra R, Concato J, Fiellin DA. Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review. Arch Intern Med. 2007;167:221–8.
Aharonovich E, LiuX SS, et al. Postdischarge cannabis use and its relationship to cocaine, alcohol, and heroin use: a prospective study. Am J Psychiatry. 2005;162:1507–14.
Callaghan RC, Allebeck P, Sidorchuk A. Marijuana use and risk of lung cancer: a 40-year cohort study. Cancer Causes Control. 2013;10:1811–20.
Livingston EH. Obesity, psychological testing and substance abuse. Surg Obes Relat Dis. 2006;2:312.
Warren M, Frost-Pineda K, Gold M. Body mass index and marijuana use. J Addict Dis. 2005;24:95–100.
Pagotto U, Marsicano G, Cota D, Lutz B, Pasquali R. The emerging role of the endocannabinoid system in endocrine regulation and energy balance. Endocr Rev. 2006 Feb;27(1):73–100.
Meany G, Conceicao E, Mitchell JE. Binge eating, binge eating disorder and loss of control eating: effects on weight outcomes after bariatric surgery. Eur Eat Disord Rev. 2014;22(2):87–91. https://doi.org/10.1002/erv.2273.
Sogg S. Alcohol misuse after bariatric surgery: epiphenomenon or “Oprah” phenomenon? Surg Obes Relat Dis. 2007;3:366–8.
Sarwer DB, Allison KC, Wadden TA, Ashare R, Spitzer JC, McCuen-Wurst C. Psychopathology, disordered eating, and impulsivity as predictors of outcomes of bariatric surgery. Surg Obes Relat Dis. 2019;15:650–5.
Ertelt TW, Mitchell JE, Lancaster K, Crosby RD, Steffen KJ, Marino JM. Alcohol abuse and dependence before and after bariatric surgery: a review of the literature and report of a new data set. Surg Obes Relat Dis. 2008;4:647–50. https://doi.org/10.1016/j.soard.2008.01.004.
Suzuki J, Haimovici F, Chang G. Alcohol use disorders after bariatric surgery. Obes Surg. 2012;22:201–7.
King WC, Chen JY, Courcoulas AP, et al. Alcohol and other substance use after bariatric surgery: Prospective evidence from a U.S. multicenter cohort study. Surg Obes Relat Dis 2017:13:1392–1402. Bariatric surgery increases risk of using illicit drugs and undergoing substance use treatment.
King WC, Chen JY, Courcoulas AP, Dakin GF, Engel SG, Flum DR, et al. Alcohol and other substance use after bariatric surgery: prospective evidence from a US multicenter cohort study. Surg Obes Relat Dis. 2017 Aug 1;13(8):1392–402.
Conason A, Teixeira J, Hsu CH, Puma L, Knafo D, Geliebter A. Substance use following bariatric weight loss surgery. JAMA 2013:148: 145–150. org/https://doi.org/10.1001/2013.jamasurg.265
Ivezaj V, Saules KK, Schuh LM. New-onset substance use disorder after gastric bypass surgery: rates and associated characteristics. Obes Surg. 2014;24:1975–80.
Lent MR, Hayes SM, Wood GC, Napolitano MA, Argyropoulos G, Gerhard GS, et al. Smoking and alcohol use in gastric bypass patients. Eat Beh. 2013;14:460–3.
Reslan S, Saules KK, Greenwald MK, Schuh LM. Substance misuse following Roux-en-Y gastric bypass surgery. Subst Use Misuse. 2014;49:405–17.
Raebel MA, Newcomer SR, Bayliss EA, Boudreau D, DeBar L, Elliott TE, et al. Chronic opioid use emerging after bariatric surgery. Pharmacoepidemiol Drug Saf. 2014;23(12):1247–57.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Allyson Diggins and Leslie Heinberg declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Eating Disorders
Rights and permissions
About this article
Cite this article
Diggins, A., Heinberg, L. Marijuana and Bariatric Surgery. Curr Psychiatry Rep 23, 10 (2021). https://doi.org/10.1007/s11920-020-01218-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s11920-020-01218-4