Abstract
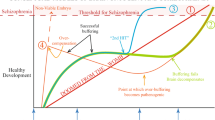
The association between exposure to perinatal risk factors and increased vulnerability for schizophrenia is now documented by a large body of epidemiologic studies. However, the diagnostic specificity of this association may be questioned, because subjects with a history of exposure to early environmental risk factors are at an increased risk for other psychiatric disorders with childhood or adult onset, such as autism, anorexia nervosa, or affective disorders. Because a given risk factor may be associated with several adverse health outcomes, these findings do not preclude the existence of a causal relationship between perinatal risk factors and schizophrenia. This lack of diagnostic specificity suggests that the clinical expression of the vulnerability induced by early risk factors depends on gene-environment interactions or interaction between this prenatally determined vulnerability and exposure to later environmental risk factors.
Similar content being viewed by others
References and Recommended Reading
Murray R, Lewis SW: Is schizophrenia a neurodevelopmental disorder? BMJ 1987, 295:681–682.
Torrey F, Miller J, Rawlings R, et al.: Seasonality of birth in schizophrenia and bipolar disorder: a review of the literature. Schizophr Res 1997, 28:1–38.
McGrath J, Welham J: Season of birth and schizophrenia: a systematic review and meta-analysis of data from the southern hemisphere. Schizophr Res 1999, 35:237–242.
McGrath J, Selten JP, Chant D: Long-term trends in sunshine duration and its association with schizophrenia birth rates and age at first registration. Schizophr Res 2002, 54:199–212.
Landau EC, Cicchetti DV, Klin A, et al.: Season of birth in autism: a fiction revisited. J Autism Dev Disord 1999, 29:385–393.
Rezaul I, Persaud R, Takei N, et al.: Season of birth and eating disorders. Int J Eat Disord 1996, 19:53–61.
Lewis G, David A, Andreasson S, et al.: Schizophrenia and city life. Lancet 1992, 340:137–140.
Mortensen P, Pedersen C, Westegaard T, et al.: Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med 1999, 340:603–608.
Pedersen C, Mortensen P: Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk. Arch Gen Psychiatry 2001, 58:1039–1046.
Geddes JR, Verdoux H, Takei N, et al.: Schizophrenia and complications of pregnancy and labor: an individual patient data meta-analysis. Schizophr Bull 1999, 25:413–423.
Cannon M, Jones P, Murray R: Obstetric complications and schizophrenia: historical and meta-analytic review. Am J Psychiatry 2002, 159:1080–1092. A review of the literature on obstetric complications and schizophrenia.
Jones PB, Rantakallio P, Hartikainen AL, et al.: Schizophrenia as a long-term outcome of pregnancy, delivery, and perinatal complications: a 28-year follow-up of the 1966 north Finland general population birth cohort. Am J Psychiatry 1998, 155:355–364.
Cannon TD, van Erp TG, Rosso IM, et al.: Fetal hypoxia and structural brain abnormalities in schizophrenic patients, their siblings, and controls. Arch Gen Psychiatry 2002, 59:35–41.
Done D, Johnstone E, Frith C, et al.: Complications of pregnancy and delivery in relation to psychosis in adult life: data from the British perinatal mortality survey sample. BMJ 1991, 302:1576–1580.
Sacker A, Done D, Crow T, et al.: Antecedents of schizophrenia and affective illness: obstetric complications. Br J Psychiatry 1995, 166:734–741.
Hultman CM, Sparen P, Takei N, et al.: Prenatal and perinatal risk factors for schizophrenia, affective psychosis, and reactive psychosis of early onset: case-control study. BMJ 1999, 318:421–426.
Zornberg GL, Buka SL, Tsuang MT: Hypoxic-ischemia-related fetal/neonatal complications and risk of schizophrenia and other nonaffective psychoses: a 19-year longitudinal study. Am J Psychiatry 2000, 157:196–202.
Buka S, Fan A: Association of prenatal and perinatal complications with subsequent bipolar disorder and schizophrenia. Schizophr Res 1999, 39:113–119.
Verdoux H, Geddes J, Takei N, et al.: Obstetric complications and age at onset in schizophrenia: an international collaborative meta-analysis of individual patient data. Am J Psychiatry 1997, 154:1220–1227.
Jaffee SR, Moffitt TE, Caspi A, et al.: Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Arch Gen Psychiatry 2002, 59:215–222.
Cnattingius S, Hultman C, Dahl M, et al.: Very preterm birth, birth trauma, and the risk of anorexia nervosa among girls. Arch Gen Psychiatry 1999, 56:634–638.
Foley DL, Thacker LR, Aggen SH, et al.: Pregnancy and perinatal complications associated with risks for common psychiatric disorders in a population-based sample of female twins. Am J Med Genet 2001, 105:426–431.
Bolton PF, Murphy M, Macdonald H, et al.: Obstetric complications in autism: consequences or causes of the condition? J Am Acad Child Adolesc Psychiatr 1997, 36:272–281.
Burd L, Severud R, Kerbeshian J, et al.: Prenatal and perinatal risk factors for autism. J Perinat Med 1999, 27:441–450.
Juul-Dam N, Townsend J, Courchesne E: Prenatal, perinatal, and neonatal factors in autism, pervasive developmental disorder-not otherwise specified, and the general population. Pediatrics 2001, 107:E63.
Deb S, Prasad KB, Seth H, et al.: A comparison of obstetric and neonatal complications between children with autistic disorder and their siblings. J Intellect Disabil Res 1997, 41:81–86.
Sprich-Buckminster S, Biederman J, Milberger S, et al.: Are perinatal complications relevant to the manifestation of ADD? Issues of comorbidity and familiality. J Am Acad Child Adolesc Psychiatry 1993, 32:1032–1037.
Milberger S, Biederman J, Faraone SV, et al.: Pregnancy, delivery and infancy complications and attention deficit hyperactivity disorder: issues of gene-environment interaction. Biol Psychiatry 1997, 41:65–75.
Mick E, Biederman J, Prince J, et al.: Impact of low birth weight on attention-deficit hyperactivity disorder. J Dev Behav Pediatr 2002, 23:16–22.
Brown A, Susser E: In utero infection and adult schizophrenia. Ment Retard Dev Disabil Res Rev 2002, 8:51–57. An interesting review of the epidemiologic evidence regarding the link between prenatal exposure to viruses and psychosis.
Cannon M, Cotter D, Coffey VP, et al.: Prenatal exposure to the 1957 influenza epidemic and adult schizophrenia: a followup study. Br J Psychiatry 1996, 168:368–371.
Morgan V, Castle D, Page A, et al.: Influenza epidemics and incidence of schizophrenia, affective disorders and mental retardation in Western Australia: no evidence of a major effect. Schizophr Res 1997, 26:25–39.
Brown A, Cohen P, Greenwald S, et al.: Nonaffective psychosis after prenatal exposure to rubella. Am J Psychiatry 2000, 157:438–443.
Chess S: Follow-up report on autism in congenital rubella. J Autism Child Schizophr 1977, 7:69–81.
Madsen KM, Hviid A, Vestergaard M, et al.: A population-based study of measles, mumps, and rubella vaccination and autism. N Engl J Med 2002, 347:1477–1482.
DeStefano F, Thompson W: MMR vaccination and autism: is there a link? Expert Opin Drug Saf 2002, 1:115–120.
Suvisaari J, Haukka J, Tanskanen A, et al.: Association between prenatal exposure to poliovirus infection and adult schizophrenia. Am J Psychiatry 1999, 156:1100–1102.
Cahill M, Chant D, Welham J, et al.: No significant association between prenatal exposure poliovirus epidemics and psychosis. Aust N Z J Psychiatry 2002, 36:373–375.
Buka SL, Tsuang MT, Torrey EF, et al.: Maternal infections and subsequent psychosis among offspring. Arch Gen Psychiatry 2001, 58:1032–1037.
Susser E, Neugebauer R, Hoeck H, et al.: Schizophrenia after prenatal famine: further evidence. Arch Gen Psychiatry 1996, 53:25–31.
Hoek HW, Susser E, Buck KA, et al.: Schizoid personality disorder after prenatal exposure to famine. Am J Psychiatry 1996, 153:1637–1639.
Neugebauer R, Hoeck H, Susser E: Prenatal exposure to wartime famine and development of antisocial personality disorder in early adulthood. JAMA 1999, 282:455–462.
Brown AS, van Os J, Driessens C, et al.: Further evidence of relation between prenatal famine and major affective disorder. Am J Psychiatry 2000, 157:190–195.
McGrath J: Hypothesis: is low prenatal vitamin D a risk-modifying factor for schizophrenia? Schizophr Res 1999, 21:173–177.
Walker A, Rosenberg M, Balaban-Gil K: Neurodevelopmental and neurobehavioral sequelae of selected substances of abuse and psychiatric medications in utero. Child Adolesc Psychiatr Clin North Am 1999, 4:845–867.
Sorensen HJ, Mortensen EL, Reinisch JM, et al.: Do hypertension and diuretic treatment in pregnancy increase the risk of schizophrenia in offspring? Am J Psychiatry 2003, 160:464–468.
Linnet KM, Dalsgaard S, Obel C, et al.: Maternal lifestyle factors in pregnancy risk of attention deficit hyperactivity disorder and associated behaviors: review of the current evidence. Am J Psychiatry 2003, 160:1028–1040.
Wakschlag LS, Pickett KE, Cook E, Jr., et al.: Maternal smoking during pregnancy and severe antisocial behavior in offspring: a review. Am J Public Health 2002, 92:966–974. A review on the behavioral consequences of maternal smoking.
Hultman CM, Sparen P, Cnattingius S: Perinatal risk factors for infantile autism. Epidemiology 2002, 13:417–423. A population-based study on the early risk factors for autism.
Verdoux H, Sutter AL: Obstetric complications, maternal psychopathology, and the risk of psychosis. In Obstetric Complications, Maternal Psychopathology, and the Risk of Psychosis. Edited by Häfner H. Berlin: Steinkopff Verlag Darmasdt; 2002:105–112.
Huttunen M, Niskanen P: Prenatal loss of father and psychiatric disorders. Arch Gen Psychiatry 1978, 35:429–431.
van Os J, Selten JP: Prenatal exposure to maternal stress and subsequent schizophrenia. Br J Psychiatry 1998, 172:324–326.
Selten J, Cantor-Graae E, Nahon D, et al.: No relationship between risk of schizophrenia and prenatal exposure to stress during the Six-Day War or Yom Kippur War in Israel. Schizophr Res 2003, 63:131–135.
Selten J, van der Graaf Y, van Duursen R, et al.: Psychotic illness after prenatal exposure to the 1953 Dutch flood disaster. Schizophr Res 1999, 35:243–245.
Myrham A, Rantakallio P, Isohanni M, et al.: Unwantdness of a pregnancy and schizophrenia in the child. Br J Psychiatry 1996, 169:637–640.
Malaspina D, Harlap S, Fennig S, et al.: Advancing paternal age and the risk of schizophrenia. Arch Gen Psychiatry 2001, 58:361–367.
Brown AS, Schaefer CA, Wyatt RJ, et al.: Paternal age and risk of schizophrenia in adult offspring. Am J Psychiatry 2002, 159:1528–1533.
Dalman C, Allebeck P: Paternal age and schizophrenia: further support for an association. Am J Psychiatry 2002, 159:1591–1592.
Byrne M, Agerbo E, Ewald H, et al.: Parental age and risk of schizophrenia: a case-control study. Arch Gen Psychiatry 2003, 60:673–678.
Pasamanick B, Rogers M, Lilienfeld A: Pregnancy experience and the development of behavior disorder in children. Am J Psychiatry 1956, 112:613–618.
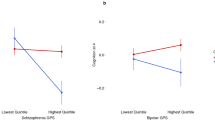
Walker J, Curtis V, Shaw P, et al.: Schizophrenia and bipolar disorder are distinguished mainly by differences in neurodevelopment. Neurotox Res 2002, 4:427–436.
Verdoux H, van Os J: Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophr Res 2002, 54:59–65.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Verdoux, H. Perinatal risk factors for schizophrenia: How specific are they?. Curr Psychiatry Rep 6, 162–167 (2004). https://doi.org/10.1007/s11920-004-0060-6
Issue Date:
DOI: https://doi.org/10.1007/s11920-004-0060-6