Abstract
Purpose of Review
Despite the unmet therapeutic needs of patients with chronic migraine (CM) and/or medication overuse, available treatment options are limited. Recently, four calcitonin gene-related peptide receptor antagonists, known as gepants, have been approved for the treatment of migraine. This review focuses on the preventive treatment of CM with gepants and highlights recent findings.
Recent Findings
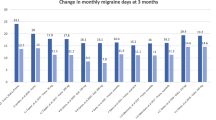
Two randomized controlled trials (RCTs) have shown promising results for rimegepant and atogepant as preventive treatments for CM. In an RCT targeting patients with CM, atogepant demonstrated a significant reduction in the mean monthly migraine days, irrespective of acute medication overuse. Moreover, the patients reported no significant safety concerns and exhibited good tolerance to treatment.
Summary
These findings highlight the potential of gepants as a new and effective therapeutic option for patients with CM and/or medication overuse. Gepant use will help improve the management and quality of life of individuals with this debilitating condition.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Arnold M. Headache classification committee of the international headache society (IHS) the international classification of headache disorders. Cephalalgia. 2018;38(1):1–211.
Natoli J, Manack A, Dean B, Butler Q, Turkel C, Stovner L, et al. Global prevalence of chronic migraine: a systematic review. Cephalalgia. 2010;30(5):599–609.
Lipton RB. Tracing transformation: chronic migraine classification, progression, and epidemiology. Neurology. 2009;72(5 Supplement 1):S3–7.
Bigal ME, Lipton RB. Modifiable risk factors for migraine progression. Headache. 2006;46(9):1334–43.
Bigal ME, Serrano D, Buse D, Scher A, Stewart WF, Lipton RB. Acute migraine medications and evolution from episodic to chronic migraine: A longitudinal population-based study. Headache. 2008;48(8):1157–68.
Manack AN, Buse DC, Lipton RB. Chronic migraine: epidemiology and disease burden. Curr Pain Headache Rep. 2011;15:70–8.
Adams AM, Serrano D, Buse DC, Reed ML, Marske V, Fanning KM, et al. The impact of chronic migraine: The Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia. 2015;35(7):563–78.
Hepp Z, Dodick DW, Varon SF, Gillard P, Hansen RN, Devine EB. Adherence to oral migraine-preventive medications among patients with chronic migraine. Cephalalgia. 2014;35(6):478–88.
Straube A, Pfaffenrath V, Ladwig KH, Meisinger C, Hoffmann W, Fendrich K, et al. Prevalence of chronic migraine and medication overuse headache in Germany–the German DMKG headache study. Cephalalgia. 2010;30(2):207–13.
Diener HC, Bussone G, Oene JCV, Lahaye M, Schwalen S, Goadsby PJ. Topiramate reduces headache days in chronic migraine: a randomized, double-blind, placebo-controlled study. Cephalalgia. 2007;27(7):814–23.
Silberstein SD, Blumenfeld AM, Cady RK, Turner IM, Lipton RB, Diener H-C, et al. OnabotulinumtoxinA for treatment of chronic migraine: PREEMPT 24-week pooled subgroup analysis of patients who had acute headache medication overuse at baseline. J Neurol Sci. 2013;331(1):48–56.
Diener H-C, Limmroth V. Medication-overuse headache: a worldwide problem. Lancet Neurol. 2004;3(8):475–83.
Carlsen LN, Munksgaard SB, Jensen RH, Bendtsen L. Complete detoxification is the most effective treatment of medication-overuse headache: a randomized controlled open-label trial. Cephalalgia. 2018;38(2):225–36.
Ferrari MD, Diener HC, Ning X, Galic M, Cohen JM, Yang R, et al. Fremanezumab versus placebo for migraine prevention in patients with documented failure to up to four migraine preventive medication classes (FOCUS): a randomised, double-blind, placebo-controlled, phase 3b trial. Lancet. 2019;394(10203):1030–40.
Mulleners WM, Kim BK, Láinez MJA, Lanteri-Minet M, Pozo-Rosich P, Wang S, et al. Safety and efficacy of galcanezumab in patients for whom previous migraine preventive medication from two to four categories had failed (CONQUER): a multicentre, randomised, double-blind, placebo-controlled, phase 3b trial. Lancet Neurol. 2020;19(10):814–25.
Ashina M, Lanteri-Minet M, Pozo-Rosich P, Ettrup A, Christoffersen CL, Josiassen MK, et al. Safety and efficacy of eptinezumab for migraine prevention in patients with two-to-four previous preventive treatment failures (DELIVER): a multi-arm, randomised, double-blind, placebo-controlled, phase 3b trial. Lancet Neurol. 2022;21(7):597–607.
Ashina M, Amin FM, Kokturk P, Cohen JM, Konings M, Tassorelli C, et al. PEARL study protocol: a real-world study of fremanezumab effectiveness in patients with chronic or episodic migraine. Pain Manag. 2021;11(6):647–54.
Lee HC, Cho S, Kim BK. Predictors of response to galcanezumab in patients with chronic migraine: a real-world prospective observational study. Neurol Sci. 2023;44:2455–63.
Reuter U, Goadsby PJ, Lanteri-Minet M, Wen S, Hours-Zesiger P, Ferrari MD, et al. Efficacy and tolerability of erenumab in patients with episodic migraine in whom two-to-four previous preventive treatments were unsuccessful: a randomised, double-blind, placebo-controlled, phase 3b study. Lancet. 2018;392(10161):2280–7.
Goadsby P, Edvinsson L, Ekman R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann Neurol. 1990;28(2):183–7.
Goadsby PJ, Edvinsson L. The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann Neurol. 1993;33(1):48–56.
Lassen L, Haderslev P, Jacobsen V, Iversen H, Sperling B, Olesen J. CGRP may play a causative role in migraine. Cephalalgia. 2002;22(1):54–61.
Olesen J, Diener H-C, Husstedt IW, Goadsby PJ, Hall D, Meier U, et al. Calcitonin gene–related peptide receptor antagonist BIBN 4096 BS for the acute treatment of migraine. N Engl J Med. 2004;350(11):1104–10.
Connor K, Shapiro R, Diener H-C, Lucas S, Kost J, Fan X, et al. Randomized, controlled trial of telcagepant for the acute treatment of migraine. Neurology. 2009;73(12):970–7.
Connor KM, Aurora SK, Loeys T, Ashina M, Jones C, Giezek H, et al. Long-term tolerability of telcagepant for acute treatment of migraine in a randomized trial. Headache. 2011;51(1):73–84.
Behm MO, Blanchard RL, Murphy MG, Palcza JS, Harris DE, Butterfield KL, et al. Effect of telcagepant on spontaneous ischemia in cardiovascular patients in a randomized study. Headache. 2011;51(6):954–60.
Ho TW, Connor KM, Zhang Y, Pearlman E, Koppenhaver J, Fan X, et al. Randomized controlled trial of the CGRP receptor antagonist telcagepant for migraine prevention. Neurology. 2014;83(11):958–66.
Ho TW, Ho AP, Ge Y, Assaid C, Gottwald R, MacGregor EA, et al. Randomized controlled trial of the CGRP receptor antagonist telcagepant for prevention of headache in women with perimenstrual migraine. Cephalalgia. 2016;36(2):148–61.
Diener H-C, Barbanti P, Dahlöf C, Reuter U, Habeck J, Podhorna J. BI 44370 TA, an oral CGRP antagonist for the treatment of acute migraine attacks: results from a phase II study. Cephalalgia. 2011;31(5):573–84.
Hewitt DJ, Aurora SK, Dodick DW, Goadsby PJ, Ge Y, Bachman R, et al. Randomized controlled trial of the CGRP receptor antagonist MK-3207 in the acute treatment of migraine. Cephalalgia. 2011;31(6):712–22.
Marcus R, Goadsby PJ, Dodick D, Stock D, Manos G, Fischer TZ. BMS-927711 for the acute treatment of migraine: a double-blind, randomized, placebo controlled, dose-ranging trial. Cephalalgia. 2014;34(2):114–25.
Croop R, Goadsby PJ, Stock DA, Conway CM, Forshaw M, Stock EG, et al. Efficacy, safety, and tolerability of rimegepant orally disintegrating tablet for the acute treatment of migraine: a randomised, phase 3, double-blind, placebo-controlled trial. Lancet. 2019;394(10200):737–45.
Lipton RB, Croop R, Stock EG, Stock DA, Morris BA, Frost M, et al. Rimegepant, an oral calcitonin gene-related peptide receptor antagonist, for migraine. N Engl J Med. 2019;381(2):142–9.
•• Croop R, Lipton RB, Kudrow D, Stock DA, Kamen L, Conway CM, et al. Oral rimegepant for preventive treatment of migraine: a phase 2/3, randomised, double-blind, placebo-controlled trial. Lancet. 2021;397(10268):51–60. RCT of rimegepant for preventive treatment of migraine.
Voss T, Lipton RB, Dodick DW, Dupre N, Ge JY, Bachman R, et al. A phase IIb randomized, double-blind, placebo-controlled trial of ubrogepant for the acute treatment of migraine. Cephalalgia. 2016;36(9):887–98.
Dodick DW, Lipton RB, Ailani J, Lu K, Finnegan M, Trugman JM, et al. Ubrogepant for the treatment of migraine. N Engl J Med. 2019;381(23):2230–41.
Lipton RB, Dodick DW, Ailani J, Lu K, Finnegan M, Szegedi A, et al. Effect of ubrogepant vs placebo on pain and the most bothersome associated symptom in the acute treatment of migraine: the ACHIEVE II randomized clinical trial. JAMA. 2019;322(19):1887–98.
•• Goadsby PJ, Dodick DW, Ailani J, Trugman JM, Finnegan M, Lu K, et al. Safety, tolerability, and efficacy of orally administered atogepant for the prevention of episodic migraine in adults: a double-blind, randomised phase 2b/3 trial. Lancet Neurol. 2020;19(9):727–37. RCT of atogepant for preventive treatment of EM.
•• Ailani J, Lipton RB, Goadsby PJ, Guo H, Miceli R, Severt L, et al. Atogepant for the preventive treatment of migraine. N Engl J Med. 2021;385(8):695–706. RCT of atogepant for preventive treatment of EM.
•• Pozo-Rosich P, Ailani J, Ashina M, Goadsby PJ, Lipton RB, Reuter U, et al. Atogepant for the preventive treatment of chronic migraine (PROGRESS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2023. RCT of atogepant for preventive treatment of CM.
Lipton RB, Croop R, Stock DA, Madonia J, Forshaw M, Lovegren M, et al. Safety, tolerability, and efficacy of zavegepant 10 mg nasal spray for the acute treatment of migraine in the USA: a phase 3, double-blind, randomised, placebo-controlled multicentre trial. Lancet Neurol. 2023;22(3):209–17.
Durham PL. CGRP-Receptor Antagonists — A Fresh Approach to Migraine Therapy? N Engl J Med. 2004;350(11):1073–5.
Bell IM. Calcitonin gene-related peptide receptor antagonists: new therapeutic agents for migraine. J Med Chem. 2014;57(19):7838–58.
Durham PL, Vause CV. Calcitonin gene-related peptide (CGRP) receptor antagonists in the treatment of migraine. CNS Drugs. 2010;24(7):539–48.
Walker CS, Raddant AC, Woolley MJ, Russo AF, Hay DL. CGRP receptor antagonist activity of olcegepant depends on the signalling pathway measured. Cephalalgia. 2018;38(3):437–51.
MaassenVanDenBrink A, Reekers M, Bax WA, Ferrari MD, Saxena PR. Coronary side-effect potential of current and prospective antimigraine drugs. Circulation. 1998;98(1):25–30.
Böhm SK, Grady EF, Bunnett NW. Regulatory mechanisms that modulate signalling by G-protein-coupled receptors. Biochem J. 1997;322(1):1–18.
• Navratilova E, Behravesh S, Oyarzo J, Dodick DW, Banerjee P, Porreca F. Ubrogepant does not induce latent sensitization in a preclinical model of medication overuse headache. Cephalalgia. 2020;40(9):892–902. Preclinical evidence supporting that gepants may not cause MOH.
Saengjaroentham C, Strother LC, Dripps I, Sultan Jabir MR, Pradhan A, Goadsby PJ, et al. Differential medication overuse risk of novel anti-migraine therapeutics. Brain. 2020;143(9):2681–8.
Holland PR, Saengjaroentham C, Sureda-Gibert P, Strother LC. Medication overuse headache: Divergent effects of new acute antimigraine drugs. Cephalalgia. 2020;40(9):889–91.
Goadsby PJ, Tepper SJ, Watkins PB, Ayele G, Miceli R, Butler M, et al. Safety and tolerability of ubrogepant following intermittent, high-frequency dosing: randomized, placebo-controlled trial in healthy adults. Cephalalgia. 2019;39(14):1753–61.
Tepper SJ, Diener H-C, Ashina M, Brandes JL, Friedman DI, Reuter U, et al. Erenumab in chronic migraine with medication overuse: subgroup analysis of a randomized trial. Neurology. 2019;92(20):e2309–20.
Yu S, Kim B-K, Guo A, Kim M-H, Zhang M, Wang Z, et al. Safety and efficacy of rimegepant orally disintegrating tablet for the acute treatment of migraine in China and South Korea: a phase 3, double-blind, randomised, placebo-controlled trial. Lancet Neurol. 2023;22(6):476–84.
Ashina M, Tepper SJ, Reuter U, Blumenfeld AM, Hutchinson S, Xia J, et al. Once-daily oral atogepant for the long-term preventive treatment of migraine: Findings from a multicenter, randomized, open-label, phase 3 trial. Headache. 2023;63(1):79–88.
Klein BC, Miceli R, Severt L, McAllister P, Mechtler L, McVige J, et al. Safety and tolerability results of atogepant for the preventive treatment of episodic migraine from a 40-week, open-label multicenter extension of the phase 3 ADVANCE trial. Cephalalgia. 2023;43(1):3331024221128250.
Boinpally R, McNamee B, Yao L, Butler M, McGeeney D, Borbridge L, et al. A single supratherapeutic dose of atogepant does not affect cardiac repolarization in healthy adults: results from a randomized, single-dose, phase 1 crossover trial. Clin Pharmacol Drug Dev. 2021;10(9):1099–107.
Holzer P, Holzer-Petsche U. Constipation caused by anti-calcitonin gene-related peptide migraine therapeutics explained by antagonism of calcitonin gene-related peptide’s motor-stimulating and prosecretory function in the intestine. Front Physiol. 2022;12:820006.
Johnson KW, Li X, Huang X, Heinz BA, Yu J, Li B. Characterization of transit rates in the large intestine of mice following treatment with a CGRP antibody, CGRP receptor antibody, and small molecule CGRP receptor antagonists. Headache. 2022;62(7):848–57.
Ruiz M, Cocores A, Tosti A, Goadsby PJ, Monteith TS. Alopecia as an emerging adverse event to CGRP monoclonal antibodies: Cases Series, evaluation of FAERS, and literature review. Cephalalgia. 2023;43(2):03331024221143538.
Melo-Carrillo A, Strassman AM, Schain AJ, Adams AM, Brin MF, Burstein R. Combined onabotulinumtoxinA/atogepant treatment blocks activation/sensitization of high-threshold and wide-dynamic range neurons. Cephalalgia. 2021;41(1):17–32.
Boinpally R, Jakate A, Butler M, Periclou A. Atogepant and sumatriptan: no clinically relevant drug–drug interactions in a randomized, open-label, crossover trial. Pain Manag. 2021;12(4):499–508.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Soohyun Cho received honoraria as a speaker from Celltrion Pharm, Daewoong Pharm, Boryung, Whan In Pharm, Teva and SK Pharm. He has been the principal investigator of clinical trials sponsored by Teva and SK Pharm. Byung-Kun Kim served on Lundbeck’s Advisory Board. He received honoraria as a moderator and speaker from Lundbeck, AbbVie, Pfizer, Eli Lilly, Teva, Yuyu Pharm, and SK Pharm. He has been the principal investigator of clinical trials sponsored by Eli-Lilly, Novartis, Lundbeck, Teva, AbbVie, and Ildong Pharm.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cho, S., Kim, BK. Update of Gepants in the Treatment of Chronic Migraine. Curr Pain Headache Rep 27, 561–569 (2023). https://doi.org/10.1007/s11916-023-01167-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11916-023-01167-6