Abstract
Purpose of review
To discuss current knowledge on the role of connexins and pannexins in the musculoskeletal system.
Recent findings
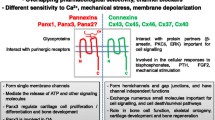
Connexins and pannexins are crucial for the development and maintenance of both bone and skeletal muscle. In bone, the presence of connexin and more recently of pannexin channels in osteoblasts, osteoclasts, and osteocytes has been described and shown to be essential for normal skeletal development and bone adaptation. In skeletal muscles, connexins and pannexins play important roles during development and regeneration through coordinated regulation of metabolic functions via cell-to-cell communication. Further, under pathological conditions, altered expression of these proteins can promote muscle atrophy and degeneration by stimulating inflammasome activity.
Summary
In this review, we highlight the important roles of connexins and pannexins in the development, maintenance, and regeneration of musculoskeletal tissues, with emphasis on the mechanisms by which these molecules mediate chemical (e.g., ATP and prostaglandin E2) and physical (e.g., mechanical stimulation) stimuli that target the musculoskeletal system and their involvement in the pathophysiological changes in both genetic and acquired diseases.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Plotkin LI, Stains JP. Connexins and pannexins in the skeleton: gap junctions, hemichannels and more. Cell Mol Life Sci. 2015;72:2853–67. doi:10.1007/s00018-015-1963-6.
Goodenough DA, Paul DL. Beyond the gap: functions of unpaired connexon channels. Nat Rev Mol Cell Biol. 2003;4:285–94. doi:10.1038/nrm1072.
Plotkin LI, Laird DW, Amedee J. Role of connexins and pannexins during ontogeny, regeneration, and pathologies of bone. BMC Cell Biol. 2016;17:29–38. doi:10.1186/s12860-016-0088-6.
Penuela S, Harland L, Simek J, et al. Pannexin channels and their links to human disease. Biochem J. 2014;461:371–81. doi:10.1042/BJ20140447.
Sosinsky GE, Boassa D, Dermietzel R, et al. Pannexin channels are not gap junction hemichannels. Channels (Austin). 2011;5:193–7. doi:10.4161/chan.5.3.15765.
Sáez JC, Cisterna BA, Vargas A, et al. Regulation of pannexin and connexin channels and their functional role in skeletal muscles. Cell Mol Life Sci. 2015;72:2929–35. doi:10.1007/s00018-015-1968-1.
Delgado-Calle J, Bellido T. Osteocytes and skeletal pathophysiology. Curr Mol Biol Rep. 2015;1:157–67. doi:10.1007/s40610-015-0026-y.
Weinger JM, Holtrop ME. An ultrastructural study of bone cells: the occurrence of microtubules, microfilaments and tight junctions. Calcif Tissue Res. 1974;14:15–29.
Civitelli R, Beyer EC, Warlow PM, et al. Connexin43 mediates direct intercellular communication in human osteoblastic cell networks. J Clin Invest. 1993;91:1888–96. doi:10.1172/JCI116406.
Ilvesaro J, Väänänen K, Tuukkanen J. Bone-resorbing osteoclasts contain gap-junctional connexin-43. J Bone Min Res. 2000;15:919–26. doi:10.1359/jbmr.2000.15.5.919.
Yellowley CE, Li Z, Zhou Z, et al. Functional gap junctions between osteocytic and osteoblastic cells. J Bone Miner Res. 2000;15:209–17. doi:10.1359/jbmr.2000.15.2.209.
Lecanda F, Towler DA, Ziambaras K, et al. Gap junctional communication modulates gene expression in osteoblastic cells. Mol Biol Cell. 1998;9:2249–58. doi:10.1091/mbc.9.8.2249.
Lecanda F, Warlow PM, Sheikh S, et al. Connexin43 deficiency causes delayed ossification, craniofacial abnormalities, and osteoblast dysfunction. J Cell Biol. 2000;151:931–44. doi:10.1083/jcb.151.4.931.
Thi MM, Urban-Maldonado M, Spray DC, et al. Characterization of human telomerase reverse transcriptase (hTERT) immortalized osteoblast cell lines generated from wildtype and connexin43-null mouse calvaria. Am J Physiol Cell Physiol. 2010;299:C994–C1006. doi:10.1152/ajpcell.00544.2009.
Reaume AG, de Sousa PA, Kulkarni S, et al. Cardiac malformation in neonatal mice lacking connexin43. Science. 1995;267:1831–4. doi:10.1126/science.7892609.
Gonzalez-Nieto D, Li L, Kohler A, et al. Connexin-43 in the osteogenic BM niche regulates its cellular composition and the bidirectional traffic of hematopoietic stem cells and progenitors. Blood. 2012;119:5144–54. doi:10.1182/blood-2011-07-368506.
Watkins M, Grimston SK, Norris JY, et al. Osteoblast connexin43 modulates skeletal architecture by regulating both arms of bone remodeling. Mol Biol Cell. 2011;22:1240–51. doi:10.1091/mbc.E10-07-0571.
Chung D, Castro CH, Watkins M, et al. Low peak bone mass and attenuated anabolic response to parathyroid hormone in mice with an osteoblast-specific deletion of connexin43. J Cell Sci. 2006;119:4187–98. doi:10.1242/jcs.03162.
Plotkin LI, Lezcano V, Thostenson J, et al. Connexin 43 is required for the anti-apoptotic effect of bisphosphonates on osteocytes and osteoblasts in vivo. J Bone Miner Res. 2008;23:1712–21. doi:10.1359/jbmr.080617.
Zhang Y, Paul EM, Sathyendra V, et al. Enhanced osteoclastic resorption and responsiveness to mechanical load in gap junction deficient bone. PLoS ONE. 2011;6:e23516. doi:10.1371/journal.pone.0023516.
Bivi N, Condon KW, Allen MR, et al. Cell autonomous requirement of connexin 43 for osteocyte survival: consequences for endocortical resorption and periosteal bone formation. J Bone Miner Res. 2012;27:374–89. doi:10.1002/jbmr.548.
• Shen H, Grimston S, Civitelli R, et al. Deletion of connexin43 in osteoblasts/osteocytes leads to impaired muscle formation in mice. J Bone Miner Res. 2014;30:596–605. doi:10.1002/jbmr.2389. First demonstration of the role of osteoblastic Cx43 on skeletal muscle formation.
Kruger O, Plum A, Kim JS, et al. Defective vascular development in connexin 45-deficient mice. Development. 2000;127:4179–93.
Chaible LM, Sanches DS, Cogliati B, et al. Delayed osteoblastic differentiation and bone development in Cx43 knockout mice. Toxicol Pathol. 2011;39:1046–55. doi:10.1177/0192623311422075.
Stains JP, Civitelli R. Gap junctions in skeletal development and function. Biochim Biophys Acta. 2005;1719:69–81. doi:10.1016/j.bbamem.2005.10.012.
Paic F, Igwe JC, Nori R, et al. Identification of differentially expressed genes between osteoblasts and osteocytes. Bone. 2009;45:682–92. doi:10.1016/j.bone.2009.06.010.
Pacheco-Costa R, Hassan I, Reginato RD, et al. High bone mass in mice lacking Cx37 due to defective osteoclast differentiation. J Biol Chem. 2014;289:8508–20. doi:10.1074/jbc.M113.529735.
Pacheco-Costa R, Kadakia JR, Atkinson EG, et al. Connexin37 deficiency alters organic bone matrix, cortical bone geometry, and increases Wnt/beta-catenin signaling. Bone. 2017;97:105–13. doi:10.1016/j.bone.2017.01.010.
Loiselle AE, Paul EM, Lewis GS, et al. Osteoblast and osteocyte-specific loss of Connexin43 results in delayed bone formation and healing during murine fracture healing. J Orthop Res. 2013;31:147–54. doi:10.1002/jor.22178.
Maass K, Ghanem A, Kim JS, et al. Defective epidermal barrier in neonatal mice lacking the C-terminal region of connexin43. Mol Biol Cell. 2004;15:4597–608. doi:10.1091/mbc.E04-04-0324.
Pacheco-Costa R, Davis HM, Sorenson C, et al. Defective cancellous bone structure and abnormal response to PTH in cortical bone of mice lacking Cx43 cytoplasmic C-terminus domain. Bone. 2015;81:632–43. doi:10.1016/j.bone.2015.09.011.
Moorer MC, Hebert C, Tomlinson RE, et al. Defective signaling, osteoblastogenesis, and bone remodeling in a mouse model of connexin43 C-terminal truncation. J Cell Sci. 2017;130:531–40. doi:10.1242/jcs.197285.
Bond SR, Lau A, Penuela S, et al. Pannexin 3 is a novel target for Runx2, expressed by osteoblasts and mature growth plate chondrocytes. J Bone Miner Res. 2011;26:2911–22. doi:10.1002/jbmr.509.
Xiao Z, Camalier CE, Nagashima K, et al. Analysis of the extracellular matrix vesicle proteome in mineralizing osteoblasts. J Cell Physiol. 2007;210:325–35. doi:10.1002/jcp.20826.
Cheung WY, Fritton JC, Morgan SA, et al. Pannexin-1 and P2X7-receptor are required for apoptotic osteocytes in fatigued bone to trigger RANKL production in neighboring bystander osteocytes. J Bone Miner Res. 2016;31:890–9. doi:10.1002/jbmr.2740.
Caskenette D, Penuela S, Lee V, et al. Global deletion of Panx3 produces multiple phenotypic effects in mouse humeri and femora. J. Anat. 2016; 28(5):746–56. doi:10.1111/joa.12437.
Genetos DC, Zhou Z, Li Z, et al. Age-related changes in gap junctional intercellular communication in osteoblastic cells. J Orthop Res. 2012;30:1979–84. doi:10.1002/jor.22172.
•• Davis HM, Pacheco-Costa R, Atkinson EG, et al. Disruption of the Cx43/miR21 pathway leads to osteocyte apoptosis and increased osteoclastogenesis with aging. Aging Cell. 2017; doi:10.1111/acel.12586. This study describes for the first time the molecular signaling pathways that lead to osteocyte apoptosis and osteoclast recruitment in the absence of Cx43 and with aging.
Kar R, Riquelme MA, Werner S, et al. Connexin 43 channels protect osteocytes against oxidative stress-induced cell death. J Bone Miner Res. 2013;28:1611–21. doi:10.1002/jbmr.1917.
Almeida M, Han L, Martin-Millan M, et al. Skeletal involution by age-associated oxidative stress and its acceleration by loss of sex steroids. J Biol Chem. 2007;282:27285–97. doi:10.1074/jbc.M702810200.
Paznekas WA, Boyadjiev SA, Shapiro RE, et al. Connexin 43 (GJA1) mutations cause the pleiotropic phenotype of oculodentodigital dysplasia. Am J Hum Genet. 2003;72:408–18. doi:10.1086/346090.
Alao MJ, Bonneau D, Holder-Espinasse M, et al. Oculo-dento-digital dysplasia: lack of genotype-phenotype correlation for GJA1 mutations and usefulness of neuro-imaging. Eur J Med Genet. 2010;53:19–22. doi:10.1016/j.ejmg.2009.08.007.
Brice G, Ostergaard P, Jeffery S, et al. A novel mutation in GJA1 causing oculodentodigital syndrome and primary lymphoedema in a three generation family. Clin Genet. 2013;84:378–81. doi:10.1111/cge.12158.
Himi M, Fujimaki T, Yokoyama T, et al. A case of oculodentodigital dysplasia syndrome with novel GJA1 gene mutation. Jpn J Ophthalmol. 2009;53:541–5. doi:10.1007/s10384-009-0711-6.
Gabriel LA, Sachdeva R, Marcotty A, et al. Oculodentodigital dysplasia: new ocular findings and a novel connexin 43 mutation. Arch Ophthalmol. 2011;129:781–4. doi:10.1001/archophthalmol.2011.113.
Furuta N, Ikeda M, Hirayanagi K, et al. A novel GJA1 mutation in oculodentodigital dysplasia with progressive spastic paraplegia and sensory deficits. Intern Med. 2012;51:93–8. doi:10.2169/internalmedicine.51.5770.
Fenwick A, Richardson RJ, Butterworth J, et al. Novel mutations in GJA1 cause oculodentodigital syndrome. J Dent Res. 2008;87:1021–6. doi:10.1177/154405910808701108.
Debeer P, Van EH, Huysmans C, et al. Novel GJA1 mutations in patients with oculo-dento-digital dysplasia (ODDD). Eur J Med Genet 2005;48:377–87. doi:10.1016/j.ejmg.2005.05.003.
de la Parra DR, Zenteno JC. A new GJA1 (connexin 43) mutation causing oculodentodigital dysplasia associated to uncommon features. Ophthalmic Genet. 2007;28:198–202. doi:10.1080/13816810701538620.
Kjaer KW, Hansen L, Eiberg H, et al. Novel connexin 43 (GJA1) mutation causes oculo-dento-digital dysplasia with curly hair. Am. J. Med. Genet. A. 2004;127:152–57. doi:10.1002/ajmg.a.20614.
Itro A, Marra A, Urciuolo V, et al. Oculodentodigital dysplasia. A case report. Minerva Stomatol. 2005;54:453–9.
Izumi K, Lippa AM, Wilkens A, et al. Congenital heart defects in oculodentodigital dysplasia: Report of two cases. Am J Med Genet A. 2013;161:3150–4. doi:10.1002/ajmg.a.36159.
Jamsheer A, Sowinska-Seidler A, Socha M, et al. Three novel GJA1 missense substitutions resulting in oculo-dento-digital dysplasia (ODDD)—further extension of the mutational spectrum. Gene. 2014;539:157–61. doi:10.1016/j.gene.2014.01.066.
Jamsheer A, Wisniewska M, Szpak A, et al. A novel GJA1 missense mutation in a Polish child with oculodentodigital dysplasia. J Appl Genet. 2009;50:297–9. doi:10.1007/BF03195687.
Joss SK, Ghazawy S, Tomkins S, et al. Variable expression of neurological phenotype in autosomal recessive oculodentodigital dysplasia of two sibs and review of the literature. Eur J Pediatr. 2008;167:341–5. doi:10.1007/s00431-007-0468-1.
Kellermayer R, Keller M, Ratajczak P, et al. Bigenic connexin mutations in a patient with hidrotic ectodermal dysplasia. Eur J Dermatol. 2005;15:75–9.
Kelly SC, Ratajczak P, Keller M, et al. A novel GJA 1 mutation in oculo-dento-digital dysplasia with curly hair and hyperkeratosis. Eur J Dermatol. 2006;16:241–5.
Laird DW. Syndromic and non-syndromic disease-linked Cx43 mutations. FEBS Lett. 2014;588:1339–48. doi:10.1016/j.febslet.2013.12.022.
Paznekas WA, Karczeski B, Vermeer S, et al. GJA1 mutations, variants, and connexin 43 dysfunction as it relates to the oculodentodigital dysplasia phenotype. Hum Mutat. 2009;30:724–33. doi:10.1002/humu.20958.
Honkaniemi J, Kalkkila JP, Koivisto P, et al. Letter to the editor: Novel GJA1 mutation in oculodentodigital dysplasia. Am J Med Genet A. 2005;139:48–9. doi:10.1002/ajmg.a.30925.
Pizzuti A, Flex E, Mingarelli R, et al. A homozygous GJA1 gene mutation causes a Hallermann-Streiff/ODDD spectrum phenotype. Hum Mutat. 2004;23:286. doi:10.1002/humu.9220.
Richardson R, Donnai D, Meire F, et al. Expression of Gja1 correlates with the phenotype observed in oculodentodigital syndrome/type III syndactyly. J Med Genet. 2004;41:60–7. doi:10.1136/jmg.2003.012005.
van Steensel MA, Spruijt L, van der Burgt I, et al. A 2-bp deletion in the GJA1 gene is associated with oculo-dento-digital dysplasia with palmoplantar keratoderma. Am J Med Genet A. 2005;132A:171–4. doi:10.1002/ajmg.a.30412.
Vasconcellos JP, Melo MB, Schimiti RB, et al. A novel mutation in the GJA1 gene in a family with oculodentodigital dysplasia. Arch Ophthalmol. 2005;123:1422–6. doi:10.1001/archopht.123.10.1422.
Vitiello C, D’Adamo P, Gentile F, et al. A novel GJA1 mutation causes oculodentodigital dysplasia without syndactyly. Am J Med Genet A. 2005;133A:58–60. doi:10.1002/ajmg.a.30554.
Vreeburg M, de Zwart-Storm EA, Schouten MI, et al. Skin changes in oculo-dento-digital dysplasia are correlated with C-terminal truncations of connexin 43. Am J Med Genet A. 2007;143:360–3. doi:10.1002/ajmg.a.31558.
Wiest T, Herrmann O, Stogbauer F, et al. Clinical and genetic variability of oculodentodigital dysplasia. Clin Genet. 2006;70:71–2. doi:10.1111/j.1399-0004.2006.00631.x.
Flenniken AM, Osborne LR, Anderson N, et al. A Gja1 missense mutation in a mouse model of oculodentodigital dysplasia. Development. 2005;132:4375–86. doi:10.1242/dev.02011.
Hu Y, Chen IP, de Almeida S, et al. A novel autosomal recessive GJA1 missense mutation linked to craniometaphyseal dysplasia. PLoS ONE. 2013;8:e73576. doi:10.1371/journal.pone.0073576.
Van Norstrand DW, Asimaki A, Rubinos C, et al. Connexin43 mutation causes heterogeneous gap junction loss and sudden infant death. Circulation. 2012;125:474–81. doi:10.1161/CIRCULATIONAHA.111.057224.
•• Shao Q, Lindstrom K, Shi R, et al. A germline variant in the PANX1 gene has reduced channel function and is associated with multisystem dysfunction. J Biol Chem. 2016;291:12432–43. doi:10.1074/jbc.M116.717934. The first report of a pannexin1 mutation associated with human disease.
Plotkin LI. Connexin 43 hemichannels and intracellular signaling in bone cells. Front Physiol. 2014;5:131. doi:10.3389/fphys.2014.00131.
Plotkin LI, Bellido T. Beyond gap junctions: Connexin43 and bone cell signaling. Bone. 2013;52:157–66. doi:10.1016/j.bone.2012.09.030.
Stains JP, Civitelli R. Connexins in the skeleton. Semin. Cell Dev. Biol. 2016;50:31–9. doi:10.1016/j.semcdb.2015.12.017.
Moorer MC, Stains JP. Connexin43 and the Intercellular Signaling Network Regulating Skeletal Remodeling. Curr. Osteoporos. Rep. 2017; doi:10.1007/s11914-017-0345-4.
Araya R, Riquelme MA, Brandan E, et al. The formation of skeletal muscle myotubes requires functional membrane receptors activated by extracellular ATP. Brain Res Brain Res Rev. 2004;47:174–88. doi:10.1016/j.brainresrev.2004.06.003.
von Maltzahn J, Euwens C, Willecke K, et al. The novel mouse connexin39 gene is expressed in developing striated muscle fibers. J Cell Sci. 2004;117:5381–92. doi:10.1242/jcs.01413.
Araya R, Eckardt D, Riquelme MA, et al. Presence and importance of connexin43 during myogenesis. Cell Commun Adhes. 2003;10:451–6.
Araya R, Eckardt D, Maxeiner S, et al. Expression of connexins during differentiation and regeneration of skeletal muscle: functional relevance of connexin43. J Cell Sci. 2005;118:27–37. doi:10.1242/jcs.01553.
Langlois S, Xiang X, Young K, et al. Pannexin 1 and pannexin 3 channels regulate skeletal muscle myoblast proliferation and differentiation. J. Biol. Chem. 2014;289(44): 30717–31. doi:10.1074/jbc.M114.572131.
Riquelme MA, Cea LA, Vega JL, et al. Pannexin channels mediate the acquisition of myogenic commitment in C2C12 reserve cells promoted by P2 receptor activation. Front Cell Dev Biol. 2015;3:25. doi:10.3389/fcell.2015.00025.
Buvinic S, Almarza G, Bustamante M, et al. ATP released by electrical stimuli elicits calcium transients and gene expression in skeletal muscle. J Biol Chem. 2009;284:34490–505. doi:10.1074/jbc.M109.057315.
Riquelme MA, Cea LA, Vega JL, et al. The ATP required for potentiation of skeletal muscle contraction is released via pannexin hemichannels. Neuropharmacology. 2013;75:594–603. doi:10.1016/j.neuropharm.2013.03.022.
Jorquera G, Altamirano F, Contreras-Ferrat A, et al. Cav1.1 controls frequency-dependent events regulating adult skeletal muscle plasticity. J Cell Sci. 2013;126:1189–98. doi:10.1242/jcs.116855.
Cea LA, Puebla C, Cisterna BA, et al. Fast skeletal myofibers of mdx mouse, model of Duchenne muscular dystrophy, express connexin hemichannels that lead to apoptosis. Cell Mol Life Sci. 2016;73:2583–99. doi:10.1007/s00018-016-2132-2.
•• Cea LA, Cisterna BA, Puebla C, et al. De novo expression of connexin hemichannels in denervated fast skeletal muscles leads to atrophy. Proc Natl Acad Sci U S A. 2013;110:16229–34. doi:10.1073/pnas.1312331110. This paper describes a sequence of relevant events triggered in denervated skeletal muscles that lead to muscle atrophy and shows that de novo expressed connexin43 and connexin45 hemichannels are the cause of the myofibres ionic imbalance and negative protein balance of this muscles.
Cisterna BA, Vargas AA, Puebla C, et al. Connexin hemichannels explain the ionic imbalance and lead to atrophy in denervated skeletal muscles. Biochim Biophys Acta. 2016;1862:2168–76. doi:10.1016/j.bbadis.2016.08.020.
Vargas AA, Cisterna BA, Saavedra-Leiva F, et al. On biophysical properties and sensitivity to gap junction blockers of connexin 39 hemichannels expressed in HeLa cells. Front Physiol. 2017;8:38. doi:10.3389/fphys.2017.00038.
Schalper KA, Sánchez HA, Lee SC, et al. Connexin 43 hemichannels mediate the Ca2+ influx induced by extracellular alkalinization. Am J Physiol Cell Physiol. 2010;299:C1504–15. doi:10.1152/ajpcell.00015.2010.
•• Schalper KA, Palacios-Prado N, Retamal MA, et al. Connexin hemichannel composition determines the FGF-1-induced membrane permeability and free [Ca2+]i responses. Mol Biol Cell. 2008;19:3501–13. doi:10.1091/mbc.E07-12-1240. This paper demonstrates that dexamethasone a synthetic glucocorticoids induces expression of connexin hemichannels in skeletal myofibers. This results in reduction in the resting membrane potential, activation of the protein degradation pathway, activation of the inflammasome, and atrophy. Therefore, it is proposed that glucocorticoids are anti-inflammarory in cells of the immune system but are inflammatory in skeletal muscles.
Cea LA, Balboa E, Puebla C, et al. Dexamethasone-induced muscular atrophy is mediated by functional expression of connexin-based hemichannels. Biochim Biophys Acta. 2016;1862:1891–9. doi:10.1016/j.bbadis.2016.07.003.
Porter JD, Merriam AP, Leahy P, et al. Dissection of temporal gene expression signatures of affected and spared muscle groups in dystrophin-deficient (mdx) mice. Hum Mol Genet. 2003;12:1813–21.
Porter JD, Khanna S, Kaminski HJ, et al. A chronic inflammatory response dominates the skeletal muscle molecular signature in dystrophin-deficient mdx mice. Hum Mol Genet. 2002;11:263–72.
Spencer MJ, Montecino-Rodriguez E, Dorshkind K, et al. Helper (CD4(+)) and cytotoxic (CD8(+)) T cells promote the pathology of dystrophin-deficient muscle. Clin Immunol. 2001;98:235–43. doi:10.1006/clim.2000.4966.
Hodgetts S, Radley H, Davies M, et al. Reduced necrosis of dystrophic muscle by depletion of host neutrophils, or blocking TNFalpha function with Etanercept in mdx mice. Neuromuscul Disord. 2006;16:591–602. doi:10.1016/j.nmd.2006.06.011.
•• Cea LA, Bevilacqua JA, Arriagada C, et al. The absence of dysferlin induces the expression of functional connexin-based hemichannels in human myotubes. BMC Cell Biol. 2016;17 Suppl 1:15. doi:10.1186/s12860-016-0096-6. It demonstrates that myofibers of mdx mice, model of muscular dystrophy associated to mutation in dystrophin, express functional connexin hemichannels. In addition, it shows that these connexin hemichannels leads to increase in cytoplasmic Ca2+ signal, activation of NFkB, and apoptosis.
Whitehead NP, Streamer M, Lusambili LI, et al. Streptomycin reduces stretch-induced membrane permeability in muscles from mdx mice. Neuromuscul Disord. 2006;16:845–54. doi:10.1016/j.nmd.2006.07.024.
Figueroa VA, Retamal MA, Cea LA, et al. Extracellular gentamicin reduces the activity of connexin hemichannels and interferes with purinergic Ca2+ signaling in HeLa cells. Front Cell Neurosci. 2014;8:265. doi:10.3389/fncel.2014.00265.
Balnave CD, Allen DG. Intracellular calcium and force in single mouse muscle fibres following repeated contractions with stretch. J Physiol. 1995;488(Pt 1):25–36. doi:10.1113/jphysiol.1995.sp020943.
Yeung EW, Head SI. Allen, DG Gadolinium reduces short-term stretch-induced muscle damage in isolated mdx mouse muscle fibres. J Physiol. 2003;552:449–58. doi:10.1113/jphysiol.2003.047373.
Bansal D, Miyake K. Vogel, SS et al Defective membrane repair in dysferlin-deficient muscular dystrophy. Nature. 2003;423:168–72. doi:10.1038/nature01573.
Kerr JP, Ziman AP, Mueller AL, et al. Dysferlin stabilizes stress-induced Ca2+ signaling in the transverse tubule membrane. Proc Natl Acad Sci U S A. 2013;110:20831–6. doi:10.1073/pnas.1307960110.
Turk R. Sterrenburg, E, van der Wees, CG et al Common pathological mechanisms in mouse models for muscular dystrophies. FASEB J. 2006;20:127–9. doi:10.1096/fj.05-4678fje.
Rawat R, Cohen TV. Ampong, B et al Inflammasome up-regulation and activation in dysferlin-deficient skeletal muscle. Am J Pathol. 2010;176:2891–900. doi:10.2353/ajpath.2010.090058.
Cea LA, Riquelme MA, Cisterna BA, et al. Connexin- and pannexin-based channels in normal skeletal muscles and their possible role in muscle atrophy. J. Membr. Biol. 2012;245:423–36. doi:10.1007/s00232-012-9485-8.
Cisterna BA, Cardozo C. Sáez, JC Neuronal involvement in muscular atrophy. Front Cell Neurosci. 2014;8:405. doi:10.3389/fncel.2014.00405.
Acknowledgments
This work was supported by the National Institutes of Health R01-AR067210 and R01-AR053643 (to LIP) and T32-AR065971 (to HMD), U.S.A., and by the Fondo Nacional de Desarrollo Científico y Tecnológico (FONDECYT) grant 1150291 (to JCS) and ICM-Economía P09-022-F Centro Interdisciplinario de Neurociencias de Valparaíso (to JCS), Chile.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
Juan Sáez, Hannah Davis, Lilian Plotkin, and Bruno Cisterna declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Osteocytes
Rights and permissions
About this article
Cite this article
Plotkin, L.I., Davis, H.M., Cisterna, B.A. et al. Connexins and Pannexins in Bone and Skeletal Muscle. Curr Osteoporos Rep 15, 326–334 (2017). https://doi.org/10.1007/s11914-017-0374-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-017-0374-z