Abstract
Purpose of Review
COVID-19 has posed a continuously evolving challenge for providers caring for patients with multiple sclerosis (MS). While guidelines from national and international organizations came quickly, these have required constant reassessment and modification as the pandemic has progressed. This review aims to assess the first 2 years of literature on COVID-19 relevant to the clinical management of patients with MS. In particular, we will review how MS impacts the risk of COVID-19 infection, how disease-modifying therapies may alter this risk, and explore considerations regarding disease-modifying therapy (DMT) and vaccination for COVID-19. We will also explore potential ways in which a COVID-19 infection may impact multiple sclerosis. Our goal is to provide an overarching review of the major findings at this stage of the pandemic relevant to those that care for patients with MS.
Recent Findings
Over the course of the COVID-19 pandemic, providers have had to re-evaluate the priorities in the management of MS. A growing number of studies have evaluated the relevant risk factors and considerations regarding MS and particular disease-modifying therapies.
Summary
The long-term impacts of the pandemic on the health of those with MS will continue to be revealed. In general, most patients with MS do not need major revisions to their treatment plan due to COVID-19 risk. However, individuals who are older, more disabled, and on more potent therapies may need to consider strategies for decreasing their overall risk. Regardless, continued improvement in our understanding of interactions between infections, disease-modifying therapy, and MS are paramount to optimizing the care of those with MS going forward.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since severe respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified in December 2019, the pandemic associated with this infection (COVID-19) has posed a continuously evolving challenge for providers caring for patients with multiple sclerosis (MS). These patients are often treated with immunomodulatory medications or have chronic disability that increases the risk of infection and infection-related mortality [1]. Furthermore, infections can result in an increased severity of MS-related symptoms and may trigger clinical relapses [2, 3, 4]. Given the variety of clinical circumstances among MS patients, providers have been forced to adapt to continuously evolving challenges throughout the pandemic.
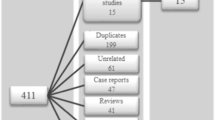
A growing number of studies have identified the clinical characteristics and outcomes of COVID-19 among patients with MS. The long-term effects of COVID-19 infection on individuals with MS remain unknown. Here, we will review the literature from the first 2 years of the COVID-19 pandemic to assess the risk of COVID-19 in the MS population, considerations for disease-modifying therapies (DMT) in the context of the pandemic, and the impact of MS on COVID-19 prevention and treatment strategies.
Risk of COVID-19 Infection for Those with MS
Current evidence does not indicate that there is an increased likelihood of a COVID-19 infection for those with MS compared to the general population [5]. Prior to the COVID-19 pandemic, those with MS appeared to be 2–4 times more likely to be hospitalized with a serious infection [1, 6, 7]. Evidence collected from a case–control study embedded within the Italian MS Registry in March 2021 suggests that people with MS who are younger, are female, have comorbidities, and receive treatments that require visits to a medical setting are more likely to contract SARS-CoV-2 [8]. The authors proposed that younger, less disabled female patients may have had higher numbers of social interactions than those with higher disease activity but this was not directly assessed by the study. A cross-sectional mixed-method study of 407 patients at the MS clinic at the University of Barcelona early in the pandemic (June 2020) found that the incidence of confirmed COVID-19 cases was similar between MS and the general population (five cases, approximately one percent of the cohort). Disease-modifying therapy (DMT) use appeared to have little impact on the risk of infection in this study [9]. A survey of 882 patients with MS in eight cities in China, including Wuhan, found no patients with MS contracted COVID-19. This may have been due to particularly stringent preventative strategies and timing of this study early in the pandemic with data collected prior to June 2020 [10].
Severity, hospitalization rates, and intensive care unit (ICU) admission rates associated with COVID-19 infection do not appear to be increased in general for those with MS [11]. However, several risk factors among those with MS seem to influence the risk of severe COVID-19. Several large national and international databases developed to track risk factors associated with COVID-19 infections over the first year of the pandemic in people with MS have consistently identified male sex, increasing age, cardio-pulmonary comorbidities, a progressive disease course, and higher disability level as risk factors for a more severe COVID-19 course [12••, 13, 14]. These risk factors, and particularly disability level, were also associated with increased mortality [12••]. The North American registry also found that compared to those of the White race, the Black race may also be associated with increased odds of ICU admission and ventilation, but race did not appear to be related to significantly increased mortality [12••].
Risk of MS Relapse Associated with COVID-19
It has been speculated that COVID-19 may increase the risk of clinical relapses in MS patients and unmask subclinical MS, as has been seen in other upper respiratory infections [2]. However, a retrospective cohort study of 56 MS subjects that contracted COVID-19 indicates that neither COVID-19 infection nor subsequent hospitalization appears to increase relapse rates in patients with MS [15]. While there are a mounting number of cases of acute CNS demyelinating diseases associated with COVID-19, whether COVID-19 predisposes or unmasks MS is less clear [16, 17]. Bellucci et al. [18] reviewed four cases of newly diagnosed MS fulfilling the 2017 McDonald Criteria identified in close proximity to SARS-CoV-2 infection. However, based on the small number of cases, it seems plausible that these patients may have had pre-morbid mild or asymptomatic MS that was discovered incidentally due to relapses exacerbated by an infection. Several potential mechanisms may represent pathologic overlap between COVID-19 and MS including the type I interferon (IFN-I) response and the T-helper 17 (TH-17) axis [18].
Disease-Modifying Therapies and COVID-19
There are now numerous DMT that reduce relapses in MS. These medications have a variety of mechanisms of action including cell depletion, alterations in immune cell trafficking, and immunomodulation. Immunity to COVID-19 is complex—and both B and T-cell responses occur concomitantly in patients infected with COVID-19 and contribute to neutralizing antibody development [19]. Guidelines from international organizations were swiftly created in the early period of the pandemic based on our best, though sometimes incomplete, understanding of the mechanisms of these DMT. This advice proved to be sound as supportive evidence has slowly accumulated [20–22].
In general, most individuals are recommended to continue DMT without intentional delays. International survey data suggests that only about 5% of MS patients had delays or changes in their treatment during the pandemic [23]. The authors noted that most of these were delays in infusions with the goal of minimizing potential COVID-19 exposure, and only about half of these delays were advised by the patient’s health care providers. A cross-sectional cohort study in China surveyed 384 patients prior to June 2020, none of whom reported a positive COVID-19 test. However, they did find that the annualized relapse rate (ARR) for those with MS increased compared to the prior year and 20% of these patients reported discontinuing or reducing the dose of their DMT due to fear of hospitalization or inability to obtain their medication [10]. In large cohorts, DMTs do not appear to be independent risk factors for COVID-19 incidence [24••]. Data from the Italian cohort also suggests that the cumulative effect of DMT on the immune system may also be relevant, as opposed to simply considering the most recently administered DMT [8].
Beta-interferons are type I interferons (IFN-I) with known anti-viral properties and are modestly effective DMT. There was early speculation that interferons may provide some protection from the consequences of a dysregulated host immune response to COVID-19, but this has not yet been clearly demonstrated [25]. The North American COVID-19 registry (COViMS) identified a non-significant decreased rate of hospitalization for those on interferon. A safety database cohort of 603 patients taking interferon beta-1a also suggested relatively low rates of serious disease and severe outcomes with COVID-19 [12••, 26]. However, a double-blind, placebo-controlled phase 3 trial of interferon beta-1a plus remdesivir versus remdesivir alone in hospitalized adults with COVID-19 did not suggest benefit with interferon beta-1a administration [27].
The fumarates (such as dimethyl fumarate) are agonists of nuclear factor erythroid 2–related factor 2 (Nrf2) and appear to limit SARS-CoV-2 replication and pro-inflammatory responses in vivo [28]. Despite associated lymphopenia for some patients, dimethyl fumarate does not seem to be associated with an increased infection risk generally [29]. Relative to higher efficacy therapies, dimethyl fumarate use is associated with lower rates of hospitalization and severe infection [24••].
Sphingosine-1-phosphate (S1P) receptor modulators (such as fingolimod, siponimod, and ozanimod) likely confer minimal overall risk of severe COVID-19. While lymphopenia due to sequestration of lymphocytes within the lymphoid tissues (where anti-viral responses are largely generated) is expected with S1P receptor modulators, it is widely believed to represent a functional lymphopenia [30]. It is worth noting that CD4 cells are preferentially targeted by these medications and potential viral infections such as herpes simplex virus, varicella-zoster virus, John Cunningham Virus, and other atypical fungal and bacterial infections have been reported [31]. However, this risk does not seem to be widespread based on larger cohorts [32•]. A review of 283 COVID-19 cases in fingolimod-treated patients and 54 cases in siponimod-treated patients suggests the risk of COVID-19 in patients on S1P receptor modulators is comparable to the general population [33]. This finding was also corroborated by other large databases [12••].
Data from the large registries appears to suggest significantly less risk with natalizumab compared to anti-CD20 DMTs [24••]. This is in-line with theoretical risk; asnatalizumab is unlikely to inhibit the migration of the immune cells relevant for a COVID-19 response [34]. On this basis, some recommend natalizumab for appropriate candidates over the cell-depleting alternatives for those in need of highly effective DMT [22]. However, within the Italian MS registry, those receiving natalizumab were at high risk of acquiring COVID-19, potentially due to frequent exposure to a hospital environment for infusions [8]. Extended dosing intervals may help reduce this exposure risk, though this has not been directly investigated in the context of COVID-19 [35]. Avoidance of the hospital setting may provide additional justification for the utilization of in-home infusion services as well as further development of the subcutaneous forms of natalizumab [36].
The anti-CD20 therapies are broadly used and appear to pose a high risk for serious infections relative to other DMT [32•]. An analysis of data from multiple registries drawn from 28 countries found that anti-CD20 therapies were associated with increased rates of hospitalization and ICU admission compared to pooled other DMTs [24••]. Data from COViMS suggested those on rituximab had a fourfold increased odds of hospitalization for COVID-19 [12••]. Rituximab as compared to ocrelizumab was also associated with significantly higher rates of ventilation compared to alternative DMT. Interestingly, however, neither of the anti-CD20 therapies was associated with a significantly higher rate of death [24••]. While this may be due to a relatively low frequency of deaths within the cohort, this remains an area for potential future investigation.
Cell-depleting therapies such as cladribine and anti-CD52 antibodies (alemtuzumab) have the most theoretical risk among Food and Drug Administration (FDA)–approved MS DMT, at least during the induction period. These medications can lead to a transient and variable period of lymphopenia after each course of treatment; however, data is limited because they are not broadly utilized for MS. However, evidence suggests that lymphopenia in general may not contribute to the increased risk associated with COVID-19 [37, 38, 39]. As an off-label treatment for highly active MS, hematopoietic stem cell transplant (HSCT) is another potent treatment option that may be associated with increased COVID-19 risk. Most consensus statements made a definitive recommendation against HSCT if viable alternatives are available [21, 22, 40]. The level of non-specific immune depletion with HSCT is likely much more significant than with DMT. Data from a cohort of 318 HSCT recipients indicated for hematologic malignancy who contracted COVID-19 found a survival rate of 68% within 30 days following a COVID-19 diagnosis. Older age, an indication for lymphoma, and recency of transplantation appeared to be notable risk factors for a more severe COVID-19 infection [41].
Glucocorticoid use in the 2 months prior to infection conferred an approximately twofold increased risk of hospitalization and a fourfold increased risk of death in the COViMS registry [12••]. Similarly, the pooled registry data from Italy and France found a two- to threefold increase in poor COVID-19 outcomes for those who had used methylprednisolone within 1 month of infection [42]. On the surface, this seems to be at odds with studies showing benefits in outcomes for those with severe COVID-19 who received glucocorticoids which led to World Health Organization (WHO) recommendations advocating for the use of these agents for patients with severe COVID-19 infections [43, 44]. The hypothesized mechanisms of steroid benefit in COVID-19 include downregulation of airway epithelium angiotensin-converting enzyme-2 (ACE-2) receptors and mitigating the dysregulated hyperinflammatory immune response that contributes to morbidity and mortality in COVID-19 [45, 46]. It seems plausible, then, that dose and timing of administration play a critical role in conferring steroid-related risk. Administration proximal to infection may allow unchecked viral replication in the early phase of the disease, for instance. Because of the data on MS patients, it is advisable to exercise caution in the administration of steroids for suspected MS relapses for those with a high risk of COVID-19 infection or complications [21].
Because of the multitude of factors for each patient, individualized approaches to DMT decisions are necessary. This should include an assessment of overall risk based on factors such as the patient’s age, comorbidities, exposure risk, the burden of treatment monitoring, and disability level in addition to the potential risk incurred by DMT. Especially for those on natalizumab or S1P receptor modulators, due to the potential for rebound events, the risk of stopping a DMT may outweigh the potential benefit.
COVID-19 Vaccines and MS
Studies of mRNA vaccine efficacy suggest a reduction in documented COVID-19 infection of over 90% in the general population [47]. The National MS Society and the Multiple Sclerosis International Federation have advised vaccination for most people with MS [20, 21]. Despite these recommendations, nearly 30% of those with MS in a primarily western US cohort were unsure or unwilling to be vaccinated in early 2021 [48]. This is despite evidence that the potential benefits of inactivated virus vaccination in general outweigh any risk for those with MS [49]. In a study of 719 people with MS, reactogenicity to SARS-CoV-2 vaccines appeared to be similar between those with MS and the general population. The most common reactions reported were transient injection site pain, fatigue, and headache [50]. Thus far, COVID-19 vaccination does not appear to increase relapse activity. [51]
Because of the immunosuppressive or immune-modulating effects of some DMTs, vaccine efficacy may be impacted by timing relative to DMT dosing. Impaired vaccination response has been identified in those on cell-depleting therapies (anti-CD20, alemtuzumab) and S1P receptor modulators. Approximately 80% of all patients treated with anti-CD20 therapy or fingolimod have weak humoral immune responses after 2 doses of messenger RNA (mRNA) COVID-19 vaccines [52, 53, 54]. However, it does appear that those on anti-CD20 therapies still develop COVID-19-targeted T-cell responses [55••]. As of April 2022, the National MS Society has recommended that people on these DMTs may benefit from three primary doses as well as two subsequent boosters of mRNA COVID vaccines [56]. Based on a cohort of 175 patients with MS on DMT, this additional dose does appear effective at increasing antibody response [57••]. At this time, it is unclear whether using IgG response as a measure of presumed humoral immunity fully reflects protection against infection, since there is also a contribution by T-cell responses [58].
Other COVID-19 Treatments and MS
The use of hydroxychloroquine and ivermectin is unsupported by the most rigorous available studies and its use is not recommended by the WHO for the prevention or treatment of COVID-19 in the clinical setting [59]. Nonetheless, widespread off-label use of this medication, on the basis of dubious evidence, was extensive enough to cause shortages and widespread increases in cases of toxicity [60]. The use of ivermectin does not have a specific contraindication in the setting of MS for appropriate indications. However, because it is metabolized by CYP450 3A4, it may interact with modafinil and oxcarbazepine. These medications are sometimes used off-label for the management of MS-related symptoms and are also CYP450 3A4 substrates. Hydroxychloroquine has an extensive list of potential drug interactions including DMTs such as S1P receptor modulators due to increased risk of bradycardia and AV block from cumulative QT prolongation [61]. While potential roles for these medications have been considered in the context of MS in pre-clinical and phase 2 trials [62, 63], they do not have a clinical role in the care of MS at this point.
The US FDA authorized tixagevimab/cilgavimab for pre-exposure prophylaxis in particular circumstances for vaccinated individuals on therapies that may reduce or prevent antibody response. Such therapies include anti-CD 20 medications, alemtuzumab, and S1P receptor modulators. However, because it is not widely available at the time of this review, providers may consider stratifying the risk of potential COVID-19 infection among their patients on these therapies based on established risk factors for severe COVID-19 to determine the most appropriate candidates for treatment [64]. At this point, we do not have data regarding the oral anti-virals that received an emergency use authorization by the US FDA in December 2021, nirmatrelvir and molnupiravir. However, there do not appear to be any theoretical contraindications for those on MS DMT.
MS and Post-Acute COVID-19 Syndrome
The number of patients recovering from COVID-19 continues to increase. Along with this, there has been increasing recognition of a group of patients with prolonged and persistent symptoms after an acute COVID-19 infection [65]. Much remains to be established in regard to the pathophysiology and diagnosis of this condition. The WHO defines this condition as prolonged symptoms 2–3 months from the onset of acute COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis [66]. Symptoms related to multiple organ systems have been implicated though neuropsychiatric sequelae including fatigue, myalgia, mood changes, sleep changes, and headaches are commonly noted. A prospective, longitudinal cohort study from the UK MS Register evaluated data from 599 patients with MS who reported infection with COVID-19 and subsequent follow-up. They found that 29% of these patients had symptoms longer than 4 weeks and 12.4% had symptoms lasting beyond 12 weeks. New or worsened fatigue was the most commonly reported symptom. High levels of pre-COVID-19-related neurologic disability appeared to predispose to long-term COVID-19 sequelae [67•].
Conclusion
While MS does not appear to be associated with severity or mortality from COVID-19, it does add layers of complicated decision-making for neurologists and patients. As the pandemic has progressed, there is gathering evidence that minimal change to treatment is in the best interest of most patients [68]. The long-term impacts of the pandemic on the health of those with MS will continue to be revealed. However, it is clear that a nuanced understanding of the infection risk of DMT and the integration of vaccine discussion into the neurology clinic will be an integral part of the future of MS care. Further exploration into the interactions between viruses and MS is needed, since there is much yet to be understood about how viral disease may impact autoimmune and demyelinating conditions.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wijnands JM, et al. Infection-related health care utilization among people with and without multiple sclerosis. Mult Scler. 2017;23(11):1506–16.
Andersen O, et al. Viral infections trigger multiple sclerosis relapses: a prospective seroepidemiological study. J Neurol. 1993;240(7):417–22.
Steelman AJ. Infection as an environmental trigger of multiple sclerosis disease exacerbation. Front Immunol. 2015;6:520.
Oikonen M, et al. Temporal relationship between environmental influenza A and Epstein-Barr viral infections and high multiple sclerosis relapse occurrence. Mult Scler. 2011;17(6):672–80.
Fan M, et al. Risk of COVID-19 infection in MS and neuromyelitis optica spectrum disorders. Neurol Neuroimmunol Neuroinflamm. 2020;7(5).
Montgomery S, Hillert J, Bahmanyar S. Hospital admission due to infections in multiple sclerosis patients. Eur J Neurol. 2013;20(8):1153–60.
Nelson RE, et al. Multiple sclerosis and risk of infection-related hospitalization and death in US veterans. Int J MS Care. 2015;17(5):221–30.
Iaffaldano P, et al. Risk of getting COVID-19 in people with multiple sclerosis: a case-control study. Neurol Neuroimmunol Neuroinflamm. 2022;9(2).
Sepulveda M, et al. Incidence and impact of COVID-19 in MS: a survey from a Barcelona MS unit. Neurol Neuroimmunol Neuroinflamm. 2021;8(2).
Zhang Y, et al. The epidemiology of COVID-19 and MS-related characteristics in a national sample of people with MS in China. Front Neurol. 2021;12:682729.
Richter D, et al. Multiple sclerosis is not associated with an increased risk for severe COVID-19: a nationwide retrospective cross-sectional study from Germany. Neurol Res Pract. 2021;3(1):42.
Salter A. et al. Outcomes and risk factors associated with SARS-CoV-2 infection in a North American registry of patients with multiple sclerosis. JAMA Neurol. 2021;78(6):699–708. This registry-based cross-sectional study of 1626 North American patients with MS and COVID-19 infection identified risk factors for worse COVID-19 outcomes for those with MS, including disability level, older age, and other comorbidities.
Louapre C, et al. Clinical characteristics and outcomes in patients with coronavirus disease 2019 and multiple sclerosis. JAMA Neurol. 2020;77(9):1079–88.
Moreno-Torres I, et al. Risk and outcomes of COVID-19 in patients with multiple sclerosis. Eur J Neurol. 2021;28(11):3712–21.
Etemadifar M, et al. COVID-19 and the risk of relapse in multiple sclerosis patients: a fight with no bystander effect? Mult Scler Relat Disord. 2021;51:102915.
Manzano GS, et al. Acute disseminated encephalomyelitis and acute hemorrhagic leukoencephalitis following COVID-19: systematic review and meta-synthesis. Neurol Neuroimmunol Neuroinflamm. 2021;8(6).
Roman GC, et al. Acute transverse myelitis (ATM): clinical review of 43 patients with COVID-19-associated ATM and 3 post-vaccination ATM serious adverse events with the ChAdOx1 nCoV-19 vaccine (AZD1222). Front Immunol. 2021;12:653786.
Bellucci G, et al. Multiple sclerosis and SARS-CoV-2: has the interplay started? Front Immunol. 2021;12:755333.
Jacobs JJL. Neutralizing antibodies mediate virus-immune pathology of COVID-19. Med Hypotheses. 2020;143:109884.
Society NMS. Disease modifying therapies during the COVID-19 pandemic. 2022 [cited 2022 Feb 8 2022]; Available from: https://www.nationalmssociety.org/coronavirus-covid-19-information/multiple-sclerosis-and-coronavirus/ms-treatment-guidelines-during-coronavirus.
Federation MSI. MS, the coronavirus and vaccines – updated global advice. 2021 [cited 2022 Feb 8 2022]; Available from: https://www.msif.org/news/2020/02/10/the-coronavirus-and-ms-what-you-need-to-know/.
Brownlee W, et al. Treating multiple sclerosis and neuromyelitis optica spectrum disorder during the COVID-19 pandemic. Neurology. 2020;94(22):949–52.
Moss BP, et al. Multiple sclerosis management during the COVID-19 pandemic. Mult Scler. 2020;26(10):1163–71.
Simpson-Yap S, et al. Associations of disease-modifying therapies with COVID-19 severity in multiple sclerosis. Neurology. 2021;97(19):e1870-e1885. This paper utilized aggregate data from registry info across 28 countries to assess the association between DMT and COVID risk.
Berger JR, Brandstadter R, Bar-Or A. COVID-19 and MS disease-modifying therapies. Neurol Neuroimmunol Neuroinflamm. 2020;7(4).
Freedman MS, et al. Outcomes of COVID-19 among patients treated with subcutaneous interferon beta-1a for multiple sclerosis. Mult Scler Relat Disord. 2021;56:103283.
Kalil AC, et al. Efficacy of interferon beta-1a plus remdesivir compared with remdesivir alone in hospitalised adults with COVID-19: a double-bind, randomised, placebo-controlled, phase 3 trial. Lancet Respir Med. 2021;9(12):1365–76.
Olagnier D, et al. SARS-CoV2-mediated suppression of NRF2-signaling reveals potent antiviral and anti-inflammatory activity of 4-octyl-itaconate and dimethyl fumarate. Nat Commun. 2020;11(1):4938.
Mehta D, et al. Effect of dimethyl fumarate on lymphocytes in RRMS. Implic Clin Pract. 2019;92(15):e1724–38.
Thomas K, et al. Fingolimod additionally acts as immunomodulator focused on the innate immune system beyond its prominent effects on lymphocyte recirculation. J Neuroinflammation. 2017;14(1):41.
Zhao Z, et al. Incidence and risk of infection associated with fingolimod in patients with multiple sclerosis: a systematic review and meta-analysis of 8,448 patients from 12 randomized controlled trials. Front Immunol. 2021;12:611711.
Luna G, et al. Infection risks among patients with multiple sclerosis treated with fingolimod, natalizumab, rituximab, and injectable therapies. JAMA Neurol. 2020;77(2):184–191. This paper uses data from a Swedish register to evaluate the risk of various infections associated with DMT prior to the COVID pandemic (2011–2017).
Sullivan R, et al. COVID-19 infection in fingolimod- or siponimod-treated patients: case series. Neurol Neuroimmunol Neuroinflamm. 2021;9(1).
Baker D, et al. The underpinning biology relating to multiple sclerosis disease modifying treatments during the COVID-19 pandemic. Mult Scler Relat Disord. 2020;43:102174.
Clerico M, et al. Extending the interval of natalizumab dosing: is efficacy preserved? Neurotherapeutics. 2020;17(1):200–7.
Lopez PA, et al. Natalizumab subcutaneous injection for the treatment of relapsing multiple sclerosis patients: a new delivery route. Mult Scler Relat Disord. 2021;55:103179.
Loonstra FC, et al. COVID-19 in multiple sclerosis: the Dutch experience. Mult Scler. 2020;26(10):1256–60.
Evangelou N, Garjani A. Lymphocyte counts and the risk of COVID-19 in people with MS. Mult Scler. 2021;27(10):1625–6.
Bsteh G, et al. COVID-19 severity and mortality in multiple sclerosis are not associated with immunotherapy: insights from a nation-wide Austrian registry. PLoS ONE. 2021;16(7):e0255316.
Reyes S, et al. Update on the management of multiple sclerosis during the COVID-19 pandemic and post pandemic: an international consensus statement. J Neuroimmunol. 2021;357:577627.
Sharma A, et al. Clinical characteristics and outcomes of COVID-19 in haematopoietic stem-cell transplantation recipients: an observational cohort study. Lancet Haematol. 2021;8(3):e185–93.
Sormani MP, et al. DMTs and COVID-19 severity in MS: a pooled analysis from Italy and France. Ann Clin Transl Neurol. 2021;8(8):1738–44.
Group RC, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021;384(8):693-704.
Group WHOREAfC-TW, et al. Association between administration of systemic corticosteroids and mortality among critically Ill patients with COVID-19: A Meta-analysis. JAMA. 2020;324(13):1330–1341.
Finney LJ, et al. Inhaled corticosteroids downregulate the SARS-CoV-2 receptor ACE2 in COPD through suppression of type I interferon. J Allergy Clin Immunol. 2021;147(2):510–519 e5.
Ghanei M, et al. The efficacy of corticosteroids therapy in patients with moderate to severe SARS-CoV-2 infection: a multicenter, randomized, open-label trial. Respir Res. 2021;22(1):245.
Dagan N, et al. BNT162b2 mRNA COVID-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. 2021;384(15):1412–23.
Xiang XM, et al. COVID-19 vaccination willingness among people with multiple sclerosis. Mult Scler J Exp Transl Clin. 2021;7(2):20552173211017160.
Farez MF, et al. Practice guideline update summary: vaccine-preventable infections and immunization in multiple sclerosis: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2019;93(13):584–94.
Briggs FBS, et al. COVID-19 vaccination reactogenicity in persons with multiple sclerosis. Neurol Neuroimmunol Neuroinflamm. 2022;9(1).
Achiron A, et al. COVID-19 vaccination in patients with multiple sclerosis: what we have learnt by February 2021. Mult Scler. 2021;27(6):864–70.
Achiron A, et al. Humoral immune response to COVID-19 mRNA vaccine in patients with multiple sclerosis treated with high-efficacy disease-modifying therapies. Ther Adv Neurol Disord. 2021;14:17562864211012836.
Konig M, et al. Humoral immunity to SARS-CoV-2 mRNA vaccination in multiple sclerosis: the relevance of time since last rituximab infusion and first experience from sporadic revaccinations. J Neurol Neurosurg Psychiatry. 2021.
Brill L, et al. Humoral and T-cell response to SARS-CoV-2 vaccination in patients with multiple sclerosis treated with ocrelizumab. JAMA Neurol. 2021;78(12):1510–4.
Apostolidis SA, et al. Cellular and humoral immune responses following SARS-CoV-2 mRNA vaccination in patients with multiple sclerosis on anti-CD20 therapy. Nat Med. 2021;27(11):1990–2001. This paper evaluates antigen-specific T and B cell responses to COVID vaccination in patients on anti-CD20 medications.
Prevention CfDCa. COVID-19 vaccines for moderately or severely immunocompromised people. April 1, 2022 4/5/2022]; Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/immuno.html?s_cid=11707:covid%20booster%20immunocompromised:sem.ga:p:RG:GM:gen:PTN:FY22.
Bar-Or A, et al. Effect of ocrelizumab on vaccine responses in patients with multiple sclerosis: the VELOCE study. Neurology. 2020;95(14):e1999–e2008. This study assessed responses to selected vaccines in ocrelizumab-treated patients with RRMS. It played a large role in guiding the timing for COVID vaccination in the early phases of the pandemic.
Konig M, et al. Immunogenicity and safety of a third SARS-CoV-2 vaccine dose in patients with multiple sclerosis and weak immune response after COVID-19 vaccination. JAMA Neurol. 2022.
Update to living WHO guideline on drugs for COVID-19. BMJ. 2022;376:o80.
Chiu MN, Bhardwaj M, Sah SP. Safety profile of COVID-19 drugs in a real clinical setting. Eur J Clin Pharmacol. 2022.
Pilote S, Simard C, Drolet B. Fingolimod (Gilenya((R)) ) in multiple sclerosis: bradycardia, atrioventricular blocks, and mild effect on the QTc interval. Something to do with the L-type calcium channel? Fundam Clin Pharmacol. 2017;31(4):392–402.
Koch MW, et al. Hydroxychloroquine for primary progressive multiple sclerosis. Ann Neurol. 2021;90(6):940–8.
Zabala A, et al. P2X4 receptor controls microglia activation and favors remyelination in autoimmune encephalitis. EMBO Mol Med. 2018;10(8).
Society NM. Prevention & treatments for COVID-19. 2021 December 17, 2021 [cited December 17, 2021 February 16]; Available from: https://www.nationalmssociety.org/coronavirus-covid-19-information/multiple-sclerosis-and-coronavirus/suspected-covid-19-and-ms.
Nalbandian A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–15.
Soriano JB, et al. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2021.
Garjani A, et al. Recovery from COVID-19 in multiple sclerosis: a prospective and longitudinal cohort study of the United Kingdom Multiple Sclerosis Register. Neurol Neuroimmunol Neuroinflamm. 2022;9(1). This longitudinal, prospective cohort study evaluated the recovery of over 500 people with MS who also had a COVID infection.
Mateen FJ, et al. Impact of COVID-19 on U.S. and Canadian neurologists' therapeutic approach to multiple sclerosis: a survey of knowledge, attitudes, and practices. J Neurol. 2020;267(12):3467–3475.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Hollen has no financial or non-financial interests that are directly or indirectly related to the work submitted for publication to disclose. Dr. Bernard has no financial or non-financial interests that are directly or indirectly related to the work submitted for publication to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Demyelinating Disorders
Rights and permissions
About this article
Cite this article
Hollen, C., Bernard, J. Multiple Sclerosis Management During the COVID-19 Pandemic. Curr Neurol Neurosci Rep 22, 537–543 (2022). https://doi.org/10.1007/s11910-022-01211-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-022-01211-9