Abstract
Antibody mediated limbic encephalitis is an increasingly recognized cause of seizures in cryptogenic epilepsy. Autoimmune encephalitis and epilepsy have been linked to both neuronal intracellular antibodies (GAD65, ANNA-1, and Ma) and neuronal cell surface antibodies (VGKC complex, NMDAR, AMPA, GABA-B, and GluR5). This article outlines the latest data on these various antibodies with a focus on their association with acute seizures in limbic encephalitis and likely increased risk for chronic epilepsy. There is mounting evidence that these antibodies may play a role in acute onset and chronic seizures in the general epilepsy population without manifesting typical limbic encephalitis symptoms. This review will discuss the data supporting early recognition and treatment options, beyond typical antiepileptic medications, necessary to improve outcomes in this epilepsy subgroup.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000;342:314–9.
Iorio R, Lennon V. Neural antigen-specific autoimmune disorders. Immunol Rev. 2012;248:104–21.
Bien CG, Schulz-Bonhage A, Deckert M, et al. Limbic encephalitis not associated with neoplasm as a cause of temporal lobe epilepsy. Neurology. 2000;55:1823–8.
Gultekin SH, Rosenfeld MR, Voltz R, et al. Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings, and tumor association in 50 patients. Brain. 2000;123:1481–94.
Vincent A, Irani SR, Lang B. The growing recognition of immunotherapy-responsive seizure disorders with autoantibodies to specific neuronal proteins. Curr Opin Neurol. 2010;23:144–50.
Bien CG, Scheffer IE. Autoantibodies and epilepsy. Epilepsia. 2011;52(3):18–22.
Zuliani L, Graus F, Giometto B, et al. Central nervous system neuronal surface antibody associated syndromes: review and guidelines for recognition. J Neurol Neurosurg Psychiatry. 2012;83:638–45.
Irani SR, Bien CG, Lang B. Autoimmune epilepsies. Curr Opin Neurol. 2011;24:146–53.
Graus F, Saiz A, Lai M, et al. Neuronal surface antigen antibodies in limbic encephalitis: clinical-immunologic associations. Neurology. 2008;71:930–6.
Alamowitch S, Graus F, Uchuya M, et al. Limbic encephalitis and small cell lung cancer: clinical and immunological features. Brain. 1997;120:923–8.
Graus F, Keime-Guibert F, Rene R, et al. Anti-Hu-associated paraneoplastic encephalomyelitis: analysis of 200 patients. Brain. 2001;124:1138–48.
Lucchinetti CF, Kimmel DW, Lennon VA. Paraneoplastic and oncologic profiles of patients seropositive for type 1 antineuronal nuclear autoantibodies. Neurology. 1998;50:652–7.
Dalmau J, Graus F, Rosenblum MK, et al. Anti-Hu-associated paraneoplastic encephalomyelitis/sensory neuronopathy. A clinical study of 71 patients. Medicine. 1992;71:59–72.
Rosenfeld MR, Eichen JG, Wade DF, et al. Molecular and clinical diversity in paraneoplastic immunity to Ma proteins. Ann Neurol. 2001;50:339–48.
Dalmau J, Graus F, Villarejo A, et al. Clinical analysis of anti-Ma2-associated encephalitis. Brain. 2004;127:1831–44.
Mata S, Muscas GC, Naldi I, et al. Non-paraneoplastic limbic encephalitis associated with anti-glutamic acid decarboxylase antibodies. J Neuroimmunol. 2008;199(1–2):155–9.
Blanc F, Ruppert E, Kleitz C, et al. Acute limbic encephalitis and glutamic acid decarboxylase antibodies: a reality? J Neurol Sci. 2009;287:69–71.
Malter MP, Helmstaedter C, Urbach H. Antibodies to glutamic acid decarboxylase define a form of limbic encephalitis. Ann Neurol. 2010;67:470–8.
Majoie HJM, de Baets M, Renier W, et al. Antibodies to voltage-gated potassium and calcium channels in epilepsy. Epilepsy Res. 2006;71:135–41.
Vincent A, Buckley C, Schott J, et al. Potassium channel antibody-associated encephalopathy: a potentially immunotherapy-responsive form of limbic encephalitis. Brain. 2004;127:701–12.
•• Lai M, Huijbers MGM, Lancaster E, et al. Investigation of LGI1 as the antigen in limbic encephalitis previously attributed to potassium channels: a case series. Lancet Neurol. 2010;9:776–85. This study of 57 patients with limbic encephalitis attributed to voltage-gated potassium channels demonstrated that the antibodies were actually binding to Lgi1 and CASPR2 antigens, proteins associated with the VGKC complex.
Irani SR, Alexander S, Waters P, et al. Antibodies to Kv1 potassium channel-complex proteins leucine-rich, glioma inactivated 1 protein and contactin-associated protein-2 in limbic encephalitis, Morvan’s syndrome and acquired neuromyotonia. Brain. 2010;133:2734–48.
Dalmau J, Tüzün E, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36.
Sansing LH, Tüzün E, Ko MW, Baccon J, Lynch DR, Dalmau J. A patient with encephalitis associated with NMDA receptor antibodies. Nat Clin Pract Neurol. 2007;3(5):291–6.
Dalmau J, Gleichman AJ, Hughes EG, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008;7:1091–8.
Irani SR, Bera K, Waters P, et al. N-methyl-D-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain. 2010;133:1655–67.
Dalmau J, Lancaster E, Martinez-Hernandez E, et al. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011;10:63–74.
•• Titulaer MJ, McCracken L, Gabilondo I, et al. Treatment and prognostic factors for long-term outcomes in patients with anti-NMDA receptor encephalitis: an observation cohort study. Lancet Neurol. 2013;12:157–65. This observation cohort study of immunotherapy outcomes on 501 patients with NMDAR encephalitis found that 81 % of patients had improvement with good outcome at 2 years. Predictors of good outcome included early initiation of treatment and initiation of second line therapy (rituximab and/or cyclophosphamide).
Lai M, Hughes EG, Peng X, et al. AMPA receptor antibodies in limbic encephalitis alter synaptic receptor location. Ann Neurol. 2009;65:424–34.
Bataller L, Galiano R, Garcia-Escrig M, et al. Reversible paraneoplastic limbic encephalitis associated with antibodies to the AMPA receptor. Neurology. 2010;74:265–7.
• Lancaster E, Lai M, Hughes E. Antibodies to the GABAB receptor in limbic encephalitis with seizures: case series and characterization of the antigen. Lancet Neurol. 2010;9:67–76. This study of 15 patients with limbic encephalitis was the first to identify GABA-B antibodies as a cause of this disorder. All 15 patients with GABA-B antibody encephalitis developed seizures with 13 of the patients noted to have seizures as their presenting symptom.
Boronat A, Sabater L, Saiz A, et al. GABAB receptor antibodies in limbic encephalitis and anti-GAD-associated neurologic disorders. Neurology. 2011;76:795–800.
Lancaster E, Martinez-Hernandez E, Titulaer MJ, et al. Antibodies to metabotropic glutamate receptor 5 in the Ophelia syndrome. Neurology. 2011;77:1698–701.
•• Irani SR, Michell AW, Lang B, et al. Faciobrachial dystonic seizures precede Lgi1 antibody limbic encephalitis. Ann Neurol. 2011;69:892–900. This case series described 29 patients with faciobrachial dystonic seizures. Lgi1 antibodies were found in 89 % of the patients. This seizure type showed a much poorer response to antiepileptic medications compared with immunotherapy.
Irani SR, Vincent A. NMDA receptor antibody encephalitis. Curr Neurol Neurosci Rep. 2011;11:298–304.
Schmitt SE, Pargeon K, Frechette ES, et al. Extreme delta brush: a unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology. 2012;79:1094–100.
Dalmau J. Status epilepticus due to paraneoplastic and nonparaneoplastic encephalitides. Epilepsia. 2009;50 Suppl. 12:58–60.
Graus F, Boronat A, Xifro X, et al. The expanding clinical profile of anti-AMPA receptor encephalitis. Neurology. 2010;74:857–9.
Vianello M, Tavolato B, Giometto B. Glutamic acid decarboxylase autoantibodies and neurological disorders. Neurol Sci. 2002;23:145–51.
Giometto B, Nicolao P, Macucci M, et al. Temporal-lobe epilepsy associated with glutamic-acid-decarboxylase autoantibodies. Lancet. 1998;352:457.
Peltola J, Kulmala P, Isojarvi J, et al. Autoantibodies to glutamic acid decarboxylase in patients with therapy-resistant epilepsy. Neurology. 2000;55(1):46–50.
Errichiello L, Perruolo G, Pascarella A, et al. Autoantibodies to glutamic acid decarboxylase (GAD) in focal and generalized epilepsy: a study on 233 patients. J Neuroimmunol. 2009;211(1–2):120–3.
Errichiello L, Striano S, Zara F, et al. Temporal lobe epilepsy and anti-glutamic acid decarboxylase autoimmunity. Neurol Sci. 2011;32:547–50.
Liimatainen S, Peltola M, Sabater L, et al. Clinical significance of glutamic acid decarboxylase antibodies in patients with epilepsy. Epilepsia. 2010;51(5):760–7.
• Falip M, Carreno M, Miro J, et al. Prevalence and immunological spectrum of temporal lobe epilepsy with glutamic acid decarboxylase antibodies. Eur J Neurol. 2012;19:827–33. This study examined the prevalence of GAD65 antibodies in 42 patients with adult onset temporal lobe epilepsy, 19 with known etiology and 23 with unknown etiology. GAD65 antibodies were present in 21 % of the patients (8.7 % high titers) with unknown etiology of their epilepsy.
Porta-Etessam J, Ruiz-Morales J, Millan JM, et al. Epilepsia partialis continua and frontal features as a debut of anti-Hu paraneo- plastic encephalomyelitis with focal frontal encephalitis. Eur J Neurol. 2001;8:359–60.
Shavit YB, Graus F, Probst A, et al. Epilepsia partialis continua: a new manifestation of anti-Hu-associated paraneoplastic encephalomyelitis. Ann Neurol. 1999;45:255–8.
Rudzinskia LA, Pittockb SJ, McKeon A, et al. Extratemporal EEG and MRI findings in ANNA-1 (anti-Hu) encephalitis. Epilepsy Res. 2011;95:255–62.
McKnight K, Jiang Y, Hart Y, Cavey A, Wroe S, Blank M, et al. Serum antibodies in epilepsy and seizure-associated disorders. Neurology. 2005;65:1730–6.
Niehusmann P, Dalmau J, Rudlowski C, et al. Diagnostic value of N-methyl-D-aspartate receptor antibodies in women with new-onset epilepsy. Arch Neurol. 2009;66(4):458–64.
Bien CG, Elger CE. Limbic encephalitis: a cause of temporal lobe epilepsy with onset in adult life. Epilepsy Behav. 2007;10:529–38.
Keime-Guibert F, Graus F, Fleury A, et al. Treatment of paraneoplastic neurological syndromes with antineuronal antibodies (Anti-Hu, Anti-Yo) with a combination of immunoglobulins, cyclophosphamide, and methylprednisolone. J Neurol Neurosurg Psychiatry. 2000;68(4):479–82.
Battaler L, Kleopa KA, Wu GF, et al. Autoimmune limbic encephalitis in 39 patients: immunophenotypes and outcomes. J Neurol Neurosurg Psychiatry. 2007;78:381–5.
Gabilondo I, Saiz A, Galán L, et al. Analysis of relapses in anti-NMDAR encephalitis. Neurology. 2011;77:996–9.
Irani SR, Buckley C, Vincent A, et al. Immunotherapy-responsive seizure-like episodes with potassium channel antibodies. Neurology. 2008;71:1647–8.
Kaymakamzade B, Kansu T, Tan E, et al. LGI1 related limbic encephalitis and response to immunosuppressive therapy. J Neurol. 2011;258:2075–7.
•• Quek AM, Britton JW, McKeon A, et al. Autoimmune epilepsy: clinical characteristics and response to immunotherapy. Arch Neurol. 2012;69(5):582–93. This case series of 32 patients with autoimmune antibody-mediated epilepsy treated with immunotherapy reported an improvement rate of 81 %, with 18 patients becoming seizure free. Patients who showed improvement had a significantly shorter time to therapy initiation than patients who did not respond to therapy, at 4 months and 22 months respectively.
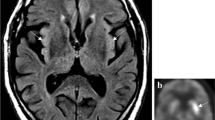
Scheid R, Lincke T, Voltz R, et al. Serial 18F-fluoro-2-deoxy-D-glucose positron emission tomography and magnetic resonance imaging of paraneoplastic limbic encephalitis. Arch Neurol. 2004;61:1785–9.
Ances BM, Vitaliani R, Taylor RA, et al. Treatment-responsive limbic encephalitis identified by neuropil antibodies: MRI and PET correlates. Brain. 2005;128(8):1764–77.
Fauser S, Talazko J, Wagner K, et al. FDG-PET and MRI in potassium channel antibody-associated non-paraneoplastic limbic encephalitis: correlation with clinical course and neuropsychology. Acta Neurol Scand. 2005;111:338–43.
Urbach H, Soeder BM, Jeub M, et al. Serial MRI of limbic encephalitis. Neuroradiology. 2006;48:380–6.
Bien CG, Urbach H, Schramm J, et al. Limbic encephalitis as a precipitating event in adult-onset temporal lobe epilepsy. Neurology. 2007;69:1236–44.
Titulaer MJ, Soffietti R, Dalmau J, et al. Screening for tumors in paraneoplastic syndromes: report of an EFNS task force. Eur J Neurol. 2011;18:19–27.
Conflict of Interest
Cynthia M. Correll declares no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Epilepsy
Rights and permissions
About this article
Cite this article
Correll, C.M. Antibodies in Epilepsy. Curr Neurol Neurosci Rep 13, 348 (2013). https://doi.org/10.1007/s11910-013-0348-1
Published:
DOI: https://doi.org/10.1007/s11910-013-0348-1