Abstract
Spinal epidural abscess (SEA) remains a relatively infrequent diagnosis. Staphylococcus aureus is the most common organism identified, and the infectious source in SEA emanates from skin and soft tissue infections in about 20 % of instances. The thoracic spine is most often involved followed by the lumbar spine. The classic triad of fever, spinal pain, and neurological deficit is present in but a minority of patients. The appearance of neurological deficits with SEA has a significant impact on the prognosis; therefore, early diagnosis is imperative. Magnetic resonance imaging has permitted earlier diagnosis, although significant delays in diagnosis are common due to the nonspecific symptoms that frequently attend the disorder. Due to the rarity of this condition, there have been few randomized controlled trials to evaluate new treatment strategies, and most recommendations regarding treatment are based on case series studies often derived from the experiences at a single center.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hlavin ML et al. Spinal epidural abscess: a ten-year perspective. Neurosurgery. 1990;27(2):177–84.
Rigamonti D et al. Spinal epidural abscess: contemporary trends in etiology, evaluation, and management. Surg Neurol. 1999;52(2):189–96. discussion 197.
Nussbaum ES et al. Spinal epidural abscess: a report of 40 cases and review. Surg Neurol. 1992;38(3):225–31.
Baker AS et al. Spinal epidural abscess. N Engl J Med. 1975;293(10):463–8.
Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 2000;23(4):175–204. discussion 205.
Hawkins M, Bolton M. Pediatric spinal epidural abscess: a 9-year institutional review and review of the literature. Pediatrics. 2013;132(6):e1680–5. This article provides a good review of limited literature available in the pediatric patients.
West KR, Mason RC, Sun M. Nocardia spinal epidural abscess: 14-year follow-up. Orthopedics. 2012;35(1):e128–31.
Atalay B et al. Nocardial epidural abscess of the thoracic spinal cord and review of the literature. J Infect Chemother. 2005;11(3):169–71.
Gudinchet F, Chapuis L, Berger D. Diagnosis of anterior cervical spinal epidural abscess by US and MRI in a newborn. Pediatr Radiol. 1991;21(7):515–7.
Danner RL, Hartman BJ. Update on spinal epidural abscess: 35 cases and review of the literature. Rev Infect Dis. 1987;9(2):265–74.
Adogwa O et al. Spontaneous spinal epidural abscess in patients 50 years of age and older: a 15-year institutional perspective and review of the literature: clinical article. J Neurosurg Spine. 2014;20(3):344–9.
Patel AR et al. Spinal epidural abscesses: risk factors, medical versus surgical management, a retrospective review of 128 cases. Spine J. 2014;14(2):326–30.
Siddiq DM, Musher DM, Darouiche RO. Spinal and paraspinal pneumococcal infections—a review. Eur J Clin Microbiol Infect Dis. 2014;33(4):517–27.
Younus F, Jimenez V. Spinal epidural abscess due to Streptococcus pneumoniae in an HIV-infected adult. Infection. 2001;29(4):234–6.
Darouiche RO et al. Bacterial spinal epidural abscess. Review of 43 cases and literature survey. Medicine (Baltimore). 1992;71(6):369–85.
Huang CR et al. Clinical characteristics and therapeutic outcome of Gram-negative bacterial spinal epidural abscess in adults. J Clin Neurosci. 2011;18(2):213–7.
Tasher D et al. Cat scratch disease with cervical vertebral osteomyelitis and spinal epidural abscess. Pediatr Infect Dis J. 2009;28(9):848–50.
Boyaci A., et al., Spinal epidural abscess in brucellosis. BMJ Case Rep, 2013. 2013.
Arora S, Kumar R. Tubercular spinal epidural abscess involving the dorsal-lumbar-sacral region without osseous involvement. J Infect Dev Ctries. 2011;5(7):544–9.
Baallal H, El Mostarchid B. Multisegmental tubercular spinal epidural abscess. Pan Afr Med J. 2013;14:2.
Kaufman DM, Kaplan JG, Litman N. Infectious agents in spinal epidural abscesses. Neurology. 1980;30(8):844–50.
Jiang Z et al. Vertebral osteomyelitis and epidural abscess due to Aspergillus nidulans resulting in spinal cord compression: case report and literature review. J Int Med Res. 2013;41(2):502–10.
Gupta PK et al. Aspergillus spinal epidural abscess. Pediatr Neurosurg. 2001;35(1):18–23.
Yung BC. Aggressive thoracic actinomycosis complicated by vertebral osteomyelitis and epidural abscess leading to spinal cord compression. Spine. 2000;25(6):745–8.
Kannangara DW, Tanaka T, Thadepalli H. Spinal epidural abscess due to Actinomyces israelii. Neurology. 1981;31(2):202–4.
Maraki S et al. Roseomonas spinal epidural abscess complicating instrumented posterior lumbar interbody fusion. J Clin Microbiol. 2013;51(7):2458–60.
Charles RW, Mody GM, Govender S. Pyogenic infection of the lumbar vertebral spine due to gas-forming organisms. A case report. Spine. 1989;14(5):541–3.
Sapico FL, Montgomerie JZ. Pyogenic vertebral osteomyelitis: report of nine cases and review of the literature. Rev Infect Dis. 1979;1(5):754–76.
Chiller TM et al. Clinical findings for fungal infections caused by methylprednisolone injections. N Engl J Med. 2013;369(17):1610–9.
Kainer MA et al. Fungal infections associated with contaminated methylprednisolone in Tennessee. N Engl J Med. 2012;367(23):2194–203.
Smith RM. Fungal infections associated with contaminated methylprednisolone injections. N Engl J Med. 2013;369(17):1598–609. This article describes in detail the large outbreak in 2012 of fungal infections, including spinal epidural abscesses, caused by injection of methylprednisone contaminated with Exserohilum rostratum.
Malani AN et al. Magnetic resonance imaging screening to identify spinal and paraspinal infections associated with injections of contaminated methylprednisolone acetate. JAMA. 2013;309(23):2465–72.
Shintani S et al. Iatrogenic acute spinal epidural abscess with septic meningitis: MR findings. Clin Neurol Neurosurg. 1992;94(3):253–5.
Heusner AP. Nontuberculous spinal epidural infections. N Engl J Med. 1948;239(23):845–54.
Frat JP et al. Cervical spinal epidural abscess and meningitis due to Prevotella oris and Peptostreptococcus micros after retropharyngeal surgery. Intensive Care Med. 2004;30(8):1695.
Jang YJ, Rhee CK. Retropharyngeal abscess associated with vertebral osteomyelitis and spinal epidural abscess. Otolaryngol Head Neck Surg. 1998;119(6):705–8.
Elian D et al. Spinal epidural abscess: an unusual complication of bacterial endocarditis. Infection. 1984;12(4):258–9.
Wong M et al. Epidural extension of infected chest wall haematoma and empyema causing spinal cord compression. Heart Lung Circ. 2014;23(1):e20–3.
Hancock DO. A study of 49 patients with acute spinal extradural abscess. Paraplegia. 1973;10(4):285–8.
Feldenzer JA et al. The pathogenesis of spinal epidural abscess: microangiographic studies in an experimental model. J Neurosurg. 1988;69(1):110–4.
Feldenzer JA et al. Experimental spinal epidural abscess: a pathophysiological model in the rabbit. Neurosurgery. 1987;20(6):859–67.
Hakin RN, Burt AA, Cook JB. Acute spinal epidural abscess. Paraplegia. 1979;17(3):330–6.
Phillips GE, Jefferson A. Acute spinal epidural abscess. Observations from fourteen cases. Postgrad Med J. 1979;55(648):712–5.
Verner EF, Musher DM. Spinal epidural abscess. Med Clin North Am. 1985;69(2):375–84.
Davis DP et al. The clinical presentation and impact of diagnostic delays on emergency department patients with spinal epidural abscess. J Emerg Med. 2004;26(3):285–91.
Tang HJ et al. Spinal epidural abscess—experience with 46 patients and evaluation of prognostic factors. J Infect. 2002;45(2):76–81.
McCaig LF, Nawar EW. National hospital ambulatory medical care survey: 2004 emergency department summary. Adv Data. 2006;372:1–29.
Thiruganasambandamoorthy, V., et al., Risk factors for serious underlying pathology in adult emergency department nontraumatic low back pain patients. J Emerg Med, 2014.
Bremer AA, Darouiche RO. Spinal epidural abscess presenting as intra-abdominal pathology: a case report and literature review. J Emerg Med. 2004;26(1):51–6.
Posada IJ. Acute spinal epidural abscess presenting as acute meningitis. Med Clin. 1986;87(13):566–7.
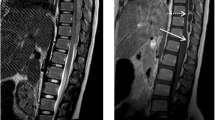
Parkinson JF, Sekhon LH. Spinal epidural abscess: appearance on magnetic resonance imaging as a guide to surgical management. Report of five cases. Neurosurg Focus. 2004;17(6):E12.
Numaguchi Y et al. Spinal epidural abscess: evaluation with gadolinium-enhanced MR imaging. Radiographics. 1993;13(3):545–59. discussion 559–60.
Johnson K, Gunaratne S, Shaffi M. Pitfalls of triage by imaging in spinal epidural abscess. Emerg Med Australas. 2014;26(2):205–6.
Koppel BS et al. Epidural spinal infection in intravenous drug abusers. Arch Neurol. 1988;45(12):1331–7.
Davis DP. Prospective evaluation of a clinical decision guideline to diagnose spinal epidural abscess in patients who present to the emergency department with spine pain. J Neurosurg Spine. 2011;14(6):765–70. This article outlines a good approach to identify patients for emergent MR imaging of the spine using risk factor assessment and erythrocyte sedimentation rate and C-reactive protein as screening laboratory markers among patients presenting to the emergency room with low back pain to decrease diagnostic delays in patients with spinal epidural abscess.
Curry Jr WT et al. Spinal epidural abscess: clinical presentation, management, and outcome. Surg Neurol. 2005;63(4):364–71. discussion 371.
Sorensen P. Spinal epidural abscesses: conservative treatment for selected subgroups of patients. Br J Neurosurg. 2003;17(6):513–8.
Connor Jr DE. Comparison of operative and nonoperative management of spinal epidural abscess: a retrospective review of clinical and laboratory predictors of neurological outcome. J Neurosurg Spine. 2013;19(1):119–27. This study identifies predictors of neurological outcome and compares operative and non operative management of patients with spinal epidural abscess.
Kim S.D., et al., Independent predictors of failure of nonoperative management of spinal epidural abscesses. The Spine Journal, (0).
Siddiq F, Malik AR, Smego Jr RA. Percutaneous computed tomography-guided needle aspiration drainage of spinal epidural abscess. South Med J. 2006;99(12):1406–7.
Lyu RK et al. Spinal epidural abscess successfully treated with percutaneous, computed tomography-guided, needle aspiration and parenteral antibiotic therapy: case report and review of the literature. Neurosurgery. 2002;51(2):509–12. discussion 512.
Safavi-Abbasi S, Maurer AJ, Rabb CH. Minimally invasive treatment of multilevel spinal epidural abscess. J Neurosurg Spine. 2013;18(1):32–5.
McGee-Collett M, Johnston IH. Spinal epidural abscess: presentation and treatment. A report of 21 cases. Med J Aust. 1991;155(1):14–7.
Redekop GJ, Del Maestro RF. Diagnosis and management of spinal epidural abscess. Can J Neurol Sci. 1992;19(2):180–7.
Yang SY. Spinal epidural abscess. N Z Med J. 1982;95(707):302–4.
Del Curling Jr O, Gower DJ, McWhorter JM. Changing concepts in spinal epidural abscess: a report of 29 cases. Neurosurgery. 1990;27(2):185–92.
Compliance with Ethics Guidelines
Conflict of Interest
Joseph Berger received grants from PML Consortium, Biogen Idec, and Novartis. Berger received personal fees from Amgen, Astra-Zeneca, Bristol Myers Squibb, Eisai, Janssen, Millennium, Parexel, Pfizer, Roche, Takeda, Genentech, Genzyme, Incyte, Inhibikase, Johnson and Johnson, Novartis, the American Academy of Neurology, and the Consortium of MS Centers. Prashanth Krishnamohan has no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Central Nervous System Infections
Rights and permissions
About this article
Cite this article
Krishnamohan, P., Berger, J.R. Spinal Epidural Abscess. Curr Infect Dis Rep 16, 436 (2014). https://doi.org/10.1007/s11908-014-0436-7
Published:
DOI: https://doi.org/10.1007/s11908-014-0436-7