Abstract
Septic shock is a major cause of morbidity and mortality throughout the world. Source control, antimicrobial therapy, early goal-directed fluid resuscitation, and infusion of vasoactive pharmaceuticals remain the cornerstones of treatment. However, the cardiovascular management of septic shock is evolving. Basic science and clinical researchers have identified novel drug targets and are testing the efficacy of new therapeutic agents. For example, prevention of microvascular leak during septic shock is the focus of active investigations and may soon provide considerable benefit to patients. Among the important topics that will be discussed in this review are the following: the role of vascular endothelial dysfunction in microvascular leak, the impact of cytokines upon structural and functional proteins within the endothelial barrier and within the heart, and the ability of selective vasopressin 1a receptor agonists to minimize tissue edema and improve hemodynamic status.
Similar content being viewed by others
Introduction
Sepsis is a major cause of morbidity and mortality throughout the world. In the U.S. alone, approximately 750,000 cases of sepsis occur annually, leading to roughly 210,000 deaths [1, 2]. The average hospital stay is 20 days for septic patients. The annual cost of caring for patients with sepsis in the U.S. exceeds $16 billion [3]. Management of sepsis and septic shock is evolving. Each year, basic science and clinical researchers advance our understanding of the underlying mechanisms. The purpose of this review is to summarize the cardiovascular management of septic shock, as well as many recent scientific discoveries.
The Pathophysiology of Sepsis-Induced Cardiovascular Dysfunction
Severe sepsis is defined as sepsis associated with hypotension, hypoperfusion, or organ dysfunction. Septic shock occurs when the hypotension is refractory to fluid resuscitation, necessitating vasopressor support [4–7]. Three significant cardiovascular events occur as sepsis progresses to severe sepsis and then to septic shock: (1) Intravascular volume decreases due to capillary leak; (2) vascular tone increases, then significantly decreases; and (3) cardiac contractility is depressed.
Capillary Leak and Diminished Vascular Tone: Dysfunction at the Level of the Vascular Endothelium
The vascular endothelium is a complex and dynamic structure. It plays crucial roles in organ homeostasis, vasomotor tone, hemostasis, and leukocyte trafficking. Endothelial activation contributes to the body’s inflammatory response by releasing signaling molecules such as E-selectin, VCAM-1, and ICAM-1. These substances facilitate leukocyte transmigration and promote local coagulation. As an early response to infection, endothelial activation helps to prevent the spread of pathogens [8]. However, this adaptive response becomes amplified and dysfunctional in sepsis. Microvascular leak is one of the consequences.
Clinicians have long known that septic patients suffer from microvascular leak and that it contributes to tissue edema, hypotension, and shock. During the past decade, several research teams have elucidated mechanisms by which vascular endothelial dysfunction contributes to this process. Intercellular junctions within the endothelial barrier have drawn particular interest, especially proteins within these junctions. Structures like cadherin are now recognized as playing important roles [9]. Processes such as actin remodeling within the vascular endothelial cytoskeleton [10] and caspase-mediated apoptosis of endothelial cells [11] have also been shown to be important. Secreted endothelial growth factors are also an important part of vascular endothelial dysfunction. They have been the focus of several investigations. Angiopoietin-2 has been shown to diminish endothelial barrier function and prime endothelial cells to respond to tumor necrosis factor alpha (TNFα). Vascular endothelial growth factor A is now known to be a potent inducer of tissue edema [12]. Angiopoietin-2 levels have even been shown to have prognostic value for septic patients [13]. Targeting microvascular leak is a potential area for new therapeutics. For example, London et al. demonstrated that recombinant Slit protein attenuates endothelial permeability caused by endotoxin and cytokines through altered trafficking of vascular endothelial-cadherin. Treatment with Slit has been shown to improve survival in multiple animal models of sepsis (see Fig. 1) [14••, 15].
Vascular leak induced by sepsis and reversed with Slit protein. London et al. [14••] demonstrated the importance of endothelial cell junctions in sepsis and provided a potential therapeutic target. a At baseline, the endothelium is semipermeable, and VE-cadherins are a major component of cell junctions. VE-cadherins are bound by and stabilized by other proteins, including p120-catenin (not shown). b In sepsis, inflammatory cytokines lead to internalization of VE-cadherins and disruption of the endothelial barrier. This results in vascular leak and accumulation of edema in the interstitial space. c Treatment with Slit prevents dissociation of VE-cadherins via the Robo4 receptor, reducing vascular leak. Three different mouse models (using endotoxin, cecal ligation and perforation leading to polymicrobial sepsis, and infection with H5N1 influenza virus) were used to confirm the prevention of vascular leak by Slit. Dramatic improvements in mortality were demonstrated
Endothelial dysfunction also contributes to impaired regulation of vasomotor tone, primarily through disturbances in nitric oxide (NO) production. NO is normally synthesized by endothelial cells (eNOS synthase) under physiologic conditions. Early in sepsis, decreased production of NO by eNOS occurs and tips the endothelial homeostatic balance toward vasoconstriction [16]. Later, sepsis leads to an increase in the production of NO, since inducible NOS (iNOS) produces much larger concentrations of NO than those produced by eNOS [17•].
The vascular endothelium plays a central role in mediating hemostasis by influencing anticoagulant and procoagulant processes. There appear to be several mechanisms by which the procoagulant state is enhanced in sepsis (which can result in disseminated intravascular coagulation and organ dysfunction). It is known that tissue factor is expressed by circulating monocytes and by endothelial cells, leading to formation of thrombin [18, 19]. In sepsis, counterregulatory systems involving the endothelium (such as protein C and tissue factor pathway inhibitor [TFPI]) may be defective. Endothelial expression of thrombomodulin (a protein that amplifies activation of protein C) is downregulated by circulating cytokines in sepsis [20]. TFPI binds to factor VIIa, tissue factor, and factor Xa. Animal studies have shown that depletion of TFPI (as occurs in sepsis) increases intravascular coagulation, while infusion of TFPI decreases intravascular coagulation and improves organ function [21, 22]. Fibrinolysis is also suppressed in severe sepsis by several mechanisms, including increased production of plasminogen activator inhibitor-1 by endothelial cells [23].
Septic Cardiomyopathy
Sepsis-induced left ventricle (LV) systolic dysfunction is a common component of septic shock. Using transesophageal echocardiography, Vileillard-Baron et al. demonstrated that 60 % of intubated patients with septic shock experienced global LV hypokinesis (defined by LV ejection fraction [LVEF] less than 45 %) during the first 3 days of sepsis [24]. Notably, these investigators reported that sepsis-induced reductions in LVEF were not associated with worse outcomes. This observation was consistent with findings from previous studies. For instance, in one small study published in 1984, sepsis survivors had lower initial LVEF (mean value of 32 %) than did nonsurvivors [25].
LV diastolic dysfunction also commonly occurs during septic shock. It also appears to be reversible. In one small study, 20 % of patients with septic shock had isolated impairment of LV relaxation, which subsequently normalized with resolution of sepsis [26]. More recently, Landesberg et al. examined the impact of diastolic dysfunction using echocardiography in a cohort of septic patients and found not only that it was common (38 % of the patients had isolated diastolic dysfunction), but also that its presence was a powerful predictor of mortality (in contrast to systolic dysfunction) [27•]. The degree to which microvascular leak is responsible for sepsis-induced systolic and/or diastolic dysfunction is unclear.
Biomarkers for cardiac dysfunction are useful during the management of septic shock. Elevation of troponin levels occurs in half of all patients with septic shock [28] and is associated with LV dysfunction as assessed by echocardiography, as well as adverse outcomes [29, 30]. In fact, elevation of troponin levels can actually be used to predict the clinical course in patients who have not yet developed shock. For example, Rosjo et al. demonstrated that elevations in troponin T predict subsequent shock in patients with severe sepsis [31]. Elevated BNP levels seem to mark the onset of sepsis-induced myocardial depression. They also have prognostic value [32]. BNP levels are elevated in both systolic and diastolic dysfunction [27•]. A reasonable approach to using biomarkers may be to monitor troponin and BNP levels early in patients with severe sepsis or septic shock both for prognosis and to alert clinicians to the possibility of cardiac dysfunction. Normal BNP and troponin levels make severe cardiac dysfunction unlikely, while elevated levels should prompt echocardiography. Later in the course of sepsis, biomarkers and/or echocardiography can be rechecked if there is suspicion of worsening cardiac dysfunction.
The Molecular Biology of Septic Cardiomyopathy
Lipopolysaccharide (LPS) and TNFα induce hemodynamic alterations during sepsis, including myocardial depression [33]. The combination of TNFα and interleukin-1β (IL1β) is extremely cardiodepressive [34]. Cardiomyocytes are the mechanical effector cells for these cytokines. However, recent evidence suggests that cardiomyocytes also respond to signals from substances like LPS, TNFα, and IL1β by producing cytokines, some of which are secreted and some of which are retained intracellularly. These secondary cytokines appear to play a major role in sepsis-induced cardiodepression [33].
Cardiomyocytes express a wide variety of toll-like receptors, which bind to various exogenous ligands, including bacterial cell components, as well as endogenous ligands released as part of the systemic inflammatory response. Binding of cardiomyocyte toll-like receptors leads to expression of inflammatory cytokines and decreased cardiomyocyte contractility through multiple pathways [35]. For example, two recently discovered proteins are S100A8 and S100A9, which are small calcium-regulating proteins that are upregulated during the toll-like receptor-initiated proinflammatory response and contribute to a decrease in cardiomyocyte contractility [36]. Another important molecule that is upregulated by toll-like receptors is intracellular adhesion molecule-1 (ICAM-1). Activated leukocytes and other ligands bind to ICAM-1 via CD18, which alters intracellular calcium release through cytoskeleton signaling and leads to decreased contractility. This event is prevented by anti-ICAM-1 and anti-CD18 antibodies [37, 38].
NO also plays an important role in septic cardiomyopathy. It is produced not only by endothelial cells, but also by myocytes. NOS is induced by proinflammatory cytokines involved in sepsis, and overproduction of NO leads to myocardial depression. Several animal studies have shown reversal of myocardial depression by NOS inhibition. Furthermore, iNOS-deficient mice seem to be resistant to cardiac dysfunction induced by endotoxin [39–41]. However, not all effects of NO on the heart are deleterious. For instance, NO may promote coronary vasodilation by counteracting vasoconstriction induced by other vasomotor substances produced in sepsis [42]. NO may also serve to improve diastolic function by facilitating LV relaxation [43].
Neuroendocrine Elements of Septic Shock
Derangements of the hypothalamic–pituitary–adrenal axis also play an important role in septic shock physiology. Indeed, adrenal insufficiency may be common in septic shock patients [44]. Furthermore, adrenal insufficiency may be associated with higher mortality [45, 46]. Recently the term “critical illness-related corticosteroid insufficiency” has been used to describe adrenal insufficiency plus tissue resistance to corticosteroids resulting in protracted inflammation.
There is also evidence that a relative deficiency of vasopressin contributes to the physiology of septic shock. A recent study of patients and rats that died from septic shock showed that posttranscriptional synthesis and transport of vasopressin are diminished in the magnocellular neurons of supraoptic and paraventricular nuclei [47].
Management of Septic Shock
Source Control and Early Antimicrobial Therapy
Source control and early antimicrobial administration are essential elements of septic shock management. Recent studies indicate that time is of the essence with regard to both elements. For example, a retrospective analysis of 2,731 patients with septic shock demonstrated that every hour of delay in antimicrobial administration after the onset of hypotension over the ensuing 6 h was associated with an average decrease in survival of 7.6 % [48]. Similarly, in a recent single-center cohort study, dramatic improvements in mortality were demonstrated when antibiotics were administered before the 1-h mark [49]. When the source of infection is unknown, broad-spectrum antimicrobials covering both gram-positive and gram-negative bacteria are warranted. Narrowing of the antimicrobial spectrum can take place after culture and sensitivity data are obtained [50, 51]. Early source control (e.g., drainage of an intra-abdominal abscess, removal of an infected foreign body) is equally important [52].
Insufficient Delivery of Oxygen and Nutrients in Sepsis
Poor organ perfusion and insufficient delivery of oxygen and nutrients to meet tissue metabolic demands are hallmarks of shock, independent of etiology. Oxygen delivery depends primarily on cardiac output and hemoglobin concentration, as described in the equation:
Cardiac output is a product of heart rate and stroke volume. Stroke volume is determined by preload, the inotropic state of the LV, and afterload. The vasoplegic state and capillary leak associated with sepsis commonly cause a relative hypovolemia that leads to reductions in preload and cardiac output.
Fluid Resuscitation in Sepsis: How Fast? How Much?
Early and aggressive fluid resuscitation is given high priority in the Society of Critical Care Medicine’s Surviving Sepsis Campaign Guidelines [53]. These recommendations are based in large part on a study of early goal-directed therapy published by Rivers et al. [5]. According to the Surviving Sepsis Campaign Guidelines, fluid resuscitation (within the first 6 h of presentation) should target a central venous pressure (CVP) of 8–12 mm Hg, urinary output ≥ 0.5 ml/kg/hr, mean arterial pressure (MAP) ≥ 65 mm Hg and central venous oxygen saturation of ≥70%. When followed, these guidelines may result in the administration of large fluid volumes.
During the past decade, the practice of large volume fluid resuscitation for patients experiencing shock has come under scrutiny. It is now recognized that excessive fluid administration may contribute to acute lung injury (ALI), abdominal compartment syndrome, coagulopathy, and cerebral edema [54–56]. For patients who are already suffering from ALI, it has been shown that conservative fluid management results in improved lung function and reductions in the duration of mechanical ventilation and intensive care [57]. Because sepsis is commonly complicated by ALI, conservative fluid management may be particularly beneficial for septic patients.
The Fluid and Catheter Treatment Trial (FACTT) highlighted potential detrimental effects of fluid administration beyond the initial resuscitation period, suggesting that clinicians should justify the administration of additional fluids using objective hemodynamic data [58]. There were two groups of patients in FACTT: (1) a liberal fluid management group, in which fluids or furosemide were administered to maintain a CVP between 10 and 14 mm Hg or a pulmonary capillary wedge pressure between 14 and 18 mm Hg (assuming no shock physiology); and (2) a conservative fluid management group, in which fluids or furosemide were administered to maintain a CVP < 4 mm Hg or a pulmonary capillary wedge pressure < 8 mm Hg. All the patients had ALI. Of the patients, 60 % were septic. The investigators observed a statistically significant increase in the number of ventilator and intensive care unit (ICU) free days for the restrictive fluid management group, without worsening of renal function or shock.
The most effective method of assessing the need for additional fluids after the initial resuscitation period is unclear. Several options are available. One approach is to evaluate preload using transthoracic echocardiography (TTE) imaging of the inferior vena cava via a subcostal view. This approach does not facilitate measurement of LV volume. It helps to determine whether the patient’s LV output is likely to improve after administration of additional intravascular volume. The diameter of the inferior vena cava is measured 2 cm from the junction with the right atrium. A diameter of less than 2 cm with more than 50 % collapse during inspiration suggests that ventricular output will increase if preload is enhanced [59, 60]. Another approach is to use the distensibility index of the inferior vena cava [(Dmax − Dmin)/Dmin]. Using a cutoff of 18 % for the distensibility index, TTE performed well in differentiating fluid responders (cardiac index increase ≥15%) from nonresponders [60]. Systolic pressure variation, pulse pressure variation, stroke volume variation, and plethysmographic waveform variation have also been shown to have utility as dynamic measures of intravascular volume in mechanically ventilated patients [61]. However, standard approaches to measuring these dynamic variables are needed before they can be widely used in clinical practice during the management of septic shock.
Our recommendation is to use transthoracic echocardiography to guide fluid resuscitation when echocardiography is available. When it is not available, we suggest following the most recently published Surviving Sepsis Guidelines and targeting a CVP ≥ 8–12 mmHg.
Metabolic indicators of the adequacy of resuscitation (such as base excess and blood lactic acid level) are useful adjuncts in the evaluation of intravascular volume. A base excess of less than −3 (base deficit) suggests a metabolic acidosis and hypoperfusion of tissues. While intravascular volume depletion may be the cause of a base deficit, conditions such as hyperchloremic states can confound the evaluation. Lactic acidosis (arterial lactic acid level greater than 5 mmol/L with an arterial pH less than 7.35) is also commonly associated with hypovolemia and hypoperfusion of tissues [62]. However, high catecholamine levels can cause elevated lactic acid levels despite adequate intravascular volume.
Fluid Resuscitation in Sepsis: What Type?
The ideal resuscitation fluid for septic shock patients is unclear. The current sepsis guidelines recommend either crystalloids or natural/artificial colloids for initial fluid resuscitation. Crystalloids are defined as solutions containing molecules with molecular weight less than 30 kDa, while colloids are those containing molecules with molecular weight greater than 30 kDa [63]. Fluid replacement may be undertaken using crystalloids, nonsynthetic colloids (such as albumin), nonprotein colloids (such as starches and gelatins), packed red blood cells (PRBCs), fresh frozen plasma (FFP), or cryoprecipitate. The choice of replacement fluid may be directed by clinical or laboratory evidence of need for a specific substance [64].
There are numerous crystalloids available for fluid resuscitation of patients experiencing septic shock. Normal saline and Ringer’s lactate solution (LR) are the most commonly available. Normal saline and LR are similar in their capacity to increase intravascular volume. However, normal saline infusion is associated with a significant incidence of hyperchloremic metabolic acidosis, which has been associated with impaired renal function [65]. Normal saline contains 154 mEq/L of chloride, while LR contains just 109 mEq/L. The pH of normal saline is 5.6, while the pH of LR is 6.6. Infusion of LR with a racemic mixture of lactate may result in pulmonary and hepatic apoptosis and release of proinflammatory mediators, which can contribute to acute respiratory distress syndrome and multiple organ failure [66]. The D-isomer of lactate may be responsible for these adverse effects. Mammalian cells produce only the L-lactate isomer, while bacteria produce the D isomer. There is evidence that mammals do not metabolize the D form of lactate efficiently. In a swine model of hemorrhagic shock, elimination of D-lactate from the LR solution prevented apoptotic cell death in the lung and liver [64, 67]. During the past 5 years, L-isomer only LR preparations have been more commonly used [64].
The most widely available nonsynthetic colloid is albumin, which is available as 4 % or 5 % and 25 % solutions. The saline versus albumin fluid evaluation (SAFE) trial was the first large randomized study to address the issue of whether crystalloid or colloid is preferable during resuscitation of critically ill patients in general. It demonstrated no difference in 28-day outcomes in this patient population [68]. However, a subgroup analysis of patients with severe sepsis suggested that albumin might be preferable to normal saline in this patient population [69]. In the subgroup analysis, it was determined that albumin (as compared with saline) did not impair renal or other organ function (Sequential Organ Failure Assessment scores). In addition, albumin administration was associated with a lower risk of death (using multivariate analysis, the adjusted OR for death for albumin was 0.71). In 2007, McIntyre et al. published the results of a retrospective multicenter cohort study in Canada that investigated whether crystalloid alone versus a combination of colloid and crystalloid administered during the first 6 h after identification of sepsis influenced ICU mortality or organ failure. This group found no association between hospital mortality or organ failure and quantity or type of fluid [70]. A prospective comparison of the effectiveness of 5 % albumin versus normal saline on 90-day mortality for patients with early septic shock (PRECISE RCT) is now underway [71].
Hydroxyethyl starches (such as hetastarch, pentastarch, and tetrastarch) are synthetic colloids available for volume resuscitation. Hetastarch and tetrastarch are 6 % solutions in sodium chloride, while pentastarch is a 10 % solution in sodium chloride. All hydroxyethyl starches can induce allergic and hypersensitivity reactions. They also have the capacity to prolong prothrombin and partial thromboplastin times. They can also alter platelet function [72–74]. Administration of hetastarch and pentastarch should not exceed 20 mL/kg, due to platelet and reticuloendothelial dysfunction. Pentastarch has been shown to cause renal impairment [75]. However, one prospective, multicenter, observational study in critically ill patients suggested that this does not occur with hetastarch [76]. Hextend is a balanced, high-molecular-weight hydroxyethyl starch that is suspended in lactate-buffered solution. In a recently completed multicenter study, patients with severe sepsis assigned to fluid resuscitation with hydroxyethyl starch (130/0.4) had an increased risk of death at day 90 and were more likely to required renal replacement therapy when compared with patients receiving Ringer’s acetate [77].
PRBCs can also be used for resuscitation of septic shock patients, although the hemoglobin level at which PRBC transfusion should be initiated is a matter of considerable debate. Because oxygen delivery depends in large part upon the hemoglobin level, it has been argued that raising the hemoglobin concentration in septic shock patients should improve tissue perfusion. However, transfusing blood products has risks (e.g., transfusion transmitted infections, transfusion-related acute lung injury (TRALI), acute transfusion reactions, hemolytic transfusion reactions, etc.) [78]. Consequently, there is a risk-to-benefit ratio that must be considered. The transfusion requirements in critical care (TRICC) trial suggested that a hemoglobin level of 7 g/dL was appropriate as a transfusion trigger for critically ill patients not experiencing acute myocardial infarction and unstable angina [79]. However, only 41 of almost 850 patients enrolled in the TRICC trial were septic. Consequently, the relevance of the TRICC trial data for the management of patients in septic shock is unclear. One strategy for the management of septic shock patients is to determine the need for PRBC transfusion on the basis of the central venous oxygen saturation [5]. According to this strategy, the hematocrit should be maintained above 30 % when the central venous oxygen saturation is lower than 70 %. Consensus with regard to an optimal transfusion strategy for patients experiencing septic shock has yet to be achieved.
FFP administration is useful when replacement of coagulation factors is needed. Cryoprecipitate administration may be appropriate when specific elements of the clotting process are deficient, such as fibrinogen, factor VII, or von Willebrand factor. For septic shock patients, this situation may arise when disseminated intravascular coagulation occurs and fibrinogen levels are low [80]. Cryoprecipitate is dissolved in only a small volume of plasma. Consequently, it is not useful as a volume-expanding agent. TRALI may develop after FFP or cryoprecipitate administration. The incidence is 1 in 5,000 to 1 in 10,000 units of plasma-containing products transfused. It is more commonly severe when FFP is administered, as compared with blood products containing smaller amounts of plasma, such as platelets or cryoprecipitate. TRALI is characterized by sudden onset of noncardiogenic pulmonary edema. It occurs within a few hours of transfusion and is attributed to antibodies in donor plasma against antigens present on the recipient’s leukocytes [81, 82].
Vasoactive Pharmaceuticals
Pharmaceutical agents are commonly used to manipulate blood pressure in septic shock patients. These drugs act by altering cardiac output and/or vascular tone (the primary determinants of blood pressure). Some vasoactive pharmaceuticals (such as dopamine and vasopressin) may also impact the endocrine and immune systems. To select the appropriate pharmaceutical agent for any given septic shock patient, it may be necessary to measure cardiac output, systemic vascular resistance, and/or central venous oxygen saturation. It may also be appropriate to evaluate tissue perfusion using metabolic indicators (such as base excess and blood lactic acid level).
A mean arterial blood pressure (MAP) goal of 65 mm Hg or greater is appropriate for most septic shock patients. To achieve this goal, the Society of Critical Care Medicine’s Surviving Sepsis Guidelines suggest that norepinephrine and dopamine should be administered (while providing appropriate fluid resuscitation) [53]. Norepinephrine is an agonist for α adrenergic and β1 adrenergic receptors. It is useful for increasing vascular tone. Although it primarily increases MAP by vasoconstriction, it can be expected to simultaneously increase stroke volume and cardiac output by 10 –15 % [6]. Norepinephrine may be more effective than dopamine at reversing hypotension in septic shock patients. In open-label trials, norepinephrine administration was shown to increase MAP in patients who remained hypotensive after fluid resuscitation and dopamine [6]. The vasoconstrictive effects of norepinephrine can impact renal hemodynamics adversely. However, this has not been a problem in adequately volume-resuscitated patients with hyperdynamic septic shock. Norepinephrine has not been shown to diminish splanchnic perfusion more than dopamine or epinephrine during the management of septic shock [83].
Dopamine is a dopamine 1 receptor agonist, as well as a β1 and α adrenergic receptor agonist at escalating doses. Dopamine increases MAP and cardiac output, primarily due to an increase in stroke volume and, to a lesser extent, due to increases in heart rate [6]. At higher doses (>10 mcg/kg/min), dopamine is pro-arrhythmic. Like norepinephrine, dopamine will cause tissue necrosis if extravasation occurs.
The most recent Surviving Sepsis Campaign Guidelines did not indicate whether dopamine or norepinephrine is preferable as the initial vasopressor during management of patients with septic shock. However, the next version of the Surviving Sepsis Campaign Guidelines may reflect a preference for norepinephrine, on the basis of a randomized controlled trial published in 2010. In that study, investigators randomized 1,679 patients with shock (1,044 of whom experienced septic shock) to either dopamine or norepinephrine. They observed no significant difference in 28-days mortality when dopamine was compared with norepinephrine. However, they noted an increase in the rate of arrhythmias in the patients randomized to dopamine (24 % vs. 12 %) [84].
The Surviving Sepsis Campaign Guidelines suggest that vasopressin should be considered for patients who have persistent hypotension due to sepsis, despite the administration of norepinephrine and dopamine. At least one survey suggests that these recommendations are being followed [85]. However, these recommendations may not be consistent with findings from the vasopressin in septic shock trial (VASST), which demonstrated that vasopressin was most beneficial (i.e., decreased mortality) in patients with less severe septic shock. Vasopressin serves as a vasopressor due to its ability to activate V1 receptors on vascular smooth muscle, as well as its capacity to block ATP-sensitive potassium channels. However, it is a nonselective vasopressin receptor agonist. It increases plasma cortisol levels and acts by a different mechanism than exogenous catecholamines, so it can be used as adjunctive vasopressor therapy when catecholamines are being infused. Vasopressin levels have been shown to be reduced in septic shock patients [7, 86].
Several recent studies suggest that selective V1a receptor agonists may be more beneficial than vasopressin in the management of septic shock. After studies of pneumonia-induced septic shock in sheep, Traber et al. reported improved hemodynamics with minimal microvascular leak when a selective V1a receptor agonist was administered [87]. Rehberg et al. reported improved survival and hemodynamics when a V1a receptor agonist was investigated using an ovine fecal peritonitis septic shock model [88••].
Epinephrine is an agonist for all adrenergic receptor subtypes. The Surviving Sepsis Campaign Guidelines do not support the use of epinephrine as a first-line agent in the treatment of septic shock. However, there are data indicating that epinephrine administration may be an appropriate first choice in certain circumstances (e.g., when patients experience septic cardiomyopathy) [83, 89, 90].
Phenylephrine is an α1 adrenergic receptor agonist. It serves as a vasoconstrictor and may elicit a reflex bradycardia. Phenylephrine should be used cautiously in patients with severely depressed myocardium. They may not tolerate large or sudden increases in LV afterload [91]. Phenylephrine can achieve similar hemodynamic results as norepinephrine, though higher doses tend to be required (underscoring phenylephrine’s relatively low potency as a vasoconstrictor) [92].
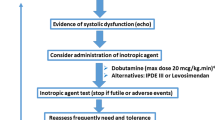
Dobutamine is an agonist for both β1 and β2 adrenergic receptors. Its β2 adrenergic receptor activating properties may lead to peripheral vasodilatation and afterload reduction. Consequently, it may improve tissue perfusion. However, the peripheral vasodilation may also lead to blood pressure reductions in septic shock patients [93].
Our recommendation is to administer norepinephrine as the initial vasoactive pharmaceutical agent during the management of septic shock (while fluid resuscitation is taking place). We suggest vasopressin as the second agent. We support the administration of an inotropic agent (dobutamine or epinephrine) if tissue perfusion is inadequate (as demonstrated by a persistently low-central venous oxygen saturation.
Steroid Therapy
The role of corticosteroids in the management of septic shock has been debated for decades. A recent meta-analysis taking into account 12 randomized trials using steroids (including the corticosteroid therapy of septic shock trial) found a significant reduction in mortality after administration of low-dose corticosteroids for 1 week or more (risk ratio 0.84) [94•]. Nevertheless, the most recent Surviving Sepsis Campaign Guidelines offer only a weak recommendation for steroid administration during the management of septic shock [95].
Conclusion
Sepsis remains a major cause of morbidity and mortality throughout the world. A better understanding of the mechanisms by which septic shock occurs may soon lead to more effective therapies. Source control, antimicrobial therapy, early goal-directed fluid resuscitation, and infusion of vasoactive pharmaceuticals remain the cornerstones of septic shock management. The role of corticosteroids in the treatment of septic shock is unclear. As a consequence of basic science investigations, new therapeutic agents are being developed to treat the capillary leak syndrome that commonly afflicts septic shock patients. Clinical trials of selective V1a receptor agonists are underway. The potential for these agents to minimize tissue edema and improve hemodynamic status in septic shock patients is encouraging.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fernandes Jr CJ, Akamine N, Knobel E. Myocardial depression in sepsis. Shock. 2008;30 Suppl 1:14–7.
Zanotti-Cavazzoni SL, Hollenberg SM. Cardiac dysfunction in severe sepsis and septic shock. Curr Opin Crit Care. 2009;15:392–7.
O’Brien Jr JM, Ali NA, Aberegg SK, et al. Sepsis. Am J Med. 2007;120:1012–22.
Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet. 2005;365:63–78.
Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77.
Hollenberg SM. Vasopressor support in septic shock. Chest. 2007;132:1678–87.
Parrillo JE. Septic shock–vasopressin, norepinephrine, and urgency. N Engl J Med. 2008;358:954–6.
Lee WL, Liles WC. Endothelial activation, dysfunction and permeability during severe infections. Curr Opin Hematol. 2011;18:191–6.
Mochizuki N. Vascular integrity mediated by vascular endothelial cadherin and regulated by sphingosine 1-phosphate and angiopoietin-1. Circ J. 2009;73:2183–91.
Hoang MV, Nagy JA, Senger DR. Active Rac1 improves pathologic VEGF neovessel architecture and reduces vascular leak: mechanistic similarities with angiopoietin-1. Blood. 2011;117:1751–60.
Hu H, Li X, Li Y, et al. Calpain-1 induces apoptosis in pulmonary microvascular endothelial cells under septic conditions. Microvasc Res. 2009;78:33–9.
Jonkam CC, Lange M, Traber DL, et al. Cardiovascular collapse and vascular permeability changes in an ovine model of methicillin-resistant Staphylococcus aureus sepsis. Shock. 2009;32:621–5.
Siner JM, Bhandari V, Engle KM, et al. Elevated serum angiopoietin 2 levels are associated with increased mortality in sepsis. Shock. 2009;31:348–53.
•• London NR, Zhu W, Bozza FA, et al.: Targeting Robo4-dependent Slit signaling to survive the cytokine storm in sepsis and influenza. Sci Transl Med. 2010;2:23ra19. This study offers a new interesting therapeutic target in the management of septic shock. The slit protein binds to the Robo-4 receptor on the endothelial cells and thus stabilizes the intercellular junctions. The net effect in animal models was decreased vascular leak and decreased mortality.
Ye X, Ding J, Zhou X, et al. Divergent roles of endothelial NF-kappaB in multiple organ injury and bacterial clearance in mouse models of sepsis. J Exp Med. 2008;205:1303–15.
Zhou M, Wang P, Chaudry IH. Endothelial nitric oxide synthase is downregulated during hyperdynamic sepsis. Biochim Biophys Acta. 1997;1335:182–90.
• Ait-Oufella H, Maury E, Lehoux S, et al. The endothelium: physiological functions and role in microcirculatory failure during severe sepsis. Intensive Care Med. 2010;36:1286–98. Extensive and up-to-date review of the entdothelium and its functions focusing on changes that occur in sepsis.
Franco RF, de Jonge E, Dekkers PE, et al. The in vivo kinetics of tissue factor messenger RNA expression during human endotoxemia: relationship with activation of coagulation. Blood. 2000;96:554–9.
Lupu C, Westmuckett AD, Peer G, et al. Tissue factor-dependent coagulation is preferentially up-regulated within arterial branching areas in a baboon model of Escherichia coli sepsis. Am J Pathol. 2005;167:1161–72.
Faust SN, Levin M, Harrison OB, et al. Dysfunction of endothelial protein C activation in severe meningococcal sepsis. N Engl J Med. 2001;345:408–16.
Sandset PM, Warn-Cramer BJ, Rao LV, et al. Depletion of extrinsic pathway inhibitor (EPI) sensitizes rabbits to disseminated intravascular coagulation induced with tissue factor: evidence supporting a physiologic role for EPI as a natural anticoagulant. Proc Natl Acad Sci USA. 1991;88:708–12.
Creasey AA, Chang AC, Feigen L, et al. Tissue factor pathway inhibitor reduces mortality from Escherichia coli septic shock. J Clin Invest. 1993;91:2850–60.
Mavrommatis AC, Theodoridis T, Economou M, et al. Activation of the fibrinolytic system and utilization of the coagulation inhibitors in sepsis: comparison with severe sepsis and septic shock. Intensive Care Med. 2001;27:1853–9.
Vieillard-Baron A, Caille V, Charron C, et al. Actual incidence of global left ventricular hypokinesia in adult septic shock. Crit Care Med. 2008;36:1701–6.
Parker MM, Shelhamer JH, Bacharach SL, et al. Profound but reversible myocardial depression in patients with septic shock. Ann Intern Med. 1984;100:483–90.
Bouhemad B, Nicolas-Robin A, Arbelot C, et al. Isolated and reversible impairment of ventricular relaxation in patients with septic shock. Crit Care Med. 2008;36:766–74.
• Landesberg G, Gilon D, Meroz Y, et al. Diastolic dysfunction and mortality in severe sepsis and septic shock. Eur Heart J. 2012;33:895–903. Septic cardiomyopathy is a clinical entity that deserves future research. This was a large observational study using tissue Doppler imaging to assess cardiac function in patients with severe sepsis. It found that diastolic dysfunction had a significant impact on mortality.
Fernandes Jr CJ, Akamine N, Knobel E. Cardiac troponin: a new serum marker of myocardial injury in sepsis. Intensive Care Med. 1999;25:1165–8.
Mehta NJ, Khan IA, Gupta V, et al. Cardiac troponin I predicts myocardial dysfunction and adverse outcome in septic shock. Int J Cardiol. 2004;95:13–7.
Ammann P, Maggiorini M, Bertel O, et al. Troponin as a risk factor for mortality in critically ill patients without acute coronary syndromes. J Am Coll Cardiol. 2003;41:2004–9.
Rosjo H, Varpula M, Hagve TA, et al. Circulating high sensitivity troponin T in severe sepsis and septic shock: distribution, associated factors, and relation to outcome. Intensive Care Med. 2011;37:77–85.
Post F, Weilemann LS, Messow CM, et al. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36:3030–7.
Muller-Werdan U, Buerke M, Ebelt H, et al. Septic cardiomyopathy—a not yet discovered cardiomyopathy? Exp Clin Cardiol. 2006;11:226–36.
Kumar A, Thota V, Dee L, et al. Tumor necrosis factor alpha and interleukin 1beta are responsible for in vitro myocardial cell depression induced by human septic shock serum. J Exp Med. 1996;183:949–58.
Boyd JH, Mathur S, Wang Y, et al. Toll-like receptor stimulation in cardiomyoctes decreases contractility and initiates an NF-kappaB dependent inflammatory response. Cardiovasc Res. 2006;72:384–93.
Boyd JH, Kan B, Roberts H, et al. S100A8 and S100A9 mediate endotoxin-induced cardiomyocyte dysfunction via the receptor for advanced glycation end products. Circ Res. 2008;102:1239–46.
Davani EY, Dorscheid DR, Lee CH, et al. Novel regulatory mechanism of cardiomyocyte contractility involving ICAM-1 and the cytoskeleton. Am J Physiol Heart Circ Physiol. 2004;287:H1013–22.
Davani EY, Boyd JH, Dorscheid DR, et al. Cardiac ICAM-1 mediates leukocyte-dependent decreased ventricular contractility in endotoxemic mice. Cardiovasc Res. 2006;72:134–42.
Balligand JL, Ungureanu D, Kelly RA, et al. Abnormal contractile function due to induction of nitric oxide synthesis in rat cardiac myocytes follows exposure to activated macrophage-conditioned medium. J Clin Invest. 1993;91:2314–9.
Brady AJ, Warren JB, Poole-Wilson PA, et al. Nitric oxide attenuates cardiac myocyte contraction. Am J Physiol. 1993;265:H176–82.
Ullrich R, Scherrer-Crosbie M, Bloch KD, et al. Congenital deficiency of nitric oxide synthase 2 protects against endotoxin-induced myocardial dysfunction in mice. Circulation. 2000;102:1440–6.
Grandel U, Sibelius U, Schrickel J, et al. Biosynthesis of constitutive nitric oxide synthase-derived nitric oxide attenuates coronary vasoconstriction and myocardial depression in a model of septic heart failure induced by Staphylococcus aureus alpha-toxin. Crit Care Med. 2001;29:1–7.
Belcher E, Mitchell J, Evans T. Myocardial dysfunction in sepsis: no role for NO? Heart. 2002;87:507–9.
Annane D, Sebille V, Charpentier C, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2002;288:862–71.
Shenker Y, Skatrud JB. Adrenal insufficiency in critically ill patients. Am J Respir Crit Care Med. 2001;163:1520–3.
Annane D, Sebille V, Troche G, et al. A 3-level prognostic classification in septic shock based on cortisol levels and cortisol response to corticotropin. JAMA. 2000;283:1038–45.
Sonneville R, Guidoux C, Barrett L, et al. Vasopressin synthesis by the magnocellular neurons is different in the supraoptic nucleus and in the paraventricular nucleus in human and experimental septic shock. Brain Pathol. 2010;20:613–22.
Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–96.
Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38:1045–53.
Ibrahim EH, Sherman G, Ward S, et al. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118:146–55.
Kollef MH, Sherman G, Ward S, et al. Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest. 1999;115:462–74.
Dellinger RP, Carlet JM, Masur H, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32:858–73.
Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327.
Balogh Z, Moore FA, Moore EE, et al. Secondary abdominal compartment syndrome: a potential threat for all trauma clinicians. Injury. 2007;38:272–9.
Coats TJ, Brazil E, Heron M, et al. Impairment of coagulation by commonly used resuscitation fluids in human volunteers. Emerg Med J. 2006;23:846–9.
Krausz MM. Initial resuscitation of hemorrhagic shock. World J Emerg Surg. 2006;1:14.
Wiedemann HP, Wheeler AP, Bernard GR, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–75.
Wheeler AP, Bernard GR, Thompson BT, et al. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med. 2006;354:2213–24.
Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest. 2002;121:2000–8.
Barbier C, Loubieres Y, Schmit C, et al. Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med. 2004;30:1740–6.
Perel A. Automated assessment of fluid responsiveness in mechanically ventilated patients. Anesth Analg. 2008;106:1031–3.
Kaplan LJ, Kellum JA. Initial pH, base deficit, lactate, anion gap, strong ion difference, and strong ion gap predict outcome from major vascular injury. Crit Care Med. 2004;32:1120–4.
Zornow MH, Prough DS. Fluid management in patients with traumatic brain injury. New Horiz. 1995;3:488–98.
Santry HP, Alam HB. Fluid resuscitation: past, present, and the future. Shock. 2010;33:229–41.
Vincent JL: Fluid resuscitation: colloids vs crystalloids. Acta Clin Belg Suppl. 2007;408-11.
Jaskille A, Alam HB, Rhee P, et al.: D-lactate increases pulmonary apoptosis by restricting phosphorylation of bad and eNOS in a rat model of hemorrhagic shock. J Trauma. 2004;57:262-69; discussion 269-70.
Ayuste EC, Chen H, Koustova E, et al. Hepatic and pulmonary apoptosis after hemorrhagic shock in swine can be reduced through modifications of conventional Ringer's solution. J Trauma. 2006;60:52–63.
Investigators SS. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350:2247–56.
Finfer S, McEvoy S, Bellomo R, et al. Impact of albumin compared to saline on organ function and mortality of patients with severe sepsis. Intensive Care Med. 2011;37:86–96.
McIntyre LA, Fergusson D, Cook DJ, et al. Resuscitating patients with early severe sepsis: a Canadian multicentre observational study. Can J Anaesth. 2007;54:790–8.
McIntyre L, Fergusson DA, Rowe B, et al. The PRECISE RCT: Evolution of an Early Septic Shock Fluid Resuscitation Trial. Transfus Med Rev. 2012.
Mortelmans Y, Merckx E, van Nerom C, et al. Effect of an equal volume replacement with 500 mL 6% hydroxyethyl starch on the blood and plasma volume of healthy volunteers. Eur J Anaesthesiol. 1995;12:259–64.
Nagy KK, Davis J, Duda J, et al. A comparison of pentastarch and lactated Ringer's solution in the resuscitation of patients with hemorrhagic shock. Circ Shock. 1993;40:289–94.
Claes Y, Van Hemelrijck J, Van Gerven M, et al. Influence of hydroxyethyl starch on coagulation in patients during the perioperative period. Anesth Analg. 1992;75:24–30.
Brunkhorst FM, Engel C, Bloos F, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39.
Sakr Y, Payen D, Reinhart K, et al. Effects of hydroxyethyl starch administration on renal function in critically ill patients. Br J Anaesth. 2007;98:216–24.
Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl Starch 130/0.4 versus Ringer's Acetate in Severe Sepsis. N Engl J Med. 2012.
Shander A, Javidroozi M, Ozawa S, et al. What is really dangerous: anaemia or transfusion? Br J Anaesth. 2011;107 Suppl 1:i41–59.
Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med. 1999;340:409–17.
Levi M, Toh CH, Thachil J, et al. Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for Standards in Haematology. Br J Haematol. 2009;145:24–33.
Wallis JP. Editorial I: transfusion-related acute lung injury (TRALI)—under-diagnosed and under-reported. Br J Anaesth. 2003;90:573–6.
Toy P, Gajic O, Bacchetti P, et al. Transfusion-related acute lung injury: incidence and risk factors. Blood. 2012;119:1757–67.
De Backer D, Creteur J, Silva E, et al. Effects of dopamine, norepinephrine, and epinephrine on the splanchnic circulation in septic shock: which is best? Crit Care Med. 2003;31:1659–67.
De Backer D, Biston P, Devriendt J, et al. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med. 2010;362:779–89.
Hsu JL. Personal Communication. 2012.
Dunser MW, Mayr AJ, Ulmer H, et al. Arginine vasopressin in advanced vasodilatory shock: a prospective, randomized, controlled study. Circulation. 2003;107:2313–9.
Traber D. Selective V1a receptor agonists in experimental septic shock. Crit Care. 2007;11:P51.
•• Rehberg S, Ertmer C, Vincent JL, et al. Role of selective V1a receptor agonism in ovine septic shock. Crit Care Med. 2011;39:119–25. This study opens the possibility to new therapuetic targets in septic shock management: vasopressin analogues that are V1 receptor selective. In a fecal peritonitis-induced septic shock animal model an experimental V1 agonist showed better hemodynamics, vascular leak and mortality when compared to standard treatment (vasopressin and single norepinephrine infusion).
Annane D, Vignon P, Renault A, et al. Norepinephrine plus dobutamine versus epinephrine alone for management of septic shock: a randomised trial. Lancet. 2007;370:676–84.
Leone M, Martin C. Vasopressor use in septic shock: an update. Curr Opin Anaesthesiol. 2008;141-7.
Antonopoulos A, Nikolopoulos D, Georgiou EK, et al. Blood pressure elevation after phenylephrine infusion may adversely affect myocardial perfusion in patients with coronary artery disease. Int J Cardiol. 2002;84:201–9.
Morelli A, Ertmer C, Rehberg S, et al. Phenylephrine versus norepinephrine for initial hemodynamic support of patients with septic shock: a randomized, controlled trial. Crit Care. 2008;12:R143.
Beale RJ, Hollenberg SM, Vincent JL, et al. Vasopressor and inotropic support in septic shock: an evidence-based review. Crit Care Med. 2004;32:S455–65.
• Annane D, Bellissant E, Bollaert PE, et al. Corticosteroids in the treatment of severe sepsis and septic shock in adults: a systematic review. JAMA. 2009;301:2362–75. After contradictory randomized trials, this meta-analysis was published showing that low-dose treatment with corticosteroids may be beneficial in severe sepsis and septic shock. The right answer for use of steroids is still a matter of debate.
Dellinger RP. Steroid therapy of septic shock: the decision is in the eye of the beholder. Crit Care Med. 2008;36:1987–9.
Acknowledgement
The authors wish to acknowledge the significant contributions of Christina Lum during the preparation of the manuscript.
Disclosure
Dr. A. Patterson has served on the American Board of Anesthesiology Board of Directors and has worked as a consultant for Dickie, McCamey and Chilcote PC.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guillamet, M.C.V., Rhee, C. & Patterson, A.J. Cardiovascular Management of Septic Shock in 2012. Curr Infect Dis Rep 14, 493–502 (2012). https://doi.org/10.1007/s11908-012-0279-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11908-012-0279-z