Abstract
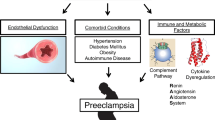
Preeclampsia is a pregnancy-specific syndrome characterized by renal dysfunction and high blood pressure. When evaluated with light microscopy, the renal lesion of preeclampsia is marked by endothelial cell swelling and the appearance of bloodless glomeruli. However, regarding the pathobiology of renal damage in preeclampsia, attention recently has shifted from the glomerular endothelial cells to the podocytes. The angiogenic imbalance in preeclampsia plays a key role in the development of both podocyte and endothelial damage in the glomerular filtration barrier. Here, we review the latest studies on the role of podocytes in the development of renal damage in preeclampsia and on podocytes as potential targets for diagnosis, treatment, and prevention of long-term complications of preeclampsia.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
von Schmidt auf Altenstadt JF, Hukkelhoven CW, van Roosmalen J, Bloemenkamp KW. Pre-eclampsia increases the risk of postpartum haemorrhage: a nationwide cohort study in the Netherlands. PLoS ONE. 2013;8(12):e81959. doi:10.1371/journal.pone.0081959.
Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367(9516):1066–74.
Gillon TE, Pels A, von Dadelszen P, MacDonell K, Magee LA. Hypertensive disorders of pregnancy: a systematic review of international clinical practice guidelines. PLoS ONE. 2014;9(12):e113715. doi:10.1371/journal.pone.0113715.
Myers JE, Kenny LC, McCowan LM, Chan EH, Dekker GA, Poston L, et al. Angiogenic factors combined with clinical risk factors to predict preterm pre-eclampsia in nulliparous women: a predictive test accuracy study. Bjog. 2013;120(10):1215–23.
Hussein W, Lafayette RA. Renal function in normal and disordered pregnancy. Curr Opin Nephrol Hypertens. 2014;23(1):46–53.
Spargo B, McCartney CP, Winemiller R. Glomerular capillary endotheliosis in toxemia of pregnancy. Arch Pathol. 1959;68:593–9.
Gartner HV, Sammoun A, Wehrmann M, Grossmann T, Junghans R, Weihing C. Preeclamptic nephropathy—an endothelial lesion. A morphological study with a review of the literature. Eur J Obstet Gynecol Reprod Biol. 1998;77(1):11–27.
Cagnoli L, Casanova S, Pasquali S. Correlations between glomerular epithelial changes and proteinuria in different glomerular diseases. [Italian]. Minerva Nefrol. 1980;27(1):155–8.
Buurma AJ, Penning ME, Prins F, Schutte JM, Bruijn JA, Wilhelmus S, et al. Preeclampsia is associated with the presence of transcriptionally active placental fragments in the maternal lung. Hypertension. 2013;62(3):608–13.
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003;111(5):649–58.
Venkatesha S, Toporsian M, Lam C, Hanai J, Mammoto T, Kim YM, et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med. 2006;12(6):642–9.
Sugimoto H, Hamano Y, Charytan D, Cosgrove D, Kieran M, Sudhakar A, et al. Neutralization of circulating vascular endothelial growth factor (VEGF) by anti-VEGF antibodies and soluble VEGF receptor 1 (sFlt-1) induces proteinuria. J Biol Chem. 2003;278(15):12605–8.
Eremina V, Sood M, Haigh J, Nagy A, Lajoie G, Ferrara N, et al. Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases. J Clin Invest. 2003;111(5):707–16.
Vigneau C, Lorcy N, Dolley-Hitze T, Jouan F, Arlot-Bonnemains Y, Laguerre B, et al. All anti-vascular endothelial growth factor drugs can induce ‘pre-eclampsia-like syndrome’: a RARe study. Nephrol Dial Transplant. 2014;29(2):325–32.
Muller-Deile J, Schiffer M. Renal involvement in preeclampsia: similarities to VEGF ablation therapy. J Pregnancy. 2011;2011:176973. doi:10.1155/2011/.
Usui J, Glezerman IG, Salvatore SP, Chandran CB, Flombaum CD, Seshan SV. Clinicopathological spectrum of kidney diseases in cancer patients treated with vascular endothelial growth factor inhibitors: a report of 5 cases and review of Literature. Hum Pathol. 2014;45(9):1918–27.
Eremina V, Jefferson JA, Kowalewska J, Hochster H, Haas M, Weisstuch J, et al. VEGF inhibition and renal thrombotic microangiopathy. N Engl J Med. 2008;358(11):1129–36.
Veron D, Villegas G, Aggarwal PK, Bertuccio C, Jimenez J, Velazquez H, et al. Acute podocyte vascular endothelial growth factor (VEGF-A) knockdown disrupts alphaVbeta3 integrin signaling in the glomerulus. PLoS ONE. 2012;7(7):e40589. doi:10.1371/journal.pone.0040589. This study describes an inducible podocyte-specific VEGF-A knockdown mouse model. Podocyte-specific VEGF-A knockdown results in endothelial cell swelling and podocyte foot process effacement in vivo. VEGF-A knockdown also leads to decreased alphaVbeta3 integrin signaling, an integrin essential for the withstanding of mechanical stress by the podocyte.
Sison K, Eremina V, Baelde H, Min W, Hirashima M, Fantus IG, et al. Glomerular structure and function require paracrine, not autocrine, VEGF-VEGFR-2 signaling. J Am Soc Nephrol. 2010;21(10):1691–701.
Kamba T, Tam BY, Hashizume H, Haskell A, Sennino B, Mancuso MR, et al. VEGF-dependent plasticity of fenestrated capillaries in the normal adult microvasculature. Am J Physiol Heart Circ Physiol. 2006;290(2):H560–76.
Zhao J, Liu H, Du H, Qiao F, Li Y, Shi X, et al. Upregulation of sFlt-1 by trophoblasts induces the barrier dysfunction of glomerular endothelial cells. J Huazhong Univ Sci Technol Med Sci. 2011;31(6):815–8.
Wang L, Zhang T, Fang M, Shen N, Wang D, Teng J, et al. Podocytes protect glomerular endothelial cells from hypoxic injury via deSUMOylation of HIF-1alpha signaling. Int J Biochem Cell Biol. 2015;58:17–27.
Veron D, Reidy KJ, Bertuccio C, Teichman J, Villegas G, Jimenez J, et al. Overexpression of VEGF-A in podocytes of adult mice causes glomerular disease. Kidney Int. 2010;77(11):989–99.
Ku CH, White KE, Dei Cas A, Hayward A, Webster Z, Bilous R, et al. Inducible overexpression of sFlt-1 in podocytes ameliorates glomerulopathy in diabetic mice. Diabetes. 2008;57(10):2824–33.
Ostalska-Nowicka D, Malinska A, Zabel M, Witkiewicz W, Nowicki M. Nephrotic syndrome unfavorable course correlates with downregulation of podocyte vascular endothelial growth factor receptor (VEGFR)-2. Folia Histochem Cytobiol. 2011;49(3):472–8.
Hohenstein B, Colin M, Foellmer C, Amann KU, Brekken RA, Daniel C, et al. Autocrine VEGF-VEGF-R loop on podocytes during glomerulonephritis in humans. Nephrol Dial Transplant. 2010;25(10):3170–80.
Bertuccio C, Veron D, Aggarwal PK, Holzman L, Tufro A. Vascular endothelial growth factor receptor 2 direct interaction with nephrin links VEGF-A signals to actin in kidney podocytes. J Biol Chem. 2011;286(46):39933–44.
Kestila M, Lenkkeri U, Mannikko M, Lamerdin J, McCready P, Putaala H, et al. Positionally cloned gene for a novel glomerular protein—nephrin—is mutated in congenital nephrotic syndrome. Mol Cell. 1998;1(4):575–82.
Baelde HJ, Eikmans M, Lappin DW, Doran PP, Hohenadel D, Brinkkoetter PT, et al. Reduction of VEGF-A and CTGF expression in diabetic nephropathy is associated with podocyte loss. Kidney Int. 2007;71(7):637–45.
Thilo F, Liu Y, Loddenkemper C, Schuelein R, Schmidt A, Yan Z, et al. VEGF regulates TRPC6 channels in podocytes. Nephrol Dial Transplant. 2012;27(3):921–9. This study investigates the regulatory effect of VEGF on TRPC6, a calcium ion channel found on podocyte foot processes and the slit diaphragms. VEGF165 significantly increases TRPC6 mRNA and protein levels, indicating that VEGF regulates podocyte structure via the expression of TRPC6.
Li SY, Huang PH, Yang AH, Tarng DC, Yang WC, Lin CC, et al. Matrix metalloproteinase-9 deficiency attenuates diabetic nephropathy by modulation of podocyte functions and dedifferentiation. Kidney Int. 2014;86(2):358–69.
Wang H, Misaki T, Taupin V, Eguchi A, Ghosh P, Farquhar MG. GIV/girdin links vascular endothelial growth factor signaling to Akt survival signaling in podocytes independent of nephrin. J Am Soc Nephrol. 2015;26(2):314–27.
Jin J, Sison K, Li C, Tian R, Wnuk M, Sung HK, et al. Soluble FLT1 binds lipid microdomains in podocytes to control cell morphology and glomerular barrier function. Cell. 2012;151(2):384–99. This study discovered the presence of a podocytal autocrine sFlt-1 loop in vitro and in a mouse model. sFlt-1 knockdown in mice resulted in podocytal flattening, cytoskeletal rearrangements and proteinuria. In vitro, sFlt-1 binds to lipid rafts and co-localizes with nephrin.
Garovic VD, Wagner SJ, Petrovic LM, Gray CE, Hall P, Sugimoto H, et al. Glomerular expression of nephrin and synaptopodin, but not podocin, is decreased in kidney sections from women with preeclampsia. Nephrol Dial Transplant. 2007;22(4):1136–43.
Zhao S, Gu X, Groome LJ, Wang Y. Decreased nephrin and GLEPP-1, but increased VEGF, Flt-1, and nitrotyrosine, expressions in kidney tissue sections from women with preeclampsia. Reprod Sci. 2009;16(10):970–9.
Zhao S, Gu Y, Coates G, Groome LJ, Saleem MA, Mathieson PW, et al. Altered nephrin and podoplanin distribution is associated with disturbed polarity protein PARD-3 and PARD-6 expressions in podocytes from preeclampsia. Reprod Sci. 2011;18(8):772–80.
Henao DE, Arias LF, Mathieson PW, Ni L, Welsh GI, Bueno JC, et al. Preeclamptic sera directly induce slit-diaphragm protein redistribution and alter podocyte barrier-forming capacity. Nephron Exp Nephrol. 2008;110(3):e73–81.
Henao DE, Cadavid AP, Saleem MA. Exogenous vascular endothelial growth factor supplementation can restore the podocyte barrier-forming capacity disrupted by sera of preeclamptic women. J Obstet Gynaecol Res. 2013;39(1):46–52. In this study human cultured podocytes were exposed to sera from preeclamptic women and healthy pregnant women. Sera from preeclamptic women contained more sFlt-1 and less VEGF and disrupted podocyte barrier-forming capacity. Adding VEGF to these sera attenuated this effect.
Kriz W, Shirato I, Nagata M, LeHir M, Lemley KV. The podocyte’s response to stress: the enigma of foot process effacement. Am J Physiol Renal Physiol. 2013;304(4):F333–47.
Collino F, Bussolati B, Gerbaudo E, Marozio L, Pelissetto S, Benedetto C, et al. Preeclamptic sera induce nephrin shedding from podocytes through endothelin-1 release by endothelial glomerular cells. Am J Physiol Renal Physiol. 2008;294(5):F1185–94.
Eyre J, Burton JO, Saleem MA, Mathieson PW, Topham PS, Brunskill NJ. Monocyte- and endothelial-derived microparticles induce an inflammatory phenotype in human podocytes. Nephron Exp Nephrol. 2011;119(3):e58–66.
Henao DE, Saleem MA. Proteinuria in preeclampsia from a podocyte injury perspective. Curr Hypertens Rep. 2013;15(6):600–5.
Buurma A, Cohen D, Veraar K, Schonkeren D, Claas FH, Bruijn JA, et al. Preeclampsia is characterized by placental complement dysregulation. Hypertension. 2012;60(5):1332–7.
Lynch AM, Murphy JR, Byers T, Gibbs RS, Neville MC, Giclas PC, et al. Alternative complement pathway activation fragment Bb in early pregnancy as a predictor of preeclampsia. Am J Obstet Gynecol. 2008;198(4):385.e1–9.
Penning ME, Chua JS, van Kooten C, Zandbergen M, Buurma A, Schutte JM et al. Classical complement pathway activation in the kidneys of women with preeclampsia. Hypertension. 2015:Accepted for publication.
Burwick RM, Easter SR, Dawood HY, Yamamoto HS, Fichorova RN, Feinberg BB. Complement activation and kidney injury molecule-1-associated proximal tubule injury in severe preeclampsia. Hypertension. 2014;64(4):833–8.
Burwick RM, Fichorova RN, Dawood HY, Yamamoto HS, Feinberg BB. Urinary excretion of C5b-9 in severe preeclampsia: tipping the balance of complement activation in pregnancy. Hypertension. 2013;62(6):1040–5.
Wang W, Irani RA, Zhang Y, Ramin SM, Blackwell SC, Tao L, et al. Autoantibody-mediated complement C3a receptor activation contributes to the pathogenesis of preeclampsia. Hypertension. 2012;60(3):712–21.
Hayman SR, Calle JC, Jatoi A, Craici IM, Wagner SJ, Weaver AL, et al. Urinary podocyte excretion and proteinuria in patients treated with antivascular endothelial growth factor therapy for solid tumor malignancies. Oncology. 2014;86(5–6):271–8.
Bhide A, Rana R, Dhavilkar M, Amodio-Hernandez M, Deshpande D, Caric V. The value of the urinary protein: creatinine ratio for the detection of significant proteinuria in women with suspected preeclampsia. Acta Obstet Gynecol Scand. 2015. doi:10.1111/aogs.12624.
Garovic VD. The role of the podocyte in preeclampsia. Clin J Am Soc Nephrol. 2014;9(8):1337–40.
Yu D, Petermann A, Kunter U, Rong S, Shankland SJ, Floege J. Urinary podocyte loss is a more specific marker of ongoing glomerular damage than proteinuria. J Am Soc Nephrol. 2005;16(6):1733–41.
Garovic VD, Wagner SJ, Turner ST, Rosenthal DW, Watson WJ, Brost BC. Urinary podocyte excretion as a marker for preeclampsia. Am J Obstet Gynecol. 2007;196(4):320 e1–7.
Craici IM, Wagner SJ, Bailey KR, Fitz-Gibbon PD, Wood-Wentz CM, Turner ST, et al. Podocyturia predates proteinuria and clinical features of preeclampsia: longitudinal prospective study. Hypertension. 2013;61(6):1289–96.
Kelder TP, Penning ME, Uh HW, Cohen D, Bloemenkamp KW, Bruijn JA, et al. Quantitative polymerase chain reaction-based analysis of podocyturia is a feasible diagnostic tool in preeclampsia. Hypertension. 2012;60(6):1538–44. In this study a new method for the detection of podocyturia is presented. Urine samples from preeclamptic women, healthy controls and women with gestational hypertension were collected and qPCR for VEGF, podocin and nephrin mRNA was performed. qPCR of these podocyte-specific molecules distinguished preeclamptic patients from healthy and hypertensive controls and is a rapid tool for the detection of podocytes in urine.
Eremina V, Baelde HJ, Quaggin SE. Role of the VEGF-A signaling pathway in the glomerulus: evidence for crosstalk between components of the glomerular filtration barrier. Nephron Physiol. 2007;106(2):32–7.
Chen DB, Zheng J. Regulation of placental angiogenesis. Microcirculation. 2014;21(1):15–25.
Mathieson PW. The podocyte as a target for therapies–new and old. Nat Rev Nephrol. 2012;8(1):52–6.
Wada T, Pippin JW, Marshall CB, Griffin SV, Shankland SJ. Dexamethasone prevents podocyte apoptosis induced by puromycin aminonucleoside: role of p53 and Bcl-2-related family proteins. J Am Soc Nephrol. 2005;16(9):2615–25.
Fujii Y, Khoshnoodi J, Takenaka H, Hosoyamada M, Nakajo A, Bessho F, et al. The effect of dexamethasone on defective nephrin transport caused by ER stress: a potential mechanism for the therapeutic action of glucocorticoids in the acquired glomerular diseases. Kidney Int. 2006;69(8):1350–9.
Macconi D, Sangalli F, Bonomelli M, Conti S, Condorelli L, Gagliardini E, et al. Podocyte repopulation contributes to regression of glomerular injury induced by ACE inhibition. Am J Pathol. 2009;174(3):797–807.
Friedman JM. ACE inhibitors and congenital anomalies. N Engl J Med. 2006;354(23):2498–500.
Sakurai N, Kuroiwa T, Ikeuchi H, Hiramatsu N, Takeuchi S, Tomioka M, et al. Fluvastatin prevents podocyte injury in a murine model of HIV-associated nephropathy. Nephrol Dial Transplant. 2009;24(8):2378–83.
Ramma W, Ahmed A. Therapeutic potential of statins and the induction of heme oxygenase-1 in preeclampsia. J Reprod Immunol. 2014;101–102:153–60.
Lefkou E, Mamopoulos A, Fragakis N, Dagklis T, Vosnakis C, Nounopoulos E, et al. Clinical improvement and successful pregnancy in a preeclamptic patient with antiphospholipid syndrome treated with pravastatin. Hypertension. 2014;63(5):e118–9.
Morton S, Thangaratinam S. Statins in pregnancy. Curr Opin Obstet Gynecol. 2013;25(6):433–40.
Fukusumi Y, Miyauchi N, Hashimoto T, Saito A, Kawachi H. Therapeutic target for nephrotic syndrome: Identification of novel slit diaphragm associated molecules. World J Nephrol. 2014;3(3):77–84.
He FF, Chen S, Su H, Meng XF, Zhang C. Actin-associated proteins in the pathogenesis of podocyte injury. Curr Genom. 2013;14(7):477–84.
Arif E, Rathore YS, Kumari B, Ashish F, Wong HN, Holzman LB, et al. Slit diaphragm protein Neph1 and its signaling: a novel therapeutic target for protection of podocytes against glomerular injury. J Biol Chem. 2014;289(14):9502–18. This study shows that Neph1 signaling inhibition prevents podocyte damage in vivo and in vitro in PAN and adriamycine renal injury models. Inhibition of Neph1 phosphorylation prevents mislocalization of Neph1 and maintains the normal cytoskeletal structure in podocytes.
McDonald SD, Han Z, Walsh MW, Gerstein HC, Devereaux PJ. Kidney disease after preeclampsia: a systematic review and meta-analysis. Am J Kidney Dis. 2010;55(6):1026–39.
Wang IK, Muo CH, Chang YC, Liang CC, Chang CT, Lin SY, et al. Association between hypertensive disorders during pregnancy and end-stage renal disease: a population-based study. Cmaj. 2013;185(3):207–13.
Vikse BE, Irgens LM, Karumanchi SA, Thadhani R, Reisaeter AV, Skjaerven R. Familial factors in the association between preeclampsia and later ESRD. Clin J Am Soc Nephrol. 2012;7(11):1819–26. This large study using the Norwegian Population Registry shows that the increased risk of end-stage renal disease after preeclampsia is not explained by familial aggregation of risk factors, but that the preeclampsia itself probably leads to kidney damage.
Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM. Preeclampsia and the risk of end-stage renal disease. N Engl J Med. 2008;359(8):800–9.
Mundel P, Shankland SJ. Podocyte biology and response to injury. J Am Soc Nephrol. 2002;13(12):3005–15.
Hara M, Yanagihara T, Kihara I. Urinary podocytes in primary focal segmental glomerulosclerosis. Nephron. 2001;89(3):342–7.
Vikse BE, Hallan S, Bostad L, Leivestad T, Iversen BM. Previous preeclampsia and risk for progression of biopsy-verified kidney disease to end-stage renal disease. Nephrol Dial Transplant. 2010;25(10):3289–96.
White WM, Garrett AT, Craici IM, Wagner SJ, Fitz-Gibbon PD, Butters KA, et al. Persistent urinary podocyte loss following preeclampsia may reflect subclinical renal injury. PLoS ONE. 2014;9(3):e92693. doi:10.1371/journal.pone.0092693. In this study urine samples from women with preeclampsia and normotensive pregnant women were collected from 24 hours before up to five to eight weeks after delivery. Altough proteinuria normalized postpartum, three out of ten preeclampsia patients still had podocyturia postpartum whereas normotensive women had no podocyturia.
Appel D, Kershaw DB, Smeets B, Yuan G, Fuss A, Frye B, et al. Recruitment of podocytes from glomerular parietal epithelial cells. J Am Soc Nephrol. 2009;20(2):333–43.
Hakroush S, Cebulla A, Schaldecker T, Behr D, Mundel P, Weins A. Extensive podocyte loss triggers a rapid parietal epithelial cell response. J Am Soc Nephrol. 2014;25(5):927–38.
Smeets B, Kuppe C, Sicking EM, Fuss A, Jirak P, van Kuppevelt TH, et al. Parietal epithelial cells participate in the formation of sclerotic lesions in focal segmental glomerulosclerosis. J Am Soc Nephrol. 2011;22(7):1262–74.
Penning ME, Bloemenkamp KW, van der Zon T, Zandbergen M, Schutte JM, Bruijn JA, et al. Association of preeclampsia with podocyte turnover. Clin J Am Soc Nephrol. 2014;9(8):1377–85. In this study, renal samples from women with preeclampsia and pregnant controls were collected from the nationwide Dutch pathology database PALGA. Endotheliosis was not associated with preeclampsia, but increased podocyte turnover and activation of parietal epithelial cells were.
Schleidgen S, Klingler C, Bertram T, Rogowski WH, Marckmann G. What is personalized medicine: sharpening a vague term based on a systematic literature review. BMC Med Ethics. 2013;14:55.
Kenny LC, Broadhurst DI, Dunn W, Brown M, North RA, McCowan L, et al. Robust early pregnancy prediction of later preeclampsia using metabolomic biomarkers. Hypertension. 2010;56(4):741–9.
Myers JE, Tuytten R, Thomas G, Laroy W, Kas K, Vanpoucke G, et al. Integrated proteomics pipeline yields novel biomarkers for predicting preeclampsia. Hypertension. 2013;61(6):1281–8.
Navaratnam K, Alfirevic Z, Baker PN, Gluud C, Gruttner B, Kublickiene K, et al. A multi-centre phase IIa clinical study of predictive testing for preeclampsia: improved pregnancy outcomes via early detection (IMPROvED). BMC Pregnancy Childbirth. 2013;13:226.
Compliance with Ethics Guidelines
Conflict of Interest
Rosanne J. Turner, Kitty W.M. Bloemenkamp, Marlies E. Penning, Jan Anthonie Bruijn, and Hans J. Baelde declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Preeclampsia
Rights and permissions
About this article
Cite this article
Turner, R.J., Bloemenkamp, K.W.M., Penning, M.E. et al. From Glomerular Endothelium to Podocyte Pathobiology in Preeclampsia: a Paradigm Shift. Curr Hypertens Rep 17, 54 (2015). https://doi.org/10.1007/s11906-015-0566-9
Published:
DOI: https://doi.org/10.1007/s11906-015-0566-9