Abstract
Hypertension is a common disorder linked to increases in cardiovascular mortality and morbidity. Effective treatment decreases this excess mortality. Therapy with a single antihypertensive agent fails to achieve blood pressure goals in up to 75 % of patients. Compared to monotherapy, combination antihypertensive therapy, especially with fixed-dose (single pill) formulations, may more effectively control blood pressure and improve medication persistence while decreasing adverse effects, healthcare costs, and physician therapeutic inertia. Certain combinations, such as a calcium channel blocker and angiotensin converting enzyme inhibitor, have been associated with similar or fewer adverse effects and better outcomes than other combinations. In contrast, other combinations such as thiazide diuretics and β-blockers may cause more adverse effects than monotherapy. When choosing a thiazide diuretic, chlorthalidone is preferable to hydrochlorothiazide, given better efficacy and cardiovascular outcomes. Initial combination antihypertensive therapy may benefit patients with stage I or II hypertension and more widespread use should be encouraged.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ong KL, Cheung BM, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75.
Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
Staessen JA, Li Y, Thijs L, Wang JG. Blood pressure reduction and cardiovascular prevention: an update including the 2003–2004 secondary prevention trials. Hypertens Res. 2005;28:385–407.
Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–72.
Rosenthal T, Gavras I. Fixed-drug combinations as first-line treatment for hypertension. Prog Cardiovasc Dis. 2006;48:416–25.
•• Gradman AH, Basile JN, Carter BL, et al. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4:42–50. This position paper from the American Society of Hypertension regarding combination anti-hypertensive therapy recommended routine use of combination therapy in “most” patients with hypertension.
Cushman WC, Ford CE, Cutler JA, et al. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). J Clin Hypertens (Greenwich). 2002;4:393–404.
•• Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–85. This paper reports the results of the ACCORD-BP trial, which randomized diabetic hypertensives to intense (SBP <120) versus standard (SBP <140) blood pressure control. The study did not show a difference between the two groups in CV outcomes, although a lower-than-expected event rate possibly confounded the results.
Neutel JM. Prescribing patterns in hypertension: the emerging role of fixed-dose combinations for attaining BP goals in hypertensive patients. Curr Med Res Opin. 2008;24:2389–401.
Hill MN, Miller NH, Degeest S, et al. Adherence and persistence with taking medication to control high blood pressure. J Am Soc Hypertens. 2011;5:56–63.
Okonofua EC, Simpson KN, Jesri A, et al. Therapeutic inertia is an impediment to achieving the Healthy People 2010 blood pressure control goals. Hypertension. 2006;47:345–51.
•• Feldman RD, Zou GY, Vandervoort MK, et al. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension. 2009;53:646–53. The STITCH trial randomized primary care practices to guideline care versus a simplified algorithm using fixed-dose combinations and a proscribed titration schedule. BP control was improved at 6 months in the algorithm arm compared to the guideline arm.
Wald DS, Law M, Morris JK, et al. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122:290–300.
Neutel JM, Smith DH, Weber MA, et al. Efficacy of combination therapy for systolic blood pressure in patients with severe systolic hypertension: The Systolic Evaluation of Lotrel Efficacy and Comparative Therapies (SELECT) Study. J Clin Hypertens. 2005;7:641–6.
Neutel JM, Smith DH, Weber MA. Effect of antihypertensive monotherapy and combination therapy on arterial distensibility and left ventricular mass. Am J Hypertens. 2004;17:37–42.
Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326:1427.
Messerli FH, Oparil S, Feng Z. Comparison of efficacy and side effects of combination therapy of angiotensin-converting enzyme inhibitor (benazepril) with calcium antagonist (either nifedipine or amlodipine) versus high-dose calcium antagonist monotherapy for systemic hypertension. Am J Cardiol. 2000;86:1182–7.
Makani H, Bangalore S, Romero J, et al. Effect of renin-angiotensin system blockade on calcium channel blocker-associated peripheral edema. Am J Med. 2011;124:128–35.
Sever PS, Messerli FH. Hypertension management 2011: Optimal combination therapy. Eur Heart J. 2011;32:2499–506.
Weber MA, Julius S, Kjeldsen SE, et al. Blood pressure dependent and independent effects of antihypertensive treatment on clinical events in the VALUE Trial. Lancet. 2004;363:2049–51.
Byrd JB, Zeng C, Tavel HM, et al. Combination therapy as initial treatment for newly diagnosed hypertension. Am Heart J. 2011;162:340–6.
• Corrao G, Nicotra F, Parodi A, et al. Cardiovascular protection by initial and subsequent combination of antihypertensive drugs in daily life practice. Hypertension. 2011;58:566–72. This case controlled study compared initial combination antihypertensive therapy with initial monotherapy in patients without a history of CV disease. The study showed an 11 % reduction in CV events in patients started on combination therapy compared to those started on monotherapy.
Kotchen TA. Expanding role for combination drug therapy in the initial treatment of hypertension? Hypertension. 2011;58:550–1.
Jamerson K, Weber MA, Bakris GL, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359:2417–28.
• Bakris GL, Sica D, Weber M, et al. The comparative effects of azilsartan medoxomil and olmesartan on ambulatory and clinic blood pressure. J Clin Hypertens (Greenwich). 2011;13:81–8. This randomized controlled trial compared azilsartan with olmesartan and placebo in patients with hypertension. BP-lowering efficacy was assessed as change in baseline in mean 24-hour ambulatory systolic blood pressure. BP reduction with azilsartan was greater than with placebo; azilsartan 40 mg was non-inferior to olmesartan 40 mg, but azilsartan 80 mg reduced mean 24-hour SBP more than olmesartan 40 mg.
Heartwire: Azilsartan/chlorthalidone combo bests olmesartan/HCTZ in stage 2 systolic hypertension. Available at: http://www.theheart.org/article/1230773.do. Accessed April 2012.
ADVANCE Collaborative Group. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370:829–40.
Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–98.
PROGRESS Collaborative Study Group. Randomised trial of perindopril based blood pressure-lowering regimen among 6108 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033–41.
Ernst ME, Lund BC. Renewed interest in chlorthalidone: evidence from the Veterans Health Administration. J Clin Hypertens (Greenwich). 2010;12:927–34.
•• Messerli FH, Makani H, Benjo A, et al. Antihypertensive efficacy of hydrochlorothiazide as evaluated by ambulatory blood pressure monitoring: a meta-analysis of randomized trials. J Am Coll Cardiol. 2011;57:590–600. This meta-analysis of randomized trials compared HCTZ with other anti-hypertensive agents, using ambulatory blood pressure as the outcome. HCTZ at doses of 12.5 mg and 25 mg was less effective at lowering 24-hour blood pressure than ACEIs, ARBs, β-blockers, or CCBs.
Messerli FH, Bangalore S. Half a century of hydrochlorothiazide: facts, fads, fiction, and follies. Am J Med. 2011;124:896–9.
SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265:3255–64.
Ernst ME, Carter BL, Zheng S, Grimm RH. Meta-analysis of dose–response characteristics of hydrochlorothiazide and chlorthalidone: Effects on systolic blood pressure and potassium. Am J Hypertens. 2010;23:440–6.
Carter BL, Ernst ME, Cohen JD. Hydrochlorothiazide versus chlorthalidone: evidence supporting their interchangeability. Hypertension. 2004;43:4–9.
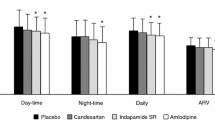
Ernst ME, Carter BL, Goerdt CJ, et al. Comparative antihypertensive effects of hydrochlorothiazide and chlorthalidone on ambulatory and office blood pressure. Hypertension. 2006;47:352–8.
Fagard RH, Celis H, Thijs L, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008;51:55–61.
Clement DL, De Buyzere ML, De Bacquer DA, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med. 2003;348:2407–15.
Multiple Risk Factor Intervention Trial Research Group. Mortality after 10 1/2 years for hypertensive participants in the Multiple Risk Factor Intervention Trial. Circulation. 1990;82:1616–28.
Ernst ME, Neaton JD, Grimm Jr RH, et al. Long-term effects of chlorthalidone versus hydrochlorothiazide on electrocardiographic left ventricular hypertrophy in the multiple risk factor intervention trial. Hypertension. 2011;58:1001–7.
Dorsch MP, Gillespie BW, Erickson SR, et al. Chlorthalidone reduces cardiovascular events compared with hydrochlorothiazide: a retrospective cohort analysis. Hypertension. 2011;57:689–94.
Mancia G, De Backer G, Dominiczak A, et al. Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105–87.
Messerli FH, Bangalore S, Julius S. Risk/benefit assessment of beta-blockers and diuretics precludes their use for first-line therapy in hypertension. Circulation. 2008;117:2706–15.
Barzilay JI, Davis BR, Cutler JA, et al. Fasting glucose levels and incident diabetes mellitus in older nondiabetic adults randomized to receive 3 different classes of antihypertensive treatment: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2006;166:2191–201.
Verdecchia P, Reboldi G, Angeli F, et al. Adverse prognostic significance of new diabetes in treated hypertensive subjects. Hypertension. 2004;43:963–9.
• Parving HH, Brenner BM, McMurray JJ, et al. Aliskiren Trial in Type 2 Diabetes Using Cardio-Renal Endpoints (ALTITUDE): rationale and study design. Nephrol Dial Transplant. 2009;24:1663–71. The ALTITUDE trial is an outcomes trial in diabetics with chronic kidney disease already on an ACEI or ARB; patients were randomized to receive aliskiren or placebo. The trial was halted early (see below) due to an increase in renal impairment, stroke, hypotension, and hyperkalemia.
Novartis. Novartis announces termination of ALTITUDE study with Rasilez/Tekturna in high-risk patients with diabetes and renal impairment [press release]. Available at: http://www.novartis.com/newsroom/media-releases/en/2011/1572562.shtml. Accessed April 2012.
Mann JF, Schmieder RE, McQueen M, et al. ONTARGET investigators. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008;372:547–53.
Yusuf S, Teo KK, Pogue J, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547–59.
Retraction--Combination treatment of angiotensin-II receptor blocker and angiotensin-converting-enzyme inhibitor in non-diabetic renal disease (COOPERATE): a randomised controlled trial. Lancet. 2009;374:1226.
Mancia G, Laurent S, Agabiti-Rosei E, et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J Hypertens. 2009;27:2121–58.
• Gupta AK, Arshad S, Poulter NR. Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension. 2010;55:399–407. This meta-analysis analyzed trials comparing fixed-dose combinations of antihypertensive drugs with their free-drug components. There was 21 % better medication compliance, as well as non-significant trends toward fewer adverse events and better BP control, with FDCs compared to free drug components.
Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120:713–9.
• Sherrill B, Halpern M, Khan S, et al. Single-pill vs free-equivalent combination therapies for hypertension: a meta-analysis of health care costs and adherence. J Clin Hypertens (Greenwich). 2011;13:898–909. This meta-analysis included trials comparing fixed-dose combinations of antihypertensive drugs with their free-drug components. The analysis demonstrated lower all-cause total costs, lower hypertension- and cardiovascular-related costs, and lower medication costs with FDCs compared to free drug components.
Khan NA, Hemmelgarn B, Padwal R, et al. The 2007 Canadian Hypertension Education Program recommendations for the management of hypertension: part 2 - therapy. Can J Cardiol. 2007;23:539–50.
Taylor AA. Combination drug treatment of hypertension: have we come full circle? Curr Cardiol Rep. 2004;6:421–6.
PDR.net: Physician’s Desk Reference. Copyright 2012, PDR Network, LLC. Available at: http://www.pdr.net/Default.aspx. Accessed April 2012.
Disclosure
Dr. Cowart: none. Dr. Taylor serves as a board member for American Society of Hypertension and has received research funding from Novartis Pharmaceuticals, Forest Research Laboratories, National Institutes of Health (NIH), National Heart, Lung, and Blood Institute (NHLBI), National Institute of Neurological Disorders and Stroke (NINDS), and VPDiagnostics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cowart, J.B., Taylor, A.A. Should Two-Drug Initial Therapy for Hypertension Be Recommended for All Patients?. Curr Hypertens Rep 14, 324–332 (2012). https://doi.org/10.1007/s11906-012-0280-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-012-0280-9
Keywords
- Hypertension
- Combination antihypertensive therapy
- Monotherapy
- Fixed-dose combination
- Calcium channel blocker
- CCB
- Angiotensin converting enzyme inhibitor
- ACE inhibitor
- ACEI
- Angiotensin receptor blocker
- ARB
- Diuretic
- Thiazide
- Chlorthalidone
- β-blocker
- Beta blocker
- Cardiovascular outcome
- Therapeutic inertia
- Medication persistence
- Clinical inertia