Abstract
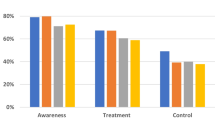
Despite clinical trial evidence and public health data documenting the benefits of controlling hypertension in individuals and populations, implementation in practice is less than optimal. Barriers to hypertension care and control are remarkably persistent and continue to impede improvement in rates of awareness, treatment, and control. Barriers have been identified at the patient, provider, health care organization, and community levels. At every level, knowledge, attitudes, values, and beliefs can impede the evidence-based recommended behaviors needed to lower blood pressure and sustain lowering over time. Numerous new studies provide data that reinforce the need for culturally sensitive interventions at each level.
Similar content being viewed by others
References and Recommended Reading
Green LW, Kreuter MW: Health Promotion and Planning: An Educational and Environmental Approach. Mountain View, CA: Mayfield Publishing Company; 1991.
Miller NH, Hill M, Kottke T, Ockene IS: Multilevel compliance challenge American Heart Association Expert Panel: the multilevel compliance challenge: recommendations for a call to action. AHA Scientific Statement; 1997. This American Heart Association scientific statement presents a new paradigm in which compliance is a behaviorally based challenge at the provider and organization level, as well as at the patient level. Evidence-based strategies and actions to be taken at each level are presented.
Rubin HR: Overcoming barriers to preventive care. J Gen Intern Med 2000, 15:434–436.
Kotchen JM, Walker WE, Chelius TH, et al.: Hypertension control and access to medical care in the inner city. Am J Public Health 1998, 88:1696–1699.
Shakoor-Abdullah B, Kotchen JM, Walker WE, et al.: Incorporating socio-economic and risk factor diversity into the development of an African-American community blood pressure control program. Ethnicity Dis 1997, 7:175–183.
DiMatteo MR, Lepper HS, Coghan TW: Depression is a risk factor for noncompliance with medical treatment. Arch Intern Med 2000, 160:2101–2107.
Hill MN, Bone LR, Kim MT, et al.: Barriers to hypertension care and control in young black men. Am J Hypertens 1999, 12:951–958. This study documents the health status and life experiences of this little studied group. The distribution and determinants of participation in treatment, adherence to therapy, and blood pressure control are described.
Elliott WJ, Maddy R, Toto R, Bakris G: Hypertension in patients with diabetes. Postgrad Med 2000, 107:29–38.
Hyman DJ, Pavlik VN, Valbona C: Physician role in lack of awareness and control of hypertension [abstract]. AHA Conference on Cardiovascular Disease, Epidemiology and Prevention. La Jolla, CA; 2000.
Berlowitz DR, Ash AS, Hickey EC: Inadequate management of blood pressure in a hypertensive population. N Engl J Med 1998, 339:1957–1963. This study provided potent evidence of the lack of medical management of hypertension by physicians in a population of veterans.
Stafford JL, Moss BL, Petkun WM: Physicians‘ satisfaction with hypertension (HTN) management and their role in improving patient compliance. AmJ Hypertens 1998, 11:233A. A survey of physicians‘ experience in hypertension management compares their satisfaction with their medication versus lifestyle interventions. Physicians were less satisfied with lifestyle modification than medication treatment and saw their role primarily as an educator only, rather as a facilitator of compliance and lifestyle change.
Waeber B, Vetter W, Darioli R, et al.: Improved blood pressure control by monitoring compliance with antihypertensive therapy. Int J Clin Pract 1999, 53:37–38.
Coleman MT, Lott JA, Sharma S: Use of continuous quality improvement to identify barriers in the management of hypertension. Am J Med Qual, 2000, 15:72–77. This article demonstrates the use of continuous quality improvement as a tool for identifying barriers to hypertension control. The principle barriers identified were cost of care and changes in lifestyle, of which African Americans suffer disproportionately.
Cranney M, Barton S, Walley T: Addressing barriers to change: an RCT of practice-based education to improve the management of hypertension in the elderly. Br J Gen Pract 1999, 49:522–526.
Stockwell DH, Madhavan S, Cohen H, et al.: The determinants of hypertension awareness, treatment, and control in an insured population. Am J Public Health 1998, 84:1768–1774. Of 409 hypertensive New York City health care workers (a population with comprehensive medical coverage), 71% were aware of their condition yet only 49% had been treated and only 12% were currently under control. This study shows that even absent traditional barriers such as health insurance, poor adherence remains.
Hill MN, Bone LR, Sterling SC, et al.: A clinical trial to improve high blood pressure care in young black men. Am J Hypertens 1999, 12:549–554.
Krieger J, Collier C, Song L, Martin D: Linking communitybased blood pressure measurement to clinical care: a randomized controlled trial of outreach and tracking by community health workers. Am J Public Health 1999, 89:856–861.
Bone LR, Hill MN, Stallings R, et al.: Community health survey in an urban African American neighborhood: Distribution and correlates of elevated blood pressure. Ethnicity Dis 2000, 10:87–95.
Ward HJ, Morisky DE, Lees NB, Fong R: A clinic and community-based approach to hypertension control in an underserved minority population: design and methods. Am J Hypertens, 2000, 13:177–183.
Brownely KA, Hurwitz BE, Schneiderman N: Ethnic variations in the pharmacological and nonpharmacological treatment of hypertension: biopsychosocial perspective. Hum Biol 1999, 71:607–639. This article emphasizes the social, political, and biologic differences within societies and how they contribute to awareness of the multifactorial nature of hypertension by the physician and the patient.
Hill MN, Miller NH: Compliance enhancement: a call for multidisciplinary team approaches. Circulation 1996, 93:4–6.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hill, M.N., Sutton, B.S. Barriers to hypertension care and control. Current Science Inc 2, 445–450 (2000). https://doi.org/10.1007/s11906-000-0026-y
Issue Date:
DOI: https://doi.org/10.1007/s11906-000-0026-y