Abstract
With HIV funding plateauing and the number of people living with HIV increasing due to the rollout of life-saving antiretroviral therapy, policy makers are faced with increasingly tighter budgets to manage the ongoing HIV epidemic. Cost-effectiveness and modeling analyses can help determine which HIV interventions may be of best value. Incidence remains remarkably high in certain populations and countries, making prevention key to controlling the spread of HIV. This paper briefly reviews concepts in modeling and cost-effectiveness methodology and then examines results of recently published cost-effectiveness analyses on the following HIV prevention strategies: condoms and circumcision, behavioral- or community-based interventions, prevention of mother-to-child transmission, HIV testing, pre-exposure prophylaxis, and treatment as prevention. We find that the majority of published studies demonstrate cost-effectiveness; however, not all interventions are affordable. We urge continued research on combination strategies and methodologies that take into account willingness to pay and budgetary impact.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
UNAIDS and Kaiser Family Foundation. Financing the response to HIV in low- and middle-income countries: international assistance from donor governments in 2014. July 2015.
Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA. 1996;276(15):1253–8.
Chambers JD, Cangelosi MJ, Neumann PJ. Medicare’s use of cost-effectiveness analysis for prevention (but not for treatment). Health Policy. 2015;119(2):156–63.
Commission on Macroeconomics and Health. Macroeconomics and health: investing in health for economic development. World Health Organization. 2001.
World Bank. World development indicators. 2015. http://data.worldbank.org/data-catalog/world-development-indicators. Accessed 26 January 2016.
National Treasury of the Republic of South Africa. Estimates of national expenditure (Abridged version). 2015.
Revill P, Walker S, Madan J, Ciaranello A, Mwase T, Gibb D, et al. Using cost-effectiveness thresholds to determine value for money in low- and middle-income country healthcare systems: are current international norms fit for purpose? [CHE Research Paper 98]. The University of York: Center for Health Economics. 2014.
Uthman OA, Popoola TA, Uthman MM, Aremu O. Economic evaluations of adult male circumcision for prevention of heterosexual acquisition of HIV in men in sub-Saharan Africa: a systematic review. PLoS One. 2010;5(3), e9628.
Menon V, Gold E, Godbole R, Castor D, Mahler H, Forsythe S, et al. Costs and impacts of scaling up voluntary medical male circumcision in Tanzania. PLoS One. 2014;9(5), e83925.
Pham QD, Wilson DP, Kerr CC, Shattock AJ, Do HM, Duong AT, et al. Estimating the cost-effectiveness of HIV prevention programmes in Vietnam, 2006–2010: a modelling study. PLoS One. 2015;10(7), e0133171.
Mitchell KM, Lepine A, Terris-Prestholt F, Torpey K, Khamofu H, Folayan MO, et al. Modelling the impact and cost-effectiveness of combination prevention amongst HIV serodiscordant couples in Nigeria. AIDS. 2015;29(15):2035–44. This study examined TasP, short- vs. long-term PrEP, condom promotion, and several combinations of these strategies using a deterministic cohort model. The results indicate the order in which prevention interventions should be prioritized as more resources become available.
Mvundura M, Nundy N, Kilbourne-Brook M, Coffey PS. Estimating the hypothetical dual health impact and cost-effectiveness of the woman’s condom in selected sub-Saharan African countries. Int J Womens Health. 2015;7:271–7.
United Nations Population Fund, Global Forum on MSM & HIV, United Nations Development Programme, World Health Organization, United States Agency for International Development, World Bank. Implementing comprehensive HIV and STI programmes with men who have sex with men: practical guidance for collaborative interventions. 2015.
Ruger JP, Abdallah AB, Ng NY, Luekens C, Cottler L. Cost-effectiveness of interventions to prevent HIV and STDs among women: a randomized controlled trial. AIDS Behav. 2014;18(10):1913–23.
Song DL, Altice FL, Copenhaver MM, Long EF. Cost-effectiveness analysis of brief and expanded evidence-based risk reduction interventions for HIV-infected people who inject drugs in the United States. PLoS One. 2015;10(2), e0116694.
Vassall A, Pickles M, Chandrashekar S, Boily MC, Shetty G, Guinness L, et al. Cost-effectiveness of HIV prevention for high-risk groups at scale: an economic evaluation of the Avahan programme in South India. Lancet Glob Health. 2014;2(9):e531–40. Using a dynamic transmission model, Vassall et al. estimate the number of HIV infections, DALYs averted, and incremental cost-effectiveness of a prevention program implemented at scale across 22 different districts in India. This study is a good example of how intervention costs and effectiveness can vary substantially within a single country, with program costs/DALY averted ranging from $17–$472 between districts.
Vassall A, Chandrashekar S, Pickles M, Beattie TS, Shetty G, Bhattacharjee P, et al. Community mobilisation and empowerment interventions as part of HIV prevention for female sex workers in Southern India: a cost-effectiveness analysis. PLoS One. 2014;9(10), e110562.
World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. June 2013.
VanDeusen A, Paintsil E, Agyarko-Poku T, Long EF. Cost effectiveness of option B plus for prevention of mother-to-child transmission of HIV in resource-limited countries: evidence from Kumasi, Ghana. BMC Infect Dis. 2015;15:130.
Gopalappa C, Stover J, Shaffer N, Mahy M. The costs and benefits of Option B+ for the prevention of mother-to-child transmission of HIV. AIDS. 2014;28 Suppl 1:S5–14.
Ishikawa N, Shimbo T, Miyano S, Sikazwe I, Mwango A, Ghidinelli MN, et al. Health outcomes and cost impact of the new WHO 2013 guidelines on prevention of mother-to-child transmission of HIV in Zambia. PLoS One. 2014;9(3), e90991.
Yu W, Li C, Fu X, Cui Z, Liu X, Fan L, et al. The cost-effectiveness of different feeding patterns combined with prompt treatments for preventing mother-to-child HIV transmission in South Africa: estimates from simulation modeling. PLoS One. 2014;9(7), e102872.
Long EF, Mandalia R, Mandalia S, Alistar SS, Beck EJ, Brandeau ML. Expanded HIV testing in low-prevalence, high-income countries: a cost-effectiveness analysis for the United Kingdom. PLoS One. 2014;9(4), e95735.
Hutchinson AB, Farnham PG, Sansom SL, Yaylali E, Mermin JH. Cost-effectiveness of frequent HIV testing of high risk populations in the United States. J Acquir Immune Defic Syndr. 2015.
Cambiano V, Ford D, Mabugu T, Napierala Mavedzenge S, Miners A, Mugurungi O, et al. Assessment of the potential impact and cost-effectiveness of self-testing for HIV in low-income countries. J Infect Dis. 2015;212(4):570–7. Using a stochastic, individual-based model, a scenario of no self-testing is compared to a scenario with self-testing. Although self-testing has only a modest impact on health or savings, the authors posit that the money saved through self-testing could be further invested in other highly cost-effective intervention. This optimistic point of view is one policy makers can keep in mind when considering healthcare savings.
Smith JA, Sharma M, Levin C, Baeten JM, van Rooyen H, Celum C, et al. Cost-effectiveness of community-based strategies to strengthen the continuum of HIV care in rural South Africa: a health economic modelling analysis. Lancet HIV. 2015;2(4):e159–68.
Bassett IV, Govindasamy D, Erlwanger AS, Hyle EP, Kranzer K, van Schaik N, et al. Mobile HIV screening in Cape Town, South Africa: clinical impact, cost and cost-effectiveness. PLoS One. 2014;9(1), e85197.
Owusu-Edusei Jr K, Tao G, Gift TL, Wang A, Wang L, Tun Y, et al. Cost-effectiveness of integrated routine offering of prenatal HIV and syphilis screening in China. Sex Transm Dis. 2014;41(2):103–10.
Rutstein SE, Brown LB, Biddle AK, Wheeler SB, Kamanga G, Mmodzi P, et al. Cost-effectiveness of provider-based HIV partner notification in urban Malawi. Health Policy Plan. 2014;29(1):115–26.
Birnkrant D. Truvada® (emtricitabine/tenofovir disoproxil fumarate) for pre-exposure prophylaxis (PrEP) for HIV-1 prevention in populations at high risk of sexually acquired HIV Infection NDA 21752 S-30. Antiviral Products Advisory Committee, U.S. Food and Drug Administration. 2012.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90.
Karim QA, Karim SS, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329(5996):1168–74.
Marrazzo JM, Ramjee G, Richardson BA, Gomez K, Mgodi N, Nair G, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2015;372(6):509–18.
Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34.
Van Damme L, Corneli A, Ahmed K, Agot K, Lombaard J, Kapiga S, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367(5):411–22.
Paltiel AD, Freedberg KA, Scott CA, Schackman BR, Losina E, Wang B, et al. HIV preexposure prophylaxis in the United States: impact on lifetime infection risk, clinical outcomes, and cost-effectiveness. Clin Infect Dis. 2009;48(6):806–15.
Gomez GB, Borquez A, Case KK, Wheelock A, Vassall A, Hankins C. The cost and impact of scaling up pre-exposure prophylaxis for HIV prevention: a systematic review of cost-effectiveness modelling studies. PLoS Med. 2013;10(3), e1001401.
Schackman BR, Eggman AA. Cost-effectiveness of pre-exposure prophylaxis for HIV: a review. Curr Opin HIV AIDS. 2012;7(6):587–92.
Juusola JL, Brandeau ML, Owens DK, Bendavid E. The cost-effectiveness of preexposure prophylaxis for HIV prevention in the United States in men who have sex with men. Ann Intern Med. 2012;156(8):541–50.
Kessler J, Myers JE, Nucifora KA, Mensah N, Toohey C, Khademi A, et al. Evaluating the impact of prioritization of antiretroviral pre-exposure prophylaxis in New York City. AIDS. 2014.
Chen A, Dowdy DW. Clinical effectiveness and cost-effectiveness of HIV pre-exposure prophylaxis in men who have sex with men: risk calculators for real-world decision-making. PLoS One. 2014;9(10), e108742.
Schneider K, Gray RT, Wilson DP. A cost-effectiveness analysis of HIV preexposure prophylaxis for men who have sex with men in Australia. Clin Infect Dis. 2014;58(7):1027–34.
Alistar SS, Owens DK, Brandeau ML. Effectiveness and cost effectiveness of oral pre-exposure prophylaxis in a portfolio of prevention programs for injection drug users in mixed HIV epidemics. PLoS One. 2014;9(1), e86584.
Mabileau G, Schwarzinger M, Flores J, Patrat C, Luton D, Epelboin S, et al. HIV-serodiscordant couples desiring a child: ‘treatment as prevention,’ preexposure prophylaxis, or medically assisted procreation? Am J Obstet Gynecol. 2015;213(3):341.e1–e12.
Terris-Prestholt F, Foss AM, Cox AP, Heise L, Meyer-Rath G, Delany-Moretlwe S, et al. Cost-effectiveness of tenofovir gel in urban South Africa: model projections of HIV impact and threshold product prices. BMC Infect Dis. 2014;14:14. This study determines the cost and cost-effectiveness of gel-based HIV prophylaxis used on a per-sex act basis, a substantially less expensive option than daily oral PrEP. The authors perform analyses to determine the various cost, coverage, and effectiveness thresholds that would be required for the gel to be considered as cost-effective as condoms. This unique analysis is useful for comparison of prevention interventions.
Alistar SS, Grant PM, Bendavid E. Comparative effectiveness and cost-effectiveness of antiretroviral therapy and pre-exposure prophylaxis for HIV prevention in South Africa. BMC Med. 2014;12:46.
Ying R, Sharma M, Heffron R, Celum CL, Baeten JM, Katabira E, et al. Cost-effectiveness of pre-exposure prophylaxis targeted to high-risk serodiscordant couples as a bridge to sustained ART use in Kampala, Uganda. J Int AIDS Soc. 2015;18(4 Suppl 3):20013.
Jewell BL, Cremin I, Pickles M, Celum C, Baeten JM, Delany-Moretlwe S, et al. Estimating the cost-effectiveness of pre-exposure prophylaxis to reduce HIV-1 and HSV-2 incidence in HIV-serodiscordant couples in South Africa. PLoS One. 2015;10(1), e0115511.
Cremin I, Morales F, Jewell BL, O’Reilly KR, Hallett TB. Seasonal PrEP for partners of migrant miners in southern Mozambique: a highly focused PrEP intervention. J Int AIDS Soc. 2015;18(4 Suppl 3):19946. doi:10.7448/ias.18.4.19946.
Walensky RP, Park JE, Wood R, Freedberg KA, Scott CA, Bekker LG, et al. The cost-effectiveness of pre-exposure prophylaxis for HIV infection in South African women. Clin Infect Dis. 2012;54(10):1504–13.
Nichols BE, Baltussen R, van Dijk JH, Thuma PE, Nouwen JL, Boucher CA, et al. Cost-effectiveness of PrEP in HIV/AIDS control in Zambia: a stochastic league approach. J Acquir Immune Defic Syndr. 2014;66(2):221–8. The authors utilize stochastic league tables, an approach that calculates the probability of selecting an intervention based on different budget levels. This method is exceptionally important for policy makers who must consider budgeting and what interventions to fund.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Danel C, Moh R, Gabillard D, Badje A, Le Carrou J, Ouassa T, et al. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med. 2015;373(9):808–22.
Lundgren JD, Babiker AG, Gordin F, Emery S, Grund B, Sharma S, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373(9):795–807.
Walensky RP, Ross EL, Kumarasamy N, Wood R, Noubary F, Paltiel AD, et al. Cost-effectiveness of HIV treatment as prevention in serodiscordant couples. N Engl J Med. 2013;369(18):1715–25. Based on the results of HPTN052, this study was the first to report that TasP is a cost-effective prevention strategy for serodiscordant couples, with results supporting this conclusion both in a South African and Indian context. Several studies have since gone on to evaluate the cost-effectiveness of TasP in various countries and populations.
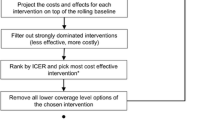
Kerr CC, Stuart RM, Gray RT, Shattock AJ, Fraser-Hurt N, Benedikt C, et al. Optima: a model for HIV epidemic analysis, program prioritization, and resource optimization. J Acquir Immune Defic Syndr. 2015;69(3):365–76.
World Health Organization. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. September 2015. Accessed 19 Nov 2015: http://www.who.int/hiv/pub/guidelines/earlyrelease-arv/en/.
Walensky RP, Weinstein MC, Smith HE, Freedberg KA, Paltiel AD. Optimal allocation of testing dollars: the example of HIV counseling, testing, and referral. Med Decis Making. 2005;25(3):321–9.
Acknowledgments
The authors would like to thank Amy Zheng for her technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Margo M. Jacobsen declares that she has no conflict of interest.
Rochelle P. Walensky reports grants from the National Institutes of Health and personal fees from LeClair Ryan.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on The Science of Prevention
Rights and permissions
About this article
Cite this article
Jacobsen, M.M., Walensky, R.P. Modeling and Cost-Effectiveness in HIV Prevention. Curr HIV/AIDS Rep 13, 64–75 (2016). https://doi.org/10.1007/s11904-016-0303-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-016-0303-2