Abstract
Purpose of Review
Chronic diarrhea is a common problem in all age groups but is a particularly challenging diagnostic problem in the elderly, since many different conditions need to be considered. The purpose of this review is to discuss the evaluation of chronic diarrhea in older individuals. It highlights those conditions that seem to occur with increased frequency in the elderly, discusses the diagnostic tests that are of greatest value in sorting out these problems, and presents an approach to evaluation that is both practical and affordable.
Recent Findings
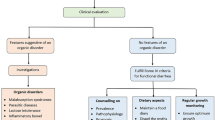
There appears to be little value in distinguishing irritable bowel syndrome with diarrhea (IBS-D) from functional diarrhea in most patients, including older individuals. Both conditions need a thoughtful analysis of potential causes that may lead to more focused treatment. Older individuals may be more at risk of having certain structural disorders, and these need to be considered when constructing a differential diagnosis. In addition, elderly patients may have atypical presentations of specific disorders that require an increased index of suspicion. Diagnostic tests generally seem to perform well in older patients but have not been validated in this cohort of patients. Although the pretest probabilities of certain diseases are different in the elderly, the conventional algorithm for assessment of chronic diarrhea should lead to a diagnosis in most cases.
Summary
Better studies are needed to adequately quantitate the likelihood of different diagnoses and the operating characteristics of diagnostic tests in older patients with chronic diarrhea. Lacking that information, physicians can still do a good job of making a diagnosis in these patients by adopting a stepwise approach.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Singh P, Mitsuhashi S, Ballou S, Rangan V, Sommers T, Cheng V, et al. Demographic and dietary associations of chronic diarrhea in a representative sample of adults in the United States. Am J Gastroenterol. 2018;113(4):593–600.
• Schiller LR, Pardi DS, Sellin JH. Chronic diarrhea: diagnosis and management. Clin Gastroenterol Hepatol. 2017;15(2):182–93. A series of issues that frame the evaluation and management of chronic diarrhea.
•• Schiller LR. Evaluation of chronic diarrhea and irritable bowel syndrome with diarrhea in adults in the era of precision medicine. Am J Gastroenterol. 2018;113(5):660–9. Basic approach to evaluation of chronic diarrhea in adults.
Steffer KJ, Santa Ana CA, Cole JA, Fordtran JS. The practical value of comprehensive stool analysis in detecting the cause of idiopathic chronic diarrhea. Gastroenterol Clin N Am. 2012;41(3):539–60.
Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Grant Thompson W, et al. U. S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38(9):1569–80.
Almario CV, Ballal ML, Chey WD, Nordstrom C, Khanna D, Spiegel BMR. Burden of gastrointestinal symptoms in the United States: results of a nationally representative survey of over 71,000 Americans. Am J Gastroenterol. 2018;113(11):1701–10.
Talley NJ, O’Keefe EA, Zinsmeister AR, Melton LJ 3rd. Prevalence of gastrointestinal symptoms in the elderly: a population-based study. Gastroenterology. 1992;102(3):895–901.
Sommers T, Mitsuhashi S, Singh P, Hirsch W, Katon J, Ballou S, et al. Prevalence of chronic constipation and chronic diarrhea in diabetic individuals in the United States. Am J Gastroenterol. 2019;114(1):135–42.
Bayless TM, Brown E, Paige DM. Lactase non-persistence and lactose intolerance. Curr Gastroenterol Rep. 2017;19(5):23. https://doi.org/10.1007/s11894-017-0558-9.
Storhaug CL, Fosse SK, Fadnes LT. Country, regional, and global estimates for lactose malabsorption in adults: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2017;2(10):738–46.
Buchman AL. Intestinal failure and rehabilitation. Gastroenterol Clin N Am. 2018;47(2):327–40.
Philip NA, Ahmed N, Pitchumoni CS. Spectrum of drug-induced chronic diarrhea. J Clin Gastroenterol. 2017;51(2):111–7.
Abraham BP, Sellin JH. Drug-induced, factitious, & idiopathic diarrhoea. Best Pract Res Clin Gastroenterol. 2012;26(5):633–48.
• Pardi DS. Diagnosis and management of microscopic colitis. Am J Gastroenterol. 2017;112(1):78–85. Review of a common cause of chronic diarrhea in older patients.
Gentile N, Yen EF. Prevalence, pathogenesis, diagnosis, and management of microscopic colitis. Gut Liver. 2018;12(3):227–35.
Bergman D, Clements MS, Khalili H, Agréus L, Hultcrantz R, Ludvigsson JF. A nationwide cohort study of the incidence of microscopic colitis in Sweden. Aliment Pharmacol Ther. 2019;49(11):1395–400.
Gentile NM, Khanna S, Loftus EV Jr, et al. The epidemiology of microscopic colitis in Olmsted County from 2002–2010: a population-based study. Clin Gastroenterol Hepatol. 2014;12(5):838–42.
Holt PR. Intestinal malabsorption in the elderly. Dig Dis. 2007;25:144–50.
Schiller LR. Diarrhea and malabsorption in the elderly. Gastroenterol Clin N Am. 2009;38(3):481–502.
Marth T. Tropheryma whipplei, immunosuppression and Whipple’s disease: from a low-pathogenic, environmental infectious organism to a rare, multifaceted inflammatory complex. Dig Dis. 2015;33(2):190–9.
Ahmed Z, Imdad A, Connelly JA, Acra S. Autoimmune enteropathy: an updated review with special focus on stem cell transplant therapy. Dig Dis Sci. 2018;64:643–54. https://doi.org/10.1007/s10620-018-5364-1.
Ebrahim VS, Martin J, Murthy S, Odstrcil E, Huang H, Polter D. Olmesartan-associated enteropathy. Proc (Baylor Univ Med Cent). 2017;30(3):348–50.
Collin P, Vilppula A, Luostarinen L, Holmes GKT, Kaukinen K. Review article: coeliac disease in later life must not be missed. Aliment Pharmacol Ther. 2018;47(5):563–72.
Sherid M, Samo S, Sulaiman S, et al. Comparison of ischemic colitis in the young and the elderly. WMJ. 2016;115(4):196–202.
Löhr JM, Panic N, Vujasinovic M, Verbeke CS. The ageing pancreas: a systematic review of the evidence and analysis of the consequences. J Intern Med. 2018;283(5):446–60.
Hirth M, Härtel N, Weiss C, Hardt P, Gubergrits N, Ebert MP, et al. Clinical course of chronic pancreatitis in elderly patients. Digestion. 2019;10:1–8. https://doi.org/10.1159/000494349.
Quigley EMM. The spectrum of small intestinal bacterial overgrowth (SIBO). Curr Gastroenterol Rep. 2019;21(1):3. https://doi.org/10.1007/s11894-019-0671-z.69.
• Rezaie A, Pimentel M, Rao SS. How to test and treat small intestinal bacterial overgrowth: an evidence-based approach. Curr Gastroenterol Rep. 2016;18(2):8. https://doi.org/10.1007/s11894-015-0482-9. Review of the evaluation and management of SIBO in adults.
Mitsui T, Shimaoka K, Goto Y, Kagami H, Kinomoto H, Ito A, et al. Small bowel bacterial overgrowth is not seen in healthy adults but is in disabled older adults. Hepatogastroenterology. 2006;53(67):82–5.
van Walree IC, van Tuyl SA, Hamaker ME. Late-onset inflammatory bowel disease in the very elderly. Neth J Med. 2015;73(1):4–9.
Butter M, Weiler S, Biedermann L, Scharl M, Rogler G, Bischoff-Ferrari HA, et al. Clinical manifestations, pathophysiology, treatment and outcome of inflammatory bowel diseases in older people. Maturitas. 2018;110:71–8.
John ES, Katz K, Saxena M, Chokhavatia S, Katz S. Management of inflammatory bowel disease in the elderly. Curr Treat Options Gastroenterol. 2016;14(3):285–304.
White AE, Clampa N, Chen Y, et al. Characteristics of Campylobacter, Salmonella infections and acute gastroenteritis in older adults in Australia, Canada, and the United States. Clin Infect Dis. 2019. https://doi.org/10.1093/cid/ciy1142.
Jump RLP, Crnich CJ, Mody L, Bradley SF, Nicolle LE, Yoshikawa TT. Infectious diseases in older adults of long-term care facilities: update on approach to diagnosis and management. J Am Geriatr Soc. 2018;66(4):789–803.
Asempa TE, Nicolau DP. Clostridium difficile infection in the elderly: an update on management. Clin Interv Aging. 2017;12:1799–809.
Donskey CJ. Clostridium difficile in older adults. Infect Dis Clin N Am. 2017;31(4):743–56.
•• McDonald LC, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66(7):987–94. https://doi.org/10.1093/cid/ciy149. Current consensus viewpoint on the management of C. difficile.
Ooijevaar RE, van Beurden YH, Terveer EM, Goorhuis A, Bauer MP, Keller JJ, et al. Update of treatment algorithms for Clostridium difficile infection. Clin Microbiol Infect. 2018;24(5):452–62.
•• Lacy BE, Mearin F, Chang L, Chey WD, Lembo AJ, Simren M, et al. Bowel disorders. Gastroenterology. 2016;150:1393–407. Rome IV definitions of functional bowel disorders, including IBS-D.
Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014;6:71–80.
Yu SW, Rao SS. Anorectal physiology and pathophysiology in the elderly. Clin Geriatr Med. 2014;30(1):95–106.
Serrano Falcón B, Barceló López M, Mateos Muñoz B, Álvarez Sánchez A, Rey E. Fecal impaction: a systematic review of its medical complications. BMC Geriatr. 2016;16:4. https://doi.org/10.1186/s12877-015-0162-5.
Borbély YM, Osterwalder A, Kröll D, et al. Diarrhea after bariatric procedures: diagnosis and therapy. World J Gastroenterol. 2017;23(26):4689–700.
Schiller LR. Antidiarrheal drug therapy. Curr Gastroenterol Rep. 2017;19(5):18. https://doi.org/10.1007/s11894-017-0557-x.
Camilleri M. Bile acid diarrhea: prevalence, pathogenesis, and therapy. Gut Liver. 2015;9(3):332–9.
Teo MTW, Sebag-Montefiore D, Donnellan CF. Prevention and management of radiation-induced late gastrointestinal toxicity. Clin Oncol. 2015;27:656–67.
Zboromyrska Y, Vila J. Advanced PCR-based molecular diagnosis of gastrointestinal infections: challenges and opportunities. Expert Rev Mol Diagn. 2016;16(6):631–40.
• Schumann D, Klose P, Lauche R, Dobos G, Langhorst J, Cramer H. Low fermentable, oligo-, di-, mono-saccharides and polyol diet in the treatment of irritable bowel syndrome: a systematic review and meta-analysis. Nutrition. 2018;45:24–31. Systematic review of the impact of the low FODMAPs diet in IBS.
• Vijayvargiya P, Camilleri M. Update on bile acid malabsorption: finally ready for prime time? Curr Gastroenterol Rep. 2018;20(3):10. https://doi.org/10.1007/s11894-018-0615-z. This review focuses on bile acid malabsorption as a common mechanism of chronic diarrhea.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Lawrence Schiller reports personal fees from Allergan, Ardelyx, Ironwood, Salix/Bausch, Shire, Commonwealth Laboratories, Prometheus Laboratories, Abbvie and Romark, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Gastroenterology in Geriatric Patients
Rights and permissions
About this article
Cite this article
Schiller, L.R. Chronic Diarrhea Evaluation in the Elderly: IBS or Something Else?. Curr Gastroenterol Rep 21, 45 (2019). https://doi.org/10.1007/s11894-019-0714-5
Published:
DOI: https://doi.org/10.1007/s11894-019-0714-5