Abstract
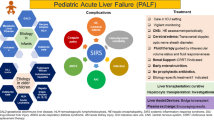
Although the etiologies of pediatric acute liver failure (ALF) are diverse, ultimate pathophysiologic pathways and management challenges for these disorders, usually lethal in the pre-transplant era, are similar. This review considers particularly the mechanisms of, and monitoring for, intracranial hypertension and coagulopathy; summarizes detailed advice for management of the ALF-associated failures of multiple body systems; and reviews the variety of prognostic scores available to guide management and assist in choosing the patients most apt to benefit from liver transplantation and the optimal timing for such transplantation.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Lee WS, McKierman P, Keely DA. Etiology, outcome, and prognostic indication of Childhood fulminant hepatic failure in United Kingdom. Pediatr Gastroenterol Nutr 2005, 575–581
• Farmer DG, Venick RS, McDiarmid SV et al. Fulminant Hepatic Failure in children: Superior and durable outcome with liver transplantation over 25 years at a single center. Ann Surg 2009; 250(3) 484–493. This study, representing one of the largest published series on LT for ALF in a single center, demonstrates a long-term survival of nearly 70 %, focuses attention on morbility and prognosis, and develops a clinically applicable and readily measurable set of pretransplant factors that determine posttransplant outcome.
Munne MS, Altabert NR, Vladimisky SN, et al. Identifications of polyhyletic variants in acute hepatitis suggest an under diagnosed circulation of hepatitis E virus in Argentina. JClin Virol. 2011;52(2):138–41.
Sundaram SS, Alonso EM, Narkewicz MR, Zhang S, Squires RH. Pediatric Acute Liver Failure Study Group. Characterization and outcomes of young infants with acute liver failure. J Pediatr. 2011;159(5):813–8.
Ciocca M, Ramonet M, Cuarterolo M, Lopez S, Cernadas C, Alvarez F. Prognosis Factors in pediatric acute liver failure. Arch Dis Child. 2008;03:48–51.
Bernal W, Auzinger G, Dhawan A, Wendon J. Acute liver failure. Lancet. 2010;376(9736):190–201.
Larsen FS, Wendon J. Prevention and management of brain edema in patients with Acute Liver Failure. Liver Transpl. 2008;14:90–6.
Clemmensen JO, Larsen FS, Kondrup J, Hansen BA, Ott P. Cerebral herniation in patients with acute liver failure is correlated with arterial ammonia concentration. Hepatology. 1999;29:648–53.
Jiang W, Desjardins P, Butterworth RF. Cerebral inflammation contributes to encephalopathy and brain edema in acute liver failure: protective effect of minocycline. J Neurochem. 2009;109:485–93.
Fiore M, Probert L, Kollia G, Akassoglou K, et al. Neurobehavioral alterations in developing transgenic mice espressing TNF-alpha in the brain. Brain Behav Immun. 1996;10:126–38.
Krueger J, Fang J, Taishi P, Chen Z, et al. Sleep A physiologic role for IL-1 beta and TNF- alpha. Ann NY Acad Sci. 1998;856:148–59.
AllanS and RothwellN. Cytokines and acute neurodegeneration. Nat. Rev. Neurosci. 2001; 2, 734–744. Petty and Lo E. Functional complexes of the blood- brain barrier: permeability changes in neuroinflammation. Prog. Neurobiol.2002; 68, 311–323.
Andersson A, Ronnback L, Hansson E. Lactate induce tumor necrosis factor- alpha, interleukin-6 and interleukin-1 beta release in microglial and astroglial—enriched primary cultures. J Neurochem. 2005;93:1327–33.
Haussinger D. Low grade cerebral edema and the pathogenesis of hepatic encephalopathy in cirrhosis. Hepatology. 2006;43:1187–90.
Vaquero J, Rose C, Butterworth R. Keeping cool in acute liver failure: Rationale for the use of mild hypothermia. Vaquero J, Rose C, Butterworth R. J Hepatol. 2005;43:1067–77.
Muñoz S, Rajender Reddy K, Lee W. The coagulopathy of acute liver failure and implications for intracranial monitoring. Neurocrit Care. 2008;9:103–7.
Mahajan A, Lat I. Correction of coagulopathy in the setting of acute liver failure. Crit Care Nurs Clin N Am. 2010;22:315–21.
Stravitz R, Kramer A, Darven T, Shaikh O, et al. Intensive care of patients with acute liver failure: recommendations of the U.S. Acute Liver Failure Study Group. Crit Care Med. 2007;35:2498–508.
Bhatia V, Batra Y, Subrat Kumar A. Prophylactic phenytoin does not improve cerebral edema or survival in acute liver failure a controlled clinical trial. J Hepatol. 2004;41:89–96.
• Starvitz R, Larsen F. Therapeutic hypothermia for acute liver failure. Crit Care Med 2009; 37: S258–S264. Cerebral edema is a potentially life-threatening complication of acute liver failure. This article focused on therapeutic hypothermia with a core temperature 32[degrees]- C-35[degrees]C. It showed reduction of cerebral edema and intracranial hypertension in patients with acute liver failure and also showed it to be an effectively bridge to transplantation.
Jacob S, Khan A, Jacobs E, Kandiah P, et al. Prolonged hypothermia as a bridge to recovery for cerebral edema and intracranial hypertension associated with fulminant hepatic failure. Neurocrit Care. 2009;11:242–6.
Dmello D, Cruz-Flores S, Matuschak GM. Moderate hypothermia with intracranial pressure monitoring as a therapeutic paradigm for the management of acute liver failure: A systematic review. Intensive Care Med. 2010;36:210–3.
Cochran JB, Losek JB. Acute Liver Failure in children. Pediatr Emerg Care. 2007;23(2):129–35.
Nadalin S, Heuer M, Wallot M, et al. Paediatric acute liver failure and transplantation: The University of Essen experience. Transpl Int. 2007;20(6):519–27.
Phua J, Lee KH. Liver support devices. Curr Opin Crit Care. 2008;14:208–15.
Sasbon JS, Devictor D, Tissieres P. Liver support for fulminant hepatic failure: Is it time to use the Molecular Adsorbents Recycling System in children? Pediatr Crit Care Medicine. 2005;6(5):585–91.
Arora G, Keeffe EB. Management of chronic liver failure until liver transplantation. Med Clin North Am. 2008;92:839,ix–60,ix.
Tissieres P, Sasbon JS, Devictor D. Liver support for fulminant hepatic failure: is it time to use the Molecular Adsorbents Recycling System in children? Pediatr Crit Care Med. 2005;6:585–91.
Liu JP, Gluud LL, Als-Nielsen B, Gluud C. Artificial and bioartificial support systems for liver failure. Cochrane Database Syst Rev 2004;(1):CD003628
Devictor D, Tissieres P, Afanetti M, Debray D. Acute liver failure in children. Clinics and Research in Hepatology and Gastroenterology. 2011;35:430–7.
• Faraj W, Dar F, Bartlet A, Vilcamelendez H, Marangoni G, Mielivergani G, Dhawan A and Rela M. Auxiliary Liver Transplantation for Acute Liver Failure in Children. Ann Surg. 2010;251(2):351–6. This study presents the largest experience of auxiliary liver transplantation for acute liver failure (ALF) in children over the past 19 years. Auxiliary partial orthotopic LT should be considered in children presenting with ALF who fulfill criteria for LT.
Dhiman R, Jain S, Masheshawri U, et al. Early indicators of prognosis in Fulminant Hepatic Failure: An assessment of the Model for End-Stage Liver Disease (MELD) and King’s College Hospital Criteria. Liver Transpl. 2007;13:814–21.
O’Grady JG. Prognostication in acute liver failure: a tool or an anchor? Liver Transpl. 2007;13:786–7.
O’Grady JG, Graeme JM, Hayllar KM, et al. Early indicators of prognosis infulminant hepatic failure. Gastroenterology. 1989;97:439–45.
Bernuau J, Benhamou JP. Fulminant and subfulminant liver failure. In: McIntyre N, Benhamou JP, Bircher J, Rizzeto M, Rodes J, editors. Oxford Textbook of Clinical. Hepatology. Oxford: Oxford Medical Publications, 1991: 923–942.
Bernuau J, Goudeau A, Poynard T, et al. Multivariate analysis of prognostic factors in fulminant hepatitis B. Hepatology. 1986;6:648–51.
Yantorno S, Kremers W, Ruf A, et al. MELD is superior to King’s College and Clichy’s Criteria to assess prognosis in fulminant hepatic failure. Transplantation. 2007;13:822–8.
• Sanchez M and D’Agostino D. Pediatric end-stage liver disease score in acute liver failure to assess poor prognosis. J Pediatr Gastroenterol Nutr. 2011 Aug 30. This is very important reference shows that PELD score used in a cohort of pediatric patients with ALF provided an accurate specificity and sensitivity to discriminate patients with poor outcome, was superior to that of the KCH and Clichy criteria, and could be helpful in establishing the optimal moment for LT evaluation and inclusion on the emergency waiting list.
Squires Jr RH, Shneider BL, Bucuvalas J, et al. Acute liver failure in children: the first 348 patients in the pediatric acute liver failure study group. J Pediatr. 2006;148:652–8.
Squires RH, Sokol RJ, Schneider BL, et al. Encephalopathy at presentation predicts outcome for children with acute liver failure. Abstract Hepatology. 2002;36:167A.
Tissieres P, Prontera W, Chevret L, et al. The pediatric risk of mortality score in infants and children with fulminant liver failure. Pediatr Transplant. 2003;7:64–8.
Dhawan A, Cheeseman P, Mieli-Vergani G. Approaches to liver failure in children. Pediatr Transplant. 2004;8:584–8.
Lu B, Gralla J, Liu E, et al. Evaluation of a scoring system for assessing prognosis in pediatric acute liver failure. Clin Gastroenterol Hepatol. 2008;6:1140–5.
Bernal W, Wendon J, Rela M. Use and outcome of liver transplantation in acetaminophen-induced acute liver failure. Hepatology. 1998;27:1050–5.
Harrison PM, O’Grady JG, Keays RT, et al. Serial prothrombin time as prognostic indicator in paracetamol induced fulminant hepatic failure. Br Med J. 1990;301:964–6.
Pereira LM, Langley PG, Hayllar KM, et al. Coagulation factor V and VIII/V ratio as predictors of outcome in paracetamol induced fulminant hepatic failure: relation to other prognostic indicators. Gut. 1992;33:98–102.
Hoofnagle JH, Carithers RL, Shapiro C, et al. Fulminant hepatic failure: summary of a workshop. Hepatology. 1995;21:240–52.
Murray-Lyon IM, Orr AH, Gazzard B, et al. Prognostic value of serum alphafetoprotein in fulminant hepatic failure including patients treated by charcoal haemoperfusion. Gut. 1976;17:576–80.
Macquillan GC, Seyam MS, Nightingale P, et al. Blood lactate but not serum phosphate levels can predict patient outcome in fulminant hepatic failure. Liver Transpl. 2005;11:1073–9.
Schmidt LE, Dalhoff K. Serum phosphate is an early predictor of outcome in severe acetaminophen-induced hepatotoxicity. Hepatology. 2002;36:659–65.
Bernal W, Donaldson N, Wyncoll D, et al. Blood lactate as an early predictor of outcome in paracetamolinduced acute liver failure: a cohort study. Lancet. 2002;359:558–63.
Ranek L, Andreasen PB, Tygstrup N. Galactose elimination capacity as a prognostic index in patients with fulminant liver failure. Gut. 1976;17:959–64.
Bhatia V, Singh R, Acharya SK. Predictive value of arterial ammonia for complications and outcome in acute liver failure. Gut. 2006;55:98–104.
Lee WM, Galbraith RM, Watt GH, et al. Predicting survival in fulminant hepatic failure using serum Gc protein concentrations. Hepatology. 1995;21:101–5.
Schiøt FV, Bangert K, Shakil AO. Predictive value of actin-free Gc-globulin in acute liver failure. Liver Transpl. 2007;13:1324–9.
Donaldson BW, Gopinath R, Wanless IR, et al. The role of transjugular liver biopsy in fulminant liver failure: relation to other prognostic indicators. Hepatology. 1993;18:1370–4.
Malinchoc M, Kamath PS, Gordon FD, et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;3:864–71.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
D’Agostino, D., Diaz, S., Sanchez, M.C. et al. Management and Prognosis of Acute Liver Failure in Children. Curr Gastroenterol Rep 14, 262–269 (2012). https://doi.org/10.1007/s11894-012-0260-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11894-012-0260-x