Abstract
Purpose of Review
Oxidative stress describes an imbalance between production and degradation of reactive oxygen species (ROS), which can damage macromolecules. However, ROS may also serve as signaling molecules activating cellular pathways involved in cell proliferation and adaptation. This review describes alterations in metabolic diseases including obesity, insulin resistance, and/or diabetes mellitus as well as responses to acute and chronic physical exercise.
Recent Findings
Chronic upregulation of oxidative stress associates with the development of insulin resistance and type 2 diabetes (T2D). While single bouts of exercise can transiently induce oxidative stress, chronic exercise promotes favorable oxidative adaptations with improvements in muscle mitochondrial biogenesis and glucose uptake.
Summary
Although impaired antioxidant defense fails to scavenge ROS in metabolic diseases, chronic exercising can restore this abnormality. The different metabolic effects are likely due to variability of reactive species and discrepancies in temporal (acute vs. chronic) and local (subcellular distribution) patterns of production.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mitochondrial respiration generates reactive oxygen species (ROS), which are quenched by antioxidant systems. Various processes such as insulin signaling and upregulation of antioxidants, adaptive protein synthesis, and mitochondrial biogenesis depend on increased ROS generation under physiological conditions such as exercising. On the other hand, dysregulation of ROS production and removal, termed oxidative stress, occurs in numerous human disorders including type 2 diabetes (T2D) and obesity [1] and has been related to their pathogenesis and complications. This review will address detrimental effects of systemic ROS and ROS originating from skeletal muscle-inducing oxidative stress and cellular damage in the context of metabolic diseases but will also explore effects of different exercise training interventions on oxidative stress in this cohort. This review is based on a search in biomedical databases (PubMed, Quertle) for the terms “obese, insulin resistant, type 2 diabetes, ROS, human, oxidative stress” as well as “obese, insulin resistant, type 2 diabetes, acute, chronic, exercise, ROS, human, oxidative stress” and mainly focuses on studies published during the last 5 years but also addresses relevant older studies.
What Is Oxidative Stress?
The term oxidative stress has first been introduced to the biomedical research community in 1985. Oxidative stress has originally been described as a disturbance in the pro-oxidant–antioxidant balance in favor of the former, potentially leading to cellular damage [2]. After the discovery of redox pathways, this definition has been rephrased as “a disruption of redox signaling and control” [3]. Oxidative stress can also be defined as a state of temporarily or chronically elevated ROS production, ROS production is temporarily or chronically elevated, perturbing cellular metabolism and damaging cellular components [4].
ROS are chemical species produced by sequential four-electron reduction of molecular O2 through the addition of electrons at metabolically active sites such as the mitochondria or cytosolic enzymes during their catalytic activity. They comprise of superoxide anion radical (O2·−), hydrogen peroxide (H2O2), and hydroxyl radical (OH·−), which are chemically instable and have a strong tendency to react with and damage biological molecules (Fig. 1). Caloric overload can stimulate substrate flux to the mitochondria, giving rise to electron donors (NADH, FADH2) and global electron transport activity with additional electron leakage due to high membrane potential (ΔΨ). Major sites of mitochondrial net ROS emission include complex I and complex III of the electron transfer system (ETS) in the inner mitochondrial membrane, the mitochondrial glyceraldehyde-3-phosphate dehydrogenase [5] in the mitochondrial matrix, as well as the flavoprotein monoamine oxidase in the outer mitochondrial membrane [6, 7]. Other ROS emission sites include the enzymes nicotinamide adenine dinucleotide phosphate (NADPH) oxidase (Nox) [8] and nitric oxide synthase (NOS) [9] as well as enzymes that produce ROS as a byproduct, such as xanthine oxidase (XO) and lipoxygenase [10]. The process of oxidative protein folding in the endoplasmic reticulum (ER) can also serve as an important source of ROS and contributes to approximately 25% of overall cellular ROS emission [11]. ER-mediated ROS emission due to oxidative protein folding increases during augmented demand in insulin-resistant individuals due to inflammation and higher insulin biosynthesis [12].
Pathological effects of chronic oxidative stress. Major sources of reactive oxygen species (ROS) involved in the pathophysiology of insulin resistance and obesity are shown. The factors responsible for elevated chronic oxidative stress include inflammatory processes via cytokine receptors (CR), increased free-fatty acids (FFA) via Toll-like receptor (TLR), and hyperglycemia, which promote ROS emission from the NADPH oxidase system (Nox) and nitric oxide (NO) synthase (NOS) as well as xanthine oxidase (XO) and the mitochondria. Binding of advanced glycation end products (AGE) to its receptor (RAGE) can further stimulate Nox-mediated ROS release. Increased mitochondrial oxidation from nutrient overload and participation of monoamine oxidase (MAO) and mitochondrial glyceraldehyde-3-phosphate dehydrogenase (mGDPH) can contribute to excess intracellular ROS production, which can cause oxidative damage to DNA, proteins, and lipids and also activate the mitogen-activated protein kinase (MAPK) pathway and C-Jun-N-terminal kinase (JNK), contributing to impaired insulin signaling and glucose uptake. Elevated intracellular diacylglycerols (DAG) and ceramides (CER) also interfere with insulin signaling. Endoplasmic reticulum (ER) stress via the unfolded protein response (UPR) remains an important source for increased ROS generation. Calcium release from the ER can enhance cytochrome c release and interfere with electron transfer within the electron transfer system, thereby further increasing mitochondrial ROS generation. AKT protein kinase B, CI–CV mitochondrial complex I–V, ERK extracellular signal-regulated kinase, GLUT4 glucose transporter 4, IR insulin receptor, IRS insulin receptor substrate, PI3K phosphoinositide 3-kinase. Arrows denote activation, red lines indicate inhibition, and words in red represent the most important outcome of oxidative damage to cellular macromolecules
Another type of redox signaling molecule, reactive nitrogen species (RNS), is derived from ·NO, a byproduct of l-arginine-l-citrulline metabolism catalyzed by NOS isozymes. ·NO can react with superoxide to form the highly reactive peroxynitrite (ONOO−). Other RNS include the nitrogen dioxide radical (·NO2) and nitrite (NO2−). RNS may modulate cell signaling or damage cells by oxidation of biological macromolecules and nitrosylation of other proteins.
In order to detoxify these highly reactive molecules and to maintain low degrees of oxidative stress, the healthy cell relies on a large array of antioxidant defense mechanisms. They are responsible for scavenging and breaking down ROS to less or nonreactive products and include antioxidant enzymes such as superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx) as well as endogenous metabolites like bilirubin and uric acid [13]. There are three mammalian isoforms of SOD: cytosolic Cu/Zn SOD or SOD1, mitochondrial Mn-dependent SOD or SOD2, and extracellular Cu/Zn SOD or SOD3, which catalyze detoxification of O2 ·− to oxygen and H2O2 [14]. CAT catalyzes the degradation of H2O2 to water and oxygen, while GPx reduces H2O2 and lipid hydroperoxides to water or corresponding alcohols consuming reduced glutathione (GSH) [15]. Obviously, both antioxidant defense and oxidant load affect the redox balance and insufficient scavenging may be an important cause for oxidative stress.
Methods for Detecting Oxidative Stress
Previous reviews have comprehensively described the methods for assessment of oxidative stress [16,17,18]. Briefly, the challenge of measuring ROS results from their short half-life ranging from nanoseconds to seconds and their overall very low concentrations. ROS can be either detected directly or indirectly by measuring molecules that preferably react with ROS in vivo.
Direct Methods to Assess Oxidative Stress
Highly specific methods involve the trapping of O2 ·− with spin trapping reagents such as α-phenyl-N-tert-butyl nitrone (PBN) that covalently bind and form stable adducts with radicals and can be detected using quantitative electron spin resonance (ESR) [16]. Alternatively, rather unspecific spin probes can be used to detect O2 ·− in intact tissues, cells, or homogenates. These probes are oxidized to form stable radicals, which are then detectable by ESR, a method often regarded as the gold standard, although methodological limitations, high costs, and extensive training impede its broad use [19].
Alternative approaches to detect ROS in cultured cells, tissues, or isolated mitochondria rely on colorimetic, fluorimetric, or luminescence-based assays as well as enzyme activity assays. These assays follow the principle that the radical reacts with a tracer, which creates a detector compound that releases a photon. The widely used quantitative lucigenin-enhanced chemiluminescence assay uses lucigenin, a compound reasonably specific for O2 ·−[19]. Although this assay is easy to use, it is prone to artifacts and the validity has been questioned based on O2 ·− overestimation due to redox cycling of the compound [20]. Lucigenin at lower concentrations (5 μM) and other compounds such as coelenterazine, luminol, or methylated-modified cypridina luciferin analog that do not undergo redox cycling are promising probes for O2 ·− detection [19].
The widely used Amplex Red assay measures extracellular H2O2 via the horseradish peroxidase-catalyzed reaction of N-acetyl-3,7-dihydroxyphenoxazine (Amplex Red) with H2O2 in a 1:1 stoichiometry to produce the red-fluorescent oxidation product, resorufin [21]. Although this assay is highly specific and sensitive, Amplex Red is light sensitive and thereby prone to artefactual formation of resorufin at high concentrations of 50 μM [22]. Lowering the concentrations to 10 μM and minimizing light exposure makes the Amplex Red assay an accurate, sensitive, and versatile way for detecting H2O2 emission from cells, tissues, and cell-free systems.
Indirect Methods to Assess Oxidative Stress
The reaction of thiobarbituric acid (TBA) with the end product of lipid peroxidation, malondialdehyde (MDA), is among the earliest and most widely used methods for quantitative detection of lipid peroxides [23]. Although the assay is fast and technically easy to perform, TBA can also react with other saturated and unsaturated aldehydes to form unspecific TBA-reactive substances (TBARS) and possibly overestimate MDA levels. Separation of the aldehyde adducts by high-performance liquid chromatography (HPLC) has therefore been applied to improve the sensitivity and accurately quantify MDA levels in tissues and plasma [24]. Isoprostanes are other important markers of lipid peroxidation, which can be detected in all body fluids including urine [25]. F2-isoprostane, the product of peroxidation of arachidonic acid, is considered to be very accurate to quantify in vivo oxidative stress in plasma or urine [26].
8-Hydroxy-2-deoxyguanosine (8-OHdG), the main product of DNA oxidation, can easily be assessed in human DNA samples and in urine by HPLC, gas chromatography mass spectrometry (GC/MS), or enzyme-linked immunosorbent assay (ELISA) [27]. Difficulties arise from the formation of artifacts during isolation and analysis of DNA and from confounding factors such as smoking [28]. Nevertheless, 8-OHdG is an important marker for measuring the effect of endogenous oxidative damage to DNA as a biomarker of oxidative stress.
ROS-mediated protein oxidation leads to formation of carbonyl groups (aldehydes and ketones) on protein side chains, mainly of proline, arginine, lysine, and threonine [29]. These stable carbonylated proteins can be detected after derivatization of the carbonyl group with 2,4-dinitrophenylhydrazine (DNPH) and formation of dinitrophenyl (DNP) hydrazone [29]. Hydrazones are measured spectrophotometrically by ELISA and Western blotting, the latter yielding semiquantitative results. Appropriate sample handling and performing the measurement as quickly as possible help to minimize artifact formation during sample collection and analysis. Although carbonylated proteins are induced by various chemical processes and different ROS, their relatively early formation and stability (hours to days) as compared to lipid peroxidation products (minutes) make them a valuable biomarker for oxidative stress [30].
The wide array of methods to detect ROS in different biological matrices offers not only a variety of advantages but also potential drawbacks. Of note, none of these methods is generally suitable for every condition. It is therefore recommended to use at least two independent methods to improve the consistency of experimental observations regarding oxidative stress. The choice should be made considering the sensitivity of the assay in the tested biological specimen. Interest in more general effects of oxidative stress will lead to the use of less specific fluorescent probes such as Amplex Red or indirect methods to detect oxidized macromolecules. Interest in the effects of certain radical species will call for ERS or lucigenin assays. New methods such as genetically encoded ROS reporters, nanoparticle delivery systems, and nanotube ROS probes will likely advance the field by enhanced specificity and sensitivity as well as localization of radical generation [31].
Links Between Oxidative Stress and Metabolic Diseases
John Baynes was one of the first to present the hypothesis that oxidative stress could be an important mechanism contributing to the pathogenesis of diabetes, arguing that diabetes-related complications are associated with oxidative damage of proteins and lipids [32]. Subsequent studies supported this hypothesis in that increased systemic and skeletal muscle ROS production may relate to the development of several metabolic abnormalities including obesity and T2D [33, 34].
Systemic Oxidative Stress in Obesity and Insulin Resistance
Several studies reported mainly elevated oxidative stress in metabolic disorders in humans (Table 1). In obese nondiabetic humans, different parameters of fat accumulation correlate with systemic oxidative stress [35, 36]. Similarly, oxidative DNA damage is elevated in individuals with prediabetes, defined by impaired fasting blood glucose >6 mmol/l but <7 mmol/l [37]. While antioxidant capacity (SOD, CAT) is also upregulated in young obese individuals, elderly obese persons and individuals with metabolic syndrome show decreased antioxidant capacity in the face of increased systemic lipid peroxidation and protein carbonyls in parallel with altered lipoprotein metabolism and decreased antioxidant capacity, and both oxidative stress and antioxidant capacity (SOD, CAT) are upregulated in young obese individuals [38, 39]. Thus, systemic oxidative stress is present in obese and insulin-resistant individuals, which further rises with aging and progression of metabolic abnormalities due to inadequate upregulation of antioxidant defense.
Tissue-Specific Oxidative Stress in Obesity and Insulin Resistance
In a healthy cohort covering a wide range of body masses (body mass index (BMI) 18 to 37 kg/m2), vascular oxidative stress, and expression of Nox-p47phox, a Nox accessory protein involved in O2 ·− production rises with the degree of adiposity without alteration of xanthine oxidase activity [40] (Table 1). The overweight/obese group features elevated protein carbonyls despite higher vascular CAT and SOD expression, suggesting compensation for increased oxidative stress. Notably, systemic plasma markers of oxidative stress and antioxidants are not different between normal weight and overweight/obese individuals in this study [40]. Obese insulin-resistant individuals exhibit twofold higher muscle mitochondrial H2O2 emission than healthy controls, possibly related to lower protein abundance of complex I subunits as well as enzymes responsible for the oxidation of fatty acids and branched-chain amino acids [41]. A similar increase in muscle mitochondrial H2O2 emission is paralleled by a 50% reduction in the GSH/GSSG ratio in muscles of obese insulin-resistant individuals [42]. Of note, others report unchanged or even decreased rates of H2O2 emission in obese insulin-resistant individuals, but these results are difficult to interpret in the absence of data on maximal ROS production rates [43]. Nevertheless, the above observations suggest that increased fat mass and insulin resistance may favor ROS production from vascular endothelium and skeletal muscle with insufficient tissue-specific compensation by antioxidant systems, leading to increased systemic oxidative stress independent of age and hyperglycemia.
Associations of Fat Mass and Insulin Resistance With Oxidative Stress
Obese children with greater insulin resistance as assessed by the homeostasis model assessment of insulin resistance (HOMA-IR) also present with a higher degree of oxidative stress [44]. In addition to insulin resistance, circulating triglycerides and high-sensitivity C-reactive protein (hsCRP) may be involved in the relationship between adiposity and oxidative stress as adjustment for these parameters reduces the association. Indeed, elevated hsCRP strongly associates with oxidative stress independent of BMI and insulin resistance [45, 46]. Furthermore, plasma adiponectin levels are negatively associated not only with BMI and waist circumference but also with markers of systemic oxidative stress. In a population-based observational study of 5115 individuals, the positive relationship of levels of oxidative stress markers with HOMA-IR disappears for F2-isoprostane after adjustment for adiposity but remains for oxidized low-density lipoprotein (ox-LDL) [47].
Taken together, these results suggest that fat accumulation, insulin resistance, and deranged lipoprotein metabolism can contribute to increased oxidative stress independent of hyperglycemia. However, these studies do not allow to draw conclusions on causal relationships.
Systemic Oxidative Stress in T2D
T2D patients show elevated markers of oxidative DNA damage in plasma and urine [48, 49] (Table 1). Of note, oxidative DNA damage and lipid peroxidation are already present in newly-diagnosed T2D and even in prediabetic individuals, defined as fasting blood glucose between 5.5 and 7 mmol/l and hemoglobin HA1c (HbA1c) levels of 5.7 to 6.4% [50]. While individuals with impaired glucose regulation (impaired fasting glucose and impaired glucose tolerance) show similar levels of oxidative stress, but slightly reduced erythrocyte SOD activity compared to glucose-tolerant people, levels of plasma lipid peroxides, and DNA damage are elevated and total antioxidant capacity, GPx, GSH, and SOD activity are decreased in T2D [51, 52].
Tissue-Specific Oxidative Stress in T2D
Oxidative tissue damage measured as increased protein carbonyls is present in the skeletal muscle of T2D individuals in parallel with decreased SOD activity [53] (Table 1). Also, expression of heat shock protein (HSP)72 and heme oxygenase (HO)-1, genes responsible for antioxidant defense mechanisms, is markedly lower in the skeletal muscle of T2D [54] (Table 1). In T2D, muscle expression of antioxidant genes further correlates with muscle oxidative capacity and insulin-stimulated glucose disposal [54, 55].
Collectively, these results suggest that even moderate increases in blood glucose impair antioxidant defense, which leads to oxidative damage with possible deterioration of skeletal muscle function in overt diabetes.
Associations of Hyperglycemia and Diabetes With Oxidative Stress
The reduction in antioxidant defense associates negatively with whole-body insulin sensitivity. Markers of oxidative DNA damage correlate with BMI, hyperglycemia, and β-cell dysfunction and progressively increase from prediabetic (5.5 and 7 mmol/l) to diabetic conditions [37, 51]. On the other hand, the positive correlation of ox-LDL and lipid peroxidation and the negative correlation of total antioxidant levels and SOD activity with insulin resistance were found to be independent of obesity in one study [47]. In T2D, muscle expression of antioxidant genes further correlates with muscle oxidative capacity and insulin-stimulated glucose disposal [54, 55]. Finally, oxidative stress is further associated with daily and day-to-day glucose variability [54, 55]. Taken together, glycemic control is an important driving force for further accelerating oxidative stress and impairment of antioxidant defense.
Results From Diet Intervention Studies
Ingestion of a high-fat diet increases mitochondrial H2O2 emission and induces insulin resistance in healthy males [42], but not in obese insulin-resistant women [56•]. High-fat diet-induced oxidative stress in skeletal muscle also associates with reduced expression of muscle mitochondrial oxidative phosphorylation genes [42, 57]. However, comparison of a high-carbohydrate and a high-fat meal reveals that only the high-carbohydrate meal decreases total antioxidant capacity and muscle SOD, supporting the view of the deleterious role of carbohydrates and glycemia for oxidative stress [58].
On the other hand, diet-induced weight loss can decrease oxidative stress by improving antioxidant status independent of physical activity [59]. In obese women, body weight reduction not only improves insulin resistance, oxidative stress, and inflammation but also activities of antioxidant enzymes including GSH and CAT [60, 61]. Similarly, a 2-month calorie restriction by 20% resulting in 8% weight loss leads to reduction in dyslipidemia as well as markers of oxidative stress and inflammation along with improved antioxidant defense [62]. Taken together, intervention studies suggest that caloric intake and body weight changes dynamically affect oxidative stress but do not allow to identify whether oxidative stress contributes to the weight-dependent alterations in metabolism and insulin resistance.
Cellular Mechanisms Contributing to ROS Production in Human Metabolic Diseases
At least 0.2–2% of the oxygen consumed during mitochondrial respiration contributes to the generation of free radicals [63, 64] (Fig. 1). T2D patients exhibit slightly lower flux through muscle ATP synthesis as well as in muscle expression of genes involved in mitochondrial function and oxidative metabolism [65,66,67]. Incomplete mitochondrial catabolism of long-chain fatty acyl-CoA has been further associated with elevated ROS production and impaired glutathione antioxidant system [68]. Intracellular accumulation of lipid metabolism intermediates (diacylglycerols, ceramides) further impairs insulin signaling [69••]. However, the data on muscle mitochondrial function in insulin-resistant (IR) and T2D humans are not fully consistent in that some features of mitochondrial function are comparable between T2D and age-matched glucose-tolerant individuals when respiratory rates are normalized to mitochondrial DNA or citrate synthase activity.
Adipose tissue may serve as an important source of ROS: nondiabetic obese KKay mice exhibit increased lipid peroxidation and H2O2 production in white adipose tissue. Elevated circulating fatty acids could contribute to oxidative stress via NADPH oxidase activation in white adipose tissue [35]. Obesity also relates closely to ER stress [70], which, in turn, associates with oxidative stress [71]. ER-mediated ROS production is increased in both obese insulin-resistant nondiabetic persons and T2D patients [72, 73]. In the context of ER stress, unfolded protein response (UPR) leads to calcium ion leakage from ER, which interferes with electron transfer in the ETS [74] and the subsequent cytochrome c release from mitochondria can induce mitochondrial ROS production [75] (Fig. 1).
Finally, advanced glycation end products (AGEs) increase under conditions of hyperglycemia [76]. Binding of AGEs to their respective receptors (RAGE) stimulates Nox, which also generates intracellular ROS [77]. (Fig. 1).
Effects of Acute and Chronic Exercise on Oxidative Stress in Metabolic Diseases
Since the 1970s, it is known that 1 h of moderate endurance exercise can increase lipid peroxidation in humans [78]. Although the biological meaning was unknown, these results created a lot of interest over the following years about the role ROS plays during exercise. While acute exercise may induce a temporary state of oxidative stress, chronic physical activity promotes favorable oxidative adaptations [79]. Various modalities of regular exercising (endurance, resistance, or combined training) generally improve systemic markers of oxidative stress and antioxidant capacity in healthy individuals [80, 81], but its impact on oxidative stress in metabolic diseases is less clear.
Acute Exercise and Oxidative Stress in Metabolic Diseases
An acute bout of exhaustive aerobic exercise results in greater ROS production in obese than in nonobese individuals [82] (Table 2). Both intensive aerobic and resistance exercise sessions lead to excessive lipid peroxidation in obese men and women [83, 84]. However, low-intensity exercise such as walking decreases lipid peroxidation in individuals with T2D, suggesting that mild exercising is able to reduce systemic oxidative stress in T2D [85]. Of note, acute high-intensity exercise-induced oxidative stress associates with increased insulin sensitivity in obese individuals [86]. Experimental studies in myocytes mimicking acute and chronic oxidative stress support this concept [87]. During acute and oxidative stress, the mitogen-activated protein kinase (MAPK) phosphatase MKP7 relocates from the nucleus to the cytoplasm, where it dephosphorylates JNK in the cytoplasm, resulting in increased insulin sensitivity through insulin receptor substrate (IRS)-1. These results suggest that oxidative stress in response to exercise is exacerbated in individuals with metabolic diseases but may also serve as an important signal improving insulin signaling and mitochondrial biogenesis.
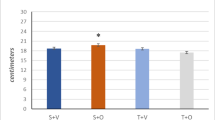
Chronic Exercising and Systemic Oxidative Stress in Obesity and Insulin Resistance
In overweight-to-obese women, 12 weeks of aerobic exercise training plus caloric restriction lowers systemic lipid peroxidation [88] (Table 2). In a similar 12-week intervention study, combined aerobic exercise and hypocaloric diet is more effective to decrease oxidative stress and improve serum antioxidant capacity than hypocaloric diet alone [89]. On the other hand, obese women feature reduction in markers of lipid peroxidation upon aerobic exercising plus caloric restriction or caloric restriction alone, but only in those individuals increasing their maximal oxygen uptake upon exercising alone [90]. Both regular aerobic and resistance training alone can improve oxidative stress and antioxidant defense in overweight individuals [81, 91]. Five weeks of combined resistance and aerobic training improve both oxidative stress and insulin resistance in insulin-resistant humans [92]. However, the combined exercise training can lead to higher oxidative lipid damage in obese individuals [92], suggesting that caution may be required when recommending combined training in persons with metabolic diseases.
Chronic Exercising and Tissue-Specific Oxidative Stress in Obesity and Insulin Resistance
As little as 2 weeks of immobilization diminishes muscle ATP production and increases muscle H2O2 emission without effects on antioxidant proteins, while a subsequent 6-week period of aerobic training not only restores ATP production and H2O2 emission to baseline levels but also increases SOD and CAT [93•] (Table 2). Likewise, a 12-week aerobic exercise training period reverses muscle mitochondrial alterations, diminishes cellular oxidative damage, and increases CAT activity in obese insulin-resistant women despite minimal weight loss [56•].
Chronic Exercising and Systemic Oxidative Stress in T2D
Chronic aerobic exercise training can reduce oxidative damage to proteins, lipids, and DNA as well as improve systemic antioxidant status in obese and T2D individuals [90, 94, 95] (Table 2). A 12-month supervised exercise training period consisting of aerobic, resistance, and flexibility training reduces some features of oxidative stress independent of changes in body weight [96••], but not systemic lipid peroxidation [97]. In obese individuals with impaired glucose tolerance, 12-weeks of mild aerobic training decreases body mass, percent body fat, and systemic lipid peroxidation and improves insulin sensitivity without affecting SOD [98]. As in insulin-resistant persons, aerobic training in combination with caloric restriction reduces oxidative stress and improves antioxidant capacity in obese glucose-intolerant persons [99]. The precise interaction between these two interventions remains to be established, as exercise training seems to provide no additional benefit when used in combination with caloric restriction [100]. Although individuals with T2D show elevated oxidative stress after maximal-intensity exercise compared to healthy individuals, 12 weeks of preconditioning with regular aerobic training markedly diminished oxidative stress in response to an acute bout of exercise in individuals with T2D [101].
Chronic Exercising and Tissue-Specific Oxidative Stress in T2D
Only a few studies have addressed the effect of exercise on muscle oxidative stress in T2D (Table 2). A 16-week period of unsupervised aerobic exercise training at moderate intensity is more effective to attenuate muscle oxidative protein damage and to increase CAT activity in obese T2D patients than exercise training at low intensity [102]. These effects occurred without changes in insulin sensitivity and body composition. On the other hand, reductions in oxidative stress related to improvements in insulin sensitivity [96••]. In another study, only interval walking training but not continuous walking training improved glycemic control without any effect on oxidative stress in T2D patients [103]. These findings indicate that the training response of oxidative stress and antioxidant defense is dependent on intensity, at least at lower levels of exercising, but again does not necessarily relate to insulin sensitivity or glycemic control.
Although the effect of exercise on oxidative stress is somewhat mixed and dependent on the metabolic disease, individuals with metabolic diseases may experience an exacerbation of oxidative stress following exercise when compared to healthy individuals. However, this increased oxidative stress may act as a preconditioning and induce upregulation in antioxidant defenses, which leads to diminished levels of oxidative stress when experiencing subsequent pro-oxidant environments [104].
Cellular Mechanisms Contributing to Exercise-Mediated ROS Production in Human Metabolic Diseases
In contrast to chronic oxidative stress in metabolic diseases, exercise-induced ROS occurs transiently, mostly limited to the duration of the exercise session. Thus, the pattern of ROS production follows the concept of hormesis, i.e., favorable biological effects at low exposures and opposite effects at higher doses. Adaption in response to exercise-induced oxidative stress renders the cell less vulnerable to successive perturbations [105]. ROS produced during higher-intensity exercise possibly promotes glucose uptake and improves glycemic control. In the mouse, repetitive contractions of extensor digitorum longus muscle stimulate glucose uptake by 300%. Contraction-stimulated, but not basal glucose uptake decreases by 50% after the addition of the antioxidant N-acetyl cysteine (NAC) [106]. Treatment with ebselen, an antioxidant reducing H2O2, similarly reduces glucose uptake, indicating a role of H2O2 generation [107]. Interestingly, these results could not be confirmed during in situ studies of NAC infusion in rats [108] and humans [109], possibly due to different NAC concentrations. Alternatively, ROS may only influence contraction-mediated glucose uptake during higher-intensity exercises with greatest ROS production [110]. Of note, treatment with the ROS scavengers and vitamins C and E surprisingly prevents exercise-induced increases in insulin sensitivity in healthy individuals, suggesting a beneficial role of ROS under exercise conditions [111].
Exercise-induced ROS also stimulates mitochondrial biogenesis and can improve mitochondrial function. Peroxisome proliferator-activated receptor gamma coactivator 1 alpha (PGC-1α) is a key regulatory factor mediating mitochondrial biogenesis [112], a process which also involves activation of AMP-activated protein kinase (AMPK) [113] (Fig. 1). Indeed, H2O2 treatment of C2C12 cells results in enhanced AMPK activation and PGC-1α promotor activity, both of which are blocked by NAC [114].
In summary, ROS generated during exercise likely mediates favorable adaptations including improvements in glucose uptake and mitochondrial biogenesis.
Conclusions
Detecting oxidative stress remains challenging, although novel developments may improve the diagnostic efficacy of ROS measurement. Nevertheless, reliable and easy-to-use biomarkers of redox homeostasis will be required to assess oxidative stress in clinical studies.
Numerous studies support the concept of a compromised balance between ROS generation and the antioxidant defense network in obesity and insulin-resistant states. The resulting chronic oxidative stress contributes to insulin resistance. Exercise training can ameliorate these effects and result in adaptive responses and improved endogenous antioxidant capacity in individuals with metabolic diseases. These changes can occur independent of relevant weight loss. Although acute exercise might induce a short-term pro-oxidative environment, regular exercise, regardless of the modality, improves cellular antioxidant capacity in obese, T2D, and IR individuals. Chronic exercise training can reduce oxidative stress, but this reduction is not necessarily related to improved insulin sensitivity and/or glycemic control.
However, the precise localization and origin of ROS in different pathological and physiological conditions and the effect of specific ROS on specific signaling pathways remain unclear. Specifically, comprehensive human studies exploring triggers for ROS generation during acute and chronic exercise and the impact of ROS on important cellular signaling pathways in the context of exercise adaptation and development of T2D are still lacking.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Matsuda M, Shimomura I. Increased oxidative stress in obesity: implications for metabolic syndrome, diabetes, hypertension, dyslipidemia, atherosclerosis, and cancer. Obesity Research & Clinical Practice. 2013;7(5):e330–41.
Sies H. Oxidative stress: introduction. oxidative stress: oxidants and antioxidants. London: Academic; 1991.
Jones DP. Redefining oxidative stress. Antioxid Redox Signal. 2006;8(9–10):1865–79. doi:10.1089/ars.2006.8.1865.
Lushchak VI. Free radicals, reactive oxygen species, oxidative stress and its classification. Chem Biol Interact. 2014;224:164–75. doi:10.1016/j.cbi.2014.10.016.
St-Pierre J, Buckingham JA, Roebuck SJ, Brand MD. Topology of superoxide production from different sites in the mitochondrial electron transport chain. J Biol Chem. 2002;277(47):44784–90. doi:10.1074/jbc.M207217200.
Orrenius S, Gogvadze V, Zhivotovsky B. Mitochondrial oxidative stress: implications for cell death. Annu Rev Pharmacol Toxicol. 2007;47:143–83. doi:10.1146/annurev.pharmtox.47.120505.105122.
Circu ML, Aw TY. Reactive oxygen species, cellular redox systems, and apoptosis. Free Radic Biol Med. 2010;48(6):749–62. doi:10.1016/j.freeradbiomed.2009.12.022.
Bedard K, Krause KH. The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev. 2007;87(1):245–313. doi:10.1152/physrev.00044.2005.
Pacher P, Beckman JS, Liaudet L. Nitric oxide and peroxynitrite in health and disease. Physiol Rev. 2007;87(1):315–424. doi:10.1152/physrev.00029.2006.
Kelley EE, Khoo NK, Hundley NJ, Malik UZ, Freeman BA, Tarpey MM. Hydrogen peroxide is the major oxidant product of xanthine oxidase. Free Radic Biol Med. 2010;48(4):493–8. doi:10.1016/j.freeradbiomed.2009.11.012.
Tu BP, Weissman JS. Oxidative protein folding in eukaryotes: mechanisms and consequences. J Cell Biol. 2004;164(3):341–6. doi:10.1083/jcb.200311055.
Salvado L, Palomer X, Barroso E, Vazquez-Carrera M. Targeting endoplasmic reticulum stress in insulin resistance. Trends in Endocrinology and Metabolism: TEM. 2015;26(8):438–48. doi:10.1016/j.tem.2015.05.007.
Brown DI, Griendling KK. Regulation of signal transduction by reactive oxygen species in the cardiovascular system. Circ Res. 2015;116(3):531–49. doi:10.1161/CIRCRESAHA.116.303584.
Fukai T, Ushio-Fukai M. Superoxide dismutases: role in redox signaling, vascular function, and diseases. Antioxid Redox Signal. 2011;15(6):1583–606. doi:10.1089/ars.2011.3999.
Margis R, Dunand C, Teixeira FK, Margis-Pinheiro M. Glutathione peroxidase family—an evolutionary overview. FEBS J. 2008;275(15):3959–70. doi:10.1111/j.1742-4658.2008.06542.x.
Dikalov SI, Harrison DG. Methods for detection of mitochondrial and cellular reactive oxygen species. Antioxid Redox Signal. 2014;20(2):372–82. doi:10.1089/ars.2012.4886.
Stephens JW, Khanolkar MP, Bain SC. The biological relevance and measurement of plasma markers of oxidative stress in diabetes and cardiovascular disease. Atherosclerosis. 2009;202(2):321–9. doi:10.1016/j.atherosclerosis.2008.06.006.
Sies H. Hydrogen peroxide as a central redox signaling molecule in physiological oxidative stress: oxidative eustress. Redox Biol. 2017;11:613–9.
Dikalov S, Griendling KK, Harrison DG. Measurement of reactive oxygen species in cardiovascular studies. Hypertension. 2007;49(4):717–27. doi:10.1161/01.HYP.0000258594.87211.6b.
Vasquez-Vivar J, Hogg N, Pritchard Jr KA, Martasek P, Kalyanaraman B. Superoxide anion formation from lucigenin: an electron spin resonance spin-trapping study. FEBS Lett. 1997;403(2):127–30.
Starkov AA. Measurement of mitochondrial ROS production. Methods Mol Biol. 2010;648:245–55. doi:10.1007/978-1-60761-756-3_16.
Zielonka J, Zielonka M, Sikora A, Adamus J, Joseph J, Hardy M, et al. Global profiling of reactive oxygen and nitrogen species in biological systems: high-throughput real-time analyses. J Biol Chem. 2012;287(5):2984–95. doi:10.1074/jbc.M111.309062.
Buege JA, Aust SD. Microsomal lipid peroxidation. Methods Enzymol. 1978;52:302–10.
Moselhy HF, Reid RG, Yousef S, Boyle SP. A specific, accurate, and sensitive measure of total plasma malondialdehyde by HPLC. J Lipid Res. 2013;54(3):852–8. doi:10.1194/jlr.D032698.
Janicka M, Kot-Wasik A, Kot J, Namiesnik J. Isoprostanes-biomarkers of lipid peroxidation: their utility in evaluating oxidative stress and analysis. Int J Mol Sci. 2010;11(11):4631–59. doi:10.3390/ijms11114631.
Roberts 2nd LJ, Morrow JD. The generation and actions of isoprostanes. Biochim Biophys Acta. 1997;1345(2):121–35.
Mayne ST. Antioxidant nutrients and chronic disease: use of biomarkers of exposure and oxidative stress status in epidemiologic research. J Nutr. 2003;133(Suppl 3):933S–40S.
Halliwell B. Why and how should we measure oxidative DNA damage in nutritional studies? How far have we come? Am J Clin Nutr. 2000;72(5):1082–7.
Dalle-Donne I, Rossi R, Giustarini D, Milzani A, Colombo R. Protein carbonyl groups as biomarkers of oxidative stress. Clinica Chimica Acta. 2003;329(1–2):23–38.
Grune T, Reinheckel T, Davies KJ. Degradation of oxidized proteins in K562 human hematopoietic cells by proteasome. J Biol Chem. 1996;271(26):15504–9.
Woolley JF, Stanicka J, Cotter TG. Recent advances in reactive oxygen species measurement in biological systems. Trends Biochem Sci. 2013;38(11):556–65. doi:10.1016/j.tibs.2013.08.009.
Baynes JW. Role of oxidative stress in development of complications in diabetes. Diabetes. 1991;40(4):405–12.
Kumashiro N, Tamura Y, Uchida T, Ogihara T, Fujitani Y, Hirose T, et al. Impact of oxidative stress and peroxisome proliferator-activated receptor gamma coactivator-1alpha in hepatic insulin resistance. Diabetes. 2008;57(8):2083–91. doi:10.2337/db08-0144.
Houstis N, Rosen ED, Lander ES. Reactive oxygen species have a causal role in multiple forms of insulin resistance. Nature. 2006;440(7086):944–8. doi:10.1038/nature04634.
Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest. 2004;114(12):1752–61. doi:10.1172/JCI21625.
Warolin J, Coenen KR, Kantor JL, Whitaker LE, Wang L, Acra SA, et al. The relationship of oxidative stress, adiposity and metabolic risk factors in healthy black and white American youth. Pediatric Obesity. 2014;9(1):43–52. doi:10.1111/j.2047-6310.2012.00135.x.
Al-Aubaidy HA, Jelinek HF. Oxidative DNA damage and obesity in type 2 diabetes mellitus. European Journal of Endocrinology/European Federation of Endocrine Societies. 2011;164(6):899–904. doi:10.1530/EJE-11-0053.
Yokota T, Kinugawa S, Yamato M, Hirabayashi K, Suga T, Takada S, et al. Systemic oxidative stress is associated with lower aerobic capacity and impaired skeletal muscle energy metabolism in patients with metabolic syndrome. Diabetes Care. 2013;36(5):1341–6. doi:10.2337/dc12-1161.
Karaouzene N, Merzouk H, Aribi M, Merzouk SA, Berrouiguet AY, Tessier C, et al. Effects of the association of aging and obesity on lipids, lipoproteins and oxidative stress biomarkers: a comparison of older with young men. Nutrition, Metabolism, and Cardiovascular Diseases: NMCD. 2011;21(10):792–9. doi:10.1016/j.numecd.2010.02.007.
Silver AE, Beske SD, Christou DD, Donato AJ, Moreau KL, Eskurza I, et al. Overweight and obese humans demonstrate increased vascular endothelial NAD(P)H oxidase-p47(phox) expression and evidence of endothelial oxidative stress. Circulation. 2007;115(5):627–37. doi:10.1161/CIRCULATIONAHA.106.657486.
Lefort N, Glancy B, Bowen B, Willis WT, Bailowitz Z, De Filippis EA, et al. Increased reactive oxygen species production and lower abundance of complex I subunits and carnitine palmitoyltransferase 1B protein despite normal mitochondrial respiration in insulin-resistant human skeletal muscle. Diabetes. 2010;59(10):2444–52. doi:10.2337/db10-0174.
Anderson EJ, Lustig ME, Boyle KE, Woodlief TL, Kane DA, Lin CT, et al. Mitochondrial H2O2 emission and cellular redox state link excess fat intake to insulin resistance in both rodents and humans. J Clin Invest. 2009;119(3):573–81.
Abdul-Ghani MA, Jani R, Chavez A, Molina-Carrion M, Tripathy D, Defronzo RA. Mitochondrial reactive oxygen species generation in obese non-diabetic and type 2 diabetic participants. Diabetologia. 2009;52(4):574–82. doi:10.1007/s00125-009-1264-4.
Codoner-Franch P, Navarro-Ruiz A, Fernandez-Ferri M, Arilla-Codoner A, Ballester-Asensio E, Valls-Belles V. A matter of fat: insulin resistance and oxidative stress. Pediatr Diabetes. 2012;13(5):392–9. doi:10.1111/j.1399-5448.2011.00847.x.
Park S, Kim M, Paik JK, Jang YJ, Lee SH, Lee JH. Oxidative stress is associated with C-reactive protein in nondiabetic postmenopausal women, independent of obesity and insulin resistance. Clin Endocrinol. 2013;79(1):65–70. doi:10.1111/j.1365-2265.2012.04512.x.
Abramson JL, Hooper WC, Jones DP, Ashfaq S, Rhodes SD, Weintraub WS, et al. Association between novel oxidative stress markers and C-reactive protein among adults without clinical coronary heart disease. Atherosclerosis. 2005;178(1):115–21. doi:10.1016/j.atherosclerosis.2004.08.007.
Park K, Gross M, Lee DH, Holvoet P, Himes JH, Shikany JM, et al. Oxidative stress and insulin resistance: the coronary artery risk development in young adults study. Diabetes Care. 2009;32(7):1302–7. doi:10.2337/dc09-0259.
Kanauchi M, Nishioka H, Hashimoto T. Oxidative DNA damage and tubulointerstitial injury in diabetic nephropathy. Nephron. 2002;91(2):327–9. 58412
Shin CS, Moon BS, Park KS, Kim SY, Park SJ, Chung MH, et al. Serum 8-hydroxy-guanine levels are increased in diabetic patients. Diabetes Care. 2001;24(4):733–7.
Kant M, Akis M, Calan M, Arkan T, Bayraktar F, Dizdaroglu M, et al. Elevated urinary levels of 8-oxo-2′-deoxyguanosine, (5′R)- and (5′S)-8,5′-cyclo-2′-deoxyadenosines, and 8-iso-prostaglandin F2alpha as potential biomarkers of oxidative stress in patients with prediabetes. DNA repair. 2016; doi:10.1016/j.dnarep.2016.09.004.
Song F, Jia W, Yao Y, Hu Y, Lei L, Lin J, et al. Oxidative stress, antioxidant status and DNA damage in patients with impaired glucose regulation and newly diagnosed type 2 diabetes. Clin Sci. 2007;112(12):599–606. doi:10.1042/CS20060323.
Dave GS, Kalia K. Hyperglycemia induced oxidative stress in type-1 and type-2 diabetic patients with and without nephropathy. Cell Mol Biol. 2007;53(5):68–78.
Bravard A, Lefai E, Meugnier E, Pesenti S, Disse E, Vouillarmet J, et al. FTO is increased in muscle during type 2 diabetes, and its overexpression in myotubes alters insulin signaling, enhances lipogenesis and ROS production, and induces mitochondrial dysfunction. Diabetes. 2011;60(1):258–68. doi:10.2337/db10-0281.
Bruce CR, Carey AL, Hawley JA, Febbraio MA. Intramuscular heat shock protein 72 and heme oxygenase-1 mRNA are reduced in patients with type 2 diabetes: evidence that insulin resistance is associated with a disturbed antioxidant defense mechanism. Diabetes. 2003;52(9):2338–45.
Ohara M, Fukui T, Ouchi M, Watanabe K, Suzuki T, Yamamoto S, et al. Relationship between daily and day-to-day glycemic variability and increased oxidative stress in type 2 diabetes. Diabetes Res Clin Pract. 2016;122:62–70. doi:10.1016/j.diabres.2016.09.025.
• Konopka AR, Asante A, Lanza IR, Robinson MM, Johnson ML, Dalla Man C, et al. Defects in mitochondrial efficiency and H2O2 emissions in obese women are restored to a lean phenotype with aerobic exercise training. Diabetes. 2015;64(6):2104–15. doi:10.2337/db14-1701. This intervention study provides evidence that impaired mitochondrial bioenergetics in obese women is restored towards that of lean, insulin-sensitive individuals 12 weeks of aerobic exercise.
Sparks LM, Xie H, Koza RA, Mynatt R, Hulver MW, Bray GA, et al. A high-fat diet coordinately downregulates genes required for mitochondrial oxidative phosphorylation in skeletal muscle. Diabetes. 2005;54(7):1926–33.
Gregersen S, Samocha-Bonet D, Heilbronn LK, Campbell LV. Inflammatory and oxidative stress responses to high-carbohydrate and high-fat meals in healthy humans. Journal of Nutrition and Metabolism. 2012;2012:238056. doi:10.1155/2012/238056.
Tumova E, Sun W, Jones PH, Vrablik M, Ballantyne CM, Hoogeveen RC. The impact of rapid weight loss on oxidative stress markers and the expression of the metabolic syndrome in obese individuals. J Obes. 2013;2013:729515. doi:10.1155/2013/729515.
Ramezanipour M, Jalali M, Sadrzade-Yeganeh H, Keshavarz SA, Eshraghian MR, Bagheri M, et al. The effect of weight reduction on antioxidant enzymes and their association with dietary intake of vitamins A, C and E. Arquivos brasileiros de endocrinologia e metabologia. 2014;58(7):744–9.
Bougoulia M, Triantos A, Koliakos G. Plasma interleukin-6 levels, glutathione peroxidase and isoprostane in obese women before and after weight loss. Association with cardiovascular risk factors. Hormones. 2006;5(3):192–9.
Johnson JB, Summer W, Cutler RG, Martin B, Hyun DH, Dixit VD, et al. Alternate day calorie restriction improves clinical findings and reduces markers of oxidative stress and inflammation in overweight adults with moderate asthma. Free Radic Biol Med. 2007;42(5):665–74. doi:10.1016/j.freeradbiomed.2006.12.005.
Chance B, Sies H, Boveris A. Hydroperoxide metabolism in mammalian organs. Physiol Rev. 1979;59(3):527–605.
Staniek K, Nohl H. H(2)O(2) detection from intact mitochondria as a measure for one-electron reduction of dioxygen requires a non-invasive assay system. Biochim Biophys Acta. 1999;1413(2):70–80.
Patti ME, Butte AJ, Crunkhorn S, Cusi K, Berria R, Kashyap S, et al. Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: potential role of PGC1 and NRF1. Proc Natl Acad Sci U S A. 2003;100(14):8466–71. doi:10.1073/pnas.1032913100.
Mootha VK, Lindgren CM, Eriksson KF, Subramanian A, Sihag S, Lehar J, et al. PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet. 2003;34(3):267–73. doi:10.1038/ng1180.
Szendroedi J, Schmid AI, Chmelik M, Toth C, Brehm A, Krssak M, et al. Muscle mitochondrial ATP synthesis and glucose transport/phosphorylation in type 2 diabetes. PLoS Med. 2007;4(5):e154. doi:10.1371/journal.pmed.0040154.
Seifert EL, Estey C, Xuan JY, Harper ME. Electron transport chain-dependent and -independent mechanisms of mitochondrial H2O2 emission during long-chain fatty acid oxidation. J Biol Chem. 2010;285(8):5748–58. doi:10.1074/jbc.M109.026203.
•• Szendroedi J, Yoshimura T, Phielix E, Koliaki C, Marcucci M, Zhang D, et al. Role of diacylglycerol activation of PKCtheta in lipid-induced muscle insulin resistance in humans. Proc Natl Acad Sci U S A. 2014;111(26):9597–602. doi:10.1073/pnas.1409229111. This paper addresses mechanisms responsible for muscle insulin resistance in humans and supports the hypothesis that activation of protein kinase Cθ by bioactive diacylglycerol and subsequent impairment of insulin signaling plays a major role in the pathogenesis of muscle insulin resistance.
Boden G. Endoplasmic reticulum stress: another link between obesity and insulin resistance/inflammation? Diabetes. 2009;58(3):518–9. doi:10.2337/db08-1746.
Sharma NK, Das SK, Mondal AK, Hackney OG, Chu WS, Kern PA, et al. Endoplasmic reticulum stress markers are associated with obesity in nondiabetic subjects. J Clin Endocrinol Metab. 2008;93(11):4532–41. doi:10.1210/jc.2008-1001.
Boden G, Duan X, Homko C, Molina EJ, Song W, Perez O, et al. Increase in endoplasmic reticulum stress-related proteins and genes in adipose tissue of obese, insulin-resistant individuals. Diabetes. 2008;57(9):2438–44. doi:10.2337/db08-0604.
Lenin R, Sankaramoorthy A, Mohan V, Balasubramanyam M. Altered immunometabolism at the interface of increased endoplasmic reticulum (ER) stress in patients with type 2 diabetes. J Leukoc Biol. 2015;98(4):615–22. doi:10.1189/jlb.3A1214-609R.
Papa FR. Endoplasmic reticulum stress, pancreatic beta-cell degeneration, and diabetes. Cold Spring Harbor Perspectives in Medicine. 2012;2(9):a007666. doi:10.1101/cshperspect.a007666.
Gorlach A, Klappa P, Kietzmann T. The endoplasmic reticulum: folding, calcium homeostasis, signaling, and redox control. Antioxid Redox Signal. 2006;8(9–10):1391–418. doi:10.1089/ars.2006.8.1391.
Nowotny K, Jung T, Hohn A, Weber D, Grune T. Advanced glycation end products and oxidative stress in type 2 diabetes mellitus. Biomol Ther. 2015;5(1):194–222. doi:10.3390/biom5010194.
Zhang M, Kho AL, Anilkumar N, Chibber R, Pagano PJ, Shah AM, et al. Glycated proteins stimulate reactive oxygen species production in cardiac myocytes: involvement of Nox2 (gp91phox)-containing NADPH oxidase. Circulation. 2006;113(9):1235–43. doi:10.1161/CIRCULATIONAHA.105.581397.
Dillard CJ, Litov RE, Savin WM, Dumelin EE, Tappel AL. Effects of exercise, vitamin E, and ozone on pulmonary function and lipid peroxidation. J Appl Physiol Respir Environ Exerc Physiol. 1978;45(6):927–32.
Veskoukis AS, Goutianos G, Paschalis V, Margaritelis NV, Tzioura A, Dipla K, et al. The rat closely mimics oxidative stress and inflammation in humans after exercise but not after exercise combined with vitamin C administration. Eur J Appl Physiol. 2016;116(4):791–804. doi:10.1007/s00421-016-3336-8.
Kim KS, Paik IY, Woo JH, Kang BY. The effect of training type on oxidative DNA damage and antioxidant capacity during three-dimensional space exercise. Medical Principles and Practice. 2010;19(2):133–41. doi:10.1159/000273075.
Dantas FF, Brasileiro-Santos Mdo S, Batista RM, do Nascimento LS, Castellano LR, Ritti-Dias RM, et al. Effect of strength training on oxidative stress and the correlation of the same with forearm vasodilatation and blood pressure of hypertensive elderly women: a randomized clinical trial. PLoS One. 2016;11(8):e0161178. doi:10.1371/journal.pone.0161178.
Roh H-T, Cho S-Y, So W-Y. Obesity promotes oxidative stress and exacerbates blood-brain barrier disruption after high-intensity exercise. J Sport Health Sci. 2016:1–6.
Vincent HK, Morgan JW, Vincent KR. Obesity exacerbates oxidative stress levels after acute exercise. Med Sci Sports Exerc. 2004;36(5):772–9.
Vincent HK, Vincent KR, Bourguignon C, Braith RW. Obesity and postexercise oxidative stress in older women. Med Sci Sports Exerc. 2005;37(2):213–9.
Haxhi J, Leto G, di Palumbo AS, Sbriccoli P, Guidetti L, Fantini C, et al. Exercise at lunchtime: effect on glycemic control and oxidative stress in middle-aged men with type 2 diabetes. Eur J Appl Physiol. 2016;116(3):573–82. doi:10.1007/s00421-015-3317-3.
Parker L, Stepto NK, Shaw CS, Serpiello FR, Anderson M, Hare DL, et al. Acute high-intensity interval exercise-induced redox signaling is associated with enhanced insulin sensitivity in obese middle-aged men. Front Physiol. 2016;7:411. doi:10.3389/fphys.2016.00411.
Berdichevsky A, Guarente L, Bose A. Acute oxidative stress can reverse insulin resistance by inactivation of cytoplasmic JNK. J Biol Chem. 2010;285(28):21581–9. doi:10.1074/jbc.M109.093633.
Bianchi VE, Ribisl PM. Reactive oxygen species response to exercise training and weight loss in sedentary overweight and obese female adults. Journal of Cardiopulmonary Rehabilitation and Prevention. 2015;35(4):263–7. doi:10.1097/HCR.0000000000000114.
Gutierrez-Lopez L, Garcia-Sanchez JR, Rincon-Viquez Mde J, Lara-Padilla E, Sierra-Vargas MP, Olivares-Corichi IM. Hypocaloric diet and regular moderate aerobic exercise is an effective strategy to reduce anthropometric parameters and oxidative stress in obese patients. Obesity Facts. 2012;5(1):12–22. doi:10.1159/000336526.
Duggan C, Tapsoba JD, Wang CY, Campbell KL, Foster-Schubert K, Gross MD, et al. Dietary weight loss, exercise, and oxidative stress in postmenopausal women: a randomized controlled trial. Cancer Prev Res. 2016;9(11):835–43. doi:10.1158/1940-6207.CAPR-16-0163.
Farinha JB, Steckling FM, Stefanello ST, Cardoso MS, Nunes LS, Barcelos RP, et al. Response of oxidative stress and inflammatory biomarkers to a 12-week aerobic exercise training in women with metabolic syndrome. Sports Medicine - Open. 2015;1(1):3. doi:10.1186/s40798-015-0011-2.
Medeiros Nda S, de Abreu FG, Colato AS, de Lemos LS, Ramis TR, Dorneles GP, et al. Effects of concurrent training on oxidative stress and insulin resistance in obese individuals. Oxidative Med Cell Longev. 2015;2015:697181. doi:10.1155/2015/697181.
• Gram M, Vigelso A, Yokota T, Helge JW, Dela F, Hey-Mogensen M. Skeletal muscle mitochondrial H2O2 emission increases with immobilization and decreases after aerobic training in young and older men. J Physiol. 2015;593(17):4011–27. doi:10.1113/JP270211. This study provides evidence that increased mitochondrial reactive oxygen species production precipitates the detrimental effects of physical inactivity.
Pittaluga M, Sgadari A, Dimauro I, Tavazzi B, Parisi P, Caporossi D. Physical exercise and redox balance in type 2 diabetics: effects of moderate training on biomarkers of oxidative stress and DNA damage evaluated through comet assay. Oxidative Med Cell Longev. 2015;2015:981242. doi:10.1155/2015/981242.
Dincer S, Altan M, Terzioglu D, Uslu E, Karsidag K, Batu S, et al. Effects of a regular exercise program on biochemical parameters of type 2 diabetes mellitus patients. The Journal of Sports Medicine and Physical Fitness. 2016;56(11):1384–91.
•• Vinetti G, Mozzini C, Desenzani P, Boni E, Bulla L, Lorenzetti I, et al. Supervised exercise training reduces oxidative stress and cardiometabolic risk in adults with type 2 diabetes: a randomized controlled trial. Scientific Reports. 2015;5:9238. doi:10.1038/srep09238. This intervention study shows that supervised exercise training was able to improve cardiorespiratory fitness, cardiometabolic risk, and oxidative stress status in individuals with type 2 diabetes.
de Oliveira VN, Bessa A, Jorge ML, Oliveira RJ, de Mello MT, De Agostini GG, et al. The effect of different training programs on antioxidant status, oxidative stress, and metabolic control in type 2 diabetes. Applied Physiology, Nutrition, and Metabolism = Physiologie appliquee, nutrition et metabolisme. 2012;37(2):334–44. doi:10.1139/h2012-004.
McNeilly AM, McClean C, Murphy M, McEneny J, Trinick T, Burke G, et al. Exercise training and impaired glucose tolerance in obese humans. J Sports Sci. 2012;30(8):725–32. doi:10.1080/02640414.2012.671952.
Kasimay O, Ergen N, Bilsel S, Kacar O, Deyneli O, Gogas D, et al. Diet-supported aerobic exercise reduces blood endothelin-1 and nitric oxide levels in individuals with impaired glucose tolerance. Journal of Clinical Lipidology. 2010;4(5):427–34. doi:10.1016/j.jacl.2010.08.001.
Wycherley TP, Brinkworth GD, Noakes M, Buckley JD, Clifton PM. Effect of caloric restriction with and without exercise training on oxidative stress and endothelial function in obese subjects with type 2 diabetes. Diabetes Obes Metab. 2008;10(11):1062–73. doi:10.1111/j.1463-1326.2008.00863.x.
Brinkmann C, Blossfeld J, Pesch M, Krone B, Wiesiollek K, Capin D, et al. Lipid-peroxidation and peroxiredoxin-overoxidation in the erythrocytes of non-insulin-dependent type 2 diabetic men during acute exercise. Eur J Appl Physiol. 2012;112(6):2277–87. doi:10.1007/s00421-011-2203-x.
Krause M, Rodrigues-Krause J, O’Hagan C, Medlow P, Davison G, Susta D, et al. The effects of aerobic exercise training at two different intensities in obesity and type 2 diabetes: implications for oxidative stress, low-grade inflammation and nitric oxide production. Eur J Appl Physiol. 2014;114(2):251–60. doi:10.1007/s00421-013-2769-6.
Karstoft K, Clark MA, Jakobsen I, Muller IA, Pedersen BK, Solomon TP, et al. The effects of 2 weeks of interval vs continuous walking training on glycaemic control and whole-body oxidative stress in individuals with type 2 diabetes: a controlled, randomised, crossover trial. Diabetologia. 2016; doi:10.1007/s00125-016-4170-6.
Lawler JM, Rodriguez DA, Hord JM. Mitochondria in the middle: exercise preconditioning protection of striated muscle. J Physiol. 2016;594(18):5161–83. doi:10.1113/JP270656.
Yun J, Finkel T. Mitohormesis. Cell Metab. 2014;19(5):757–66. doi:10.1016/j.cmet.2014.01.011.
Sandstrom ME, Zhang SJ, Bruton J, Silva JP, Reid MB, Westerblad H, et al. Role of reactive oxygen species in contraction-mediated glucose transport in mouse skeletal muscle. J Physiol. 2006;575(Pt 1):251–62. doi:10.1113/jphysiol.2006.110601.
Zhang SJ, Sandstrom ME, Aydin J, Westerblad H, Wieringa B, Katz A. Activation of glucose transport and AMP-activated protein kinase during muscle contraction in adenylate kinase-1 knockout mice. Acta Physiol. 2008;192(3):413–20. doi:10.1111/j.1748-1716.2007.01767.x.
Merry TL, Dywer RM, Bradley EA, Rattigan S, McConell GK. Local hindlimb antioxidant infusion does not affect muscle glucose uptake during in situ contractions in rat. J Appl Physiol. 2010;108(5):1275–83. doi:10.1152/japplphysiol.01335.2009.
Merry TL, Wadley GD, Stathis CG, Garnham AP, Rattigan S, Hargreaves M, et al. N-Acetylcysteine infusion does not affect glucose disposal during prolonged moderate-intensity exercise in humans. J Physiol. 2010;588(Pt 9):1623–34. doi:10.1113/jphysiol.2009.184333.
Zhang SJ, Sandstrom ME, Lanner JT, Thorell A, Westerblad H, Katz A. Activation of aconitase in mouse fast-twitch skeletal muscle during contraction-mediated oxidative stress. American Journal of Physiology Cell Physiology. 2007;293(3):C1154–9. doi:10.1152/ajpcell.00110.2007.
Ristow M, Zarse K, Oberbach A, Kloting N, Birringer M, Kiehntopf M, et al. Antioxidants prevent health-promoting effects of physical exercise in humans. Proc Natl Acad Sci U S A. 2009;106(21):8665–70. doi:10.1073/pnas.0903485106.
Safdar A, Little JP, Stokl AJ, Hettinga BP, Akhtar M, Tarnopolsky MA. Exercise increases mitochondrial PGC-1alpha content and promotes nuclear-mitochondrial cross-talk to coordinate mitochondrial biogenesis. J Biol Chem. 2011;286(12):10605–17. doi:10.1074/jbc.M110.211466.
Smith BK, Mukai K, Lally JS, Maher AC, Gurd BJ, Heigenhauser GJ, et al. AMP-activated protein kinase is required for exercise-induced peroxisome proliferator-activated receptor co-activator 1 translocation to subsarcolemmal mitochondria in skeletal muscle. J Physiol. 2013;591(6):1551–61. doi:10.1113/jphysiol.2012.245944.
Irrcher I, Ljubicic V, Hood DA. Interactions between ROS and AMP kinase activity in the regulation of PGC-1alpha transcription in skeletal muscle cells. American Journal of Physiology Cell Physiology. 2009;296(1):C116–23. doi:10.1152/ajpcell.00267.2007.
Acknowledgments
The work of the authors is supported in part by the Ministry of Science and Research of the State of North Rhine-Westphalia (MIWF NRW) and the German Federal Ministry of Health (BMG) as well as by a grant of the Federal Ministry for Research (BMBF) to the German Center for Diabetes Research (DZD e.V.; DZD Grant 2012) and by grants from the Helmholtz portfolio theme: Metabolic Dysfunction and Common Disease and the Helmholtz Alliance to Universities: Imaging and Curing Environmental Metabolic Diseases (ICEMED), the German Research Foundation (DFG, SFB 1116), German Diabetes Association (DDG), the Schmutzler-Stiftung and by the Austrian Science Fund (FWF), project no. J-3267.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dominik Pesta declares that he has no conflict of interest.
Michael Roden reports personal fees from Astra Zeneca, Eli Lilly, GI Dynamics, Merck, and Novo Nordis; grants and personal fees from Boehringer Ingelheim; grants from Novartis Pharma; and grants and personal fees from Sanofi.
Human and Animal Rights and Informed Consent
This article does not contain any studies with humans or animals performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pathogenesis of Type 2 Diabetes and Insulin Resistance
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Pesta, D., Roden, M. The Janus Head of Oxidative Stress in Metabolic Diseases and During Physical Exercise. Curr Diab Rep 17, 41 (2017). https://doi.org/10.1007/s11892-017-0867-2
Published:
DOI: https://doi.org/10.1007/s11892-017-0867-2