Abstract
Purpose of Review
To review the clinical evidence on the use of percutaneous coronary intervention (PCI) revascularization options in left main (LM) disease in comparison with coronary artery bypass graft (CABG). Coronary artery disease (CAD) involving the LM is associated with high morbidity and mortality. Though CABG remains the gold standard for complex CAD involving the LM artery, recent trials have shown a trend towards non-inferiority of the LM PCI when compared with CABG in certain subset of patients.
Recent Findings
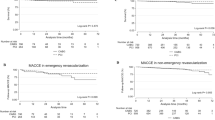
Two recent major randomized trials compared the outcomes of PCI versus CABG in the LM and multi-vessel disease with LM involvement. The NOBLE trial included patients with all range of Synergy Between Percutaneous Coronary Intervention With TAXUS and Cardiac Surgery (SYNTAX) scores and utilized biolimus drug-eluting stent (DES). The trial concluded that MACCE (major adverse cardiac and cerebrovascular event) was significantly higher with PCI (28%) when compared with CABG (18%) but overall stroke and motility were not different. EXCEL trial evaluated the same treatment option in low to intermediate SYNTAX score population with third-generation everolimus DES platform as PCI option. Results showed no significant differences in the composite primary endpoints of death, stroke, and myocardial infarction (MI) at the end of 30 days (22% versus 19.2%, p = 0.13), although repeat revascularization was higher in PCI group (16.9% versus 10%).
Summary
Recent evidence suggests that PCI is an acceptable alternative to treat symptomatic LM stenosis in select group of patients. In low to medium SYNTAX score, particularly in patients without diabetes mellitus, PCI remains a viable option. Future trials focusing on evaluating subset of patients who would benefit from one particular revascularization option in comparison with other is warranted.

Similar content being viewed by others
Abbreviations
- CAD:
-
Coronary artery disease
- PCI:
-
Percutaneous coronary intervention
- CABG:
-
Coronary artery bypass grafting
- LM:
-
Left main
- ACS:
-
Acute coronary syndrome
- ST:
-
Stent thrombosis
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011;124(23):e574–651.
Takaro T, Peduzzi P, Detre KM, Hultgren HN, Murphy ML, van der Bel-Kahn J, et al. Survival in subgroups of patients with left main coronary artery disease. Veterans Administration Cooperative Study of Surgery for Coronary Arterial Occlusive Disease. Circulation. 1982;66(1):14–22.
Ragosta M, Dee S, Sarembock IJ, Lipson LC, Gimple LW, Powers ER. Prevalence of unfavorable angiographic characteristics for percutaneous intervention in patients with unprotected left main coronary artery disease. Catheter Cardiovasc Interv. 2006;68(3):357–62.
Taggart DP, Kaul S, Boden WE, Ferguson TB Jr, Guyton RA, Mack MJ, et al. Revascularization for unprotected left main stem coronary artery stenosis stenting or surgery. J Am Coll Cardiol. 2008;51(9):885–92.
Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961–72.
El-Menyar AA, Al Suwaidi J, Holmes DR Jr. Left main coronary artery stenosis: state-of-the-art. Curr Probl Cardiol. 2007;32(3):103–93.
Rastan AJ, Boudriot E, Falk V, Kappetein AP, Borger MA, Serruys PW, et al. Frequency and pattern of de-novo three-vessel and left main coronary artery disease; insights from single center enrolment in the SYNTAX study. Eur J Cardiothorac Surg. 2008;34(2):376–82 Discussion 82-3.
Conley MJ, Ely RL, Kisslo J, Lee KL, McNeer JF, Rosati RA. The prognostic spectrum of left main stenosis. Circulation. 1978;57(5):947–52.
Thompson R. Isolated coronary ostial stenosis in women. J Am Coll Cardiol. 1986;7(5):997–1003.
Jonsson A, Ivert T, Svane B, Liska J, Jakobsson K, Hammar N. Classification of left main coronary obstruction--feasibility of surgical angioplasty and survival after coronary artery bypass surgery. Cardiovasc Surg. 2003;11(6):497–505.
Hlatky MA, Boothroyd DB, Bravata DM, Boersma E, Booth J, Brooks MM, et al. Coronary artery bypass surgery compared with percutaneous coronary interventions for multivessel disease: a collaborative analysis of individual patient data from ten randomised trials. Lancet. 2009;373(9670):1190–7.
Daemen J, Boersma E, Flather M, Booth J, Stables R, Rodriguez A, et al. Long-term safety and efficacy of percutaneous coronary intervention with stenting and coronary artery bypass surgery for multivessel coronary artery disease: a meta-analysis with 5-year patient-level data from the ARTS, ERACI-II, MASS-II, and SoS trials. Circulation. 2008;118(11):1146–54.
Stefanini GG, Holmes DR Jr. Drug-eluting coronary-artery stents. N Engl J Med. 2013;368(3):254–65.
•• Makikallio T, Holm NR, Lindsay M, Spence MS, Erglis A, Menown IB, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet. 2016;388(10061):2743–52 This trial showed that LM PCI as an option was inferior to CABG in a northern European population which was in contrast to the EXCEL trial. It also showed that patients with intermediate to high SYNTAX scores did better than those treated with CABG, whereas in those with low SYNTAX scores, CABG was a better option.
Lindstaedt M, Spiecker M, Lawo T, Yazar A, Mugge A, Bojara W, et al. Angiographic assessment of functionally insignificant left main coronary artery stenoses: reliability compared to intracoronary pressure measurement. Dtsch Med Wochenschr. 2006;131(39):2134–8.
Lindstaedt M, Spiecker M, Perings C, Lawo T, Yazar A, Holland-Letz T, et al. How good are experienced interventional cardiologists at predicting the functional significance of intermediate or equivocal left main coronary artery stenoses? Int J Cardiol. 2007;120(2):254–61.
Mintz GS, Popma JJ, Pichard AD, Kent KM, Satler LF, Chuang YC, et al. Patterns of calcification in coronary artery disease. A statistical analysis of intravascular ultrasound and coronary angiography in 1155 lesions. Circulation. 1995;91(7):1959–65.
Hamilos M, Muller O, Cuisset T, Ntalianis A, Chlouverakis G, Sarno G, et al. Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation. 2009;120(15):1505–12.
Arnett EN, Isner JM, Redwood DR, Kent KM, Baker WP, Ackerstein H, et al. Coronary artery narrowing in coronary heart disease: comparison of cineangiographic and necropsy findings. Ann Intern Med. 1979;91(3):350–6.
Leesar MA, Masden R, Jasti V. Physiological and intravascular ultrasound assessment of an ambiguous left main coronary artery stenosis. Catheter Cardiovasc Interv. 2004;62(3):349–57.
Dato I, Burzotta F, Trani C, Romano A, Paraggio L, Aurigemma C, et al. Optical coherence tomography guidance for the management of angiographically intermediate left main bifurcation lesions: early clinical experience. Int J Cardiol. 2017;248:108–13.
Jasti V, Ivan E, Yalamanchili V, Wongpraparut N, Leesar MA. Correlations between fractional flow reserve and intravascular ultrasound in patients with an ambiguous left main coronary artery stenosis. Circulation. 2004;110(18):2831–6.
Bech GJ, Droste H, Pijls NH, De Bruyne B, Bonnier JJ, Michels HR, et al. Value of fractional flow reserve in making decisions about bypass surgery for equivocal left main coronary artery disease. Heart. 2001;86(5):547–52.
Suemaru S, Iwasaki K, Yamamoto K, Kusachi S, Hina K, Hirohata S, et al. Coronary pressure measurement to determine treatment strategy for equivocal left main coronary artery lesions. Heart Vessel. 2005;20(6):271–7.
Legutko J, Dudek D, Rzeszutko L, Wizimirski M, Dubiel JS. Fractional flow reserve assessment to determine the indications for myocardial revascularisation in patients with borderline stenosis of the left main coronary artery. Kardiol Pol. 2005;63(5):499–506 Discussion 7-8.
Courtis J, Rodes-Cabau J, Larose E, Potvin JM, Dery JP, Larochelliere RD, et al. Usefulness of coronary fractional flow reserve measurements in guiding clinical decisions in intermediate or equivocal left main coronary stenoses. Am J Cardiol. 2009;103(7):943–9.
Adjedj J, De Bruyne B, Flore V, Di Gioia G, Ferrara A, Pellicano M, et al. Significance of intermediate values of fractional flow reserve in patients with coronary artery disease. Circulation. 2016;133(5):502–8.
Fearon WF, Yong AS, Lenders G, Toth GG, Dao C, Daniels DV, et al. The impact of downstream coronary stenosis on fractional flow reserve assessment of intermediate left main coronary artery disease: human validation. JACC Cardiovasc Interv. 2015;8(3):398–403.
Gotberg M, Frobert O. Instantaneous wave-free ratio versus fractional flow reserve. N Engl J Med. 2017;377(16):1596–7.
Davies JE, Sen S, Dehbi HM, Al-Lamee R, Petraco R, Nijjer SS, et al. Use of the instantaneous wave-free ratio or fractional flow reserve in PCI. N Engl J Med. 2017;376(19):1824–34.
Salvatore De Rosa AP, De Velli G, Conte M, Sabato Sorrentino CS, Mongiardo A, Sabatino J, Contarini M , Todaroand D, Indolfi C Reliability of instantaneous wave-free ratio (iFR) for the evaluation of left main coronary artery lesions. J Clin Med. 2019;8.
Norgaard BL, Terkelsen CJ, Mathiassen ON, Grove EL, Botker HE, Parner E, et al. Coronary CT angiographic and flow reserve-guided management of patients with stable ischemic heart disease. J Am Coll Cardiol. 2018;72(18):2123–34.
de la Torre Hernandez JM, Baz Alonso JA, Gomez Hospital JA, Alfonso Manterola F, Garcia Camarero T, Gimeno de Carlos F, et al. Clinical impact of intravascular ultrasound guidance in drug-eluting stent implantation for unprotected left main coronary disease: pooled analysis at the patient-level of 4 registries. JACC Cardiovasc Interv. 2014;7(3):244–54.
Park SJ, Kim YH, Park DW, Lee SW, Kim WJ, Suh J, et al. Impact of intravascular ultrasound guidance on long-term mortality in stenting for unprotected left main coronary artery stenosis. Circ Cardiovasc Interv. 2009;2(3):167–77.
Zhang J, Gao X, Kan J, Ge Z, Han L, Lu S, et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: the ULTIMATE trial. J Am Coll Cardiol. 2018;72(24):3126–37.
Abizaid AS, Mintz GS, Abizaid A, Mehran R, Lansky AJ, Pichard AD, et al. One-year follow-up after intravascular ultrasound assessment of moderate left main coronary artery disease in patients with ambiguous angiograms. J Am Coll Cardiol. 1999;34(3):707–15.
Fassa AA, Wagatsuma K, Higano ST, Mathew V, Barsness GW, Lennon RJ, et al. Intravascular ultrasound-guided treatment for angiographically indeterminate left main coronary artery disease: a long-term follow-up study. J Am Coll Cardiol. 2005;45(2):204–11.
Okabe T, Mintz GS, Lee SY, Lee B, Roy P, Steinberg DH, et al. Five-year outcomes of moderate or ambiguous left main coronary artery disease and the intravascular ultrasound predictors of events. J Invasive Cardiol. 2008;20(12):635–9.
Rathod KS, Hamshere SM, Jones DA, Mathur A. Intravascular ultrasound versus optical coherence tomography for coronary artery imaging-apples and oranges? Interv Cardiol. 2015;10(1):8–15.
•• Stone GW, Kappetein AP, Sabik JF, Pocock SJ, Morice MC, Puskas J, et al. Five-year outcomes after PCI or CABG for left main coronary disease. N Engl J Med. 2019; An important trial determining the safety and feasibility of left main coronary artery PCI, and this trial also showed that LM PCI was non-inferior to CABG over a period of 5 years.
Buszman PE, Buszman PP, Banasiewicz-Szkrobka I, Milewski KP, Zurakowski A, Orlik B, et al. Left main stenting in comparison with surgical revascularization: 10-year outcomes of the (left main coronary artery stenting) LE MANS trial. JACC Cardiovasc Interv. 2016;9(4):318–27.
Buszman PE, Buszman PP, Kiesz RS, Bochenek A, Trela B, Konkolewska M, et al. Early and long-term results of unprotected left main coronary artery stenting: the LE MANS (left main coronary artery stenting) registry. J Am Coll Cardiol. 2009;54(16):1500–11.
Buszman PE, Kiesz SR, Bochenek A, Peszek-Przybyla E, Szkrobka I, Debinski M, et al. Acute and late outcomes of unprotected left main stenting in comparison with surgical revascularization. J Am Coll Cardiol. 2008;51(5):538–45.
Boudriot E, Thiele H, Walther T, Liebetrau C, Boeckstegers P, Pohl T, et al. Randomized comparison of percutaneous coronary intervention with sirolimus-eluting stents versus coronary artery bypass grafting in unprotected left main stem stenosis. J Am Coll Cardiol. 2011;57(5):538–45.
Ahn JM, Roh JH, Kim YH, Park DW, Yun SC, Lee PH, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease: 5-year outcomes of the PRECOMBAT study. J Am Coll Cardiol. 2015;65(20):2198–206.
Park SJ, Kim YH, Park DW, Yun SC, Ahn JM, Song HG, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med. 2011;364(18):1718–27.
Morice MC, Serruys PW, Kappetein AP, Feldman TE, Stahle E, Colombo A, et al. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial. Circulation. 2014;129(23):2388–94.
•• Morice MC, Serruys PW, Kappetein AP, Feldman TE, Stahle E, Colombo A, et al. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010;121(24):2645–53 This trial forms the backbone of all soceital guideline recommendations which are currently followed by major professional cardiology and cardiothoracic surgery societies worldwide.
Stone GW, Sabik JF, Serruys PW, Simonton CA, Genereux P, Puskas J, et al. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med. 2016;375(23):2223–35.
En Chen WC, Chen L-l. Crush versus culotte stenting techniques for coronary bifurcation lesions A systematic review and meta-analysis of clinical trials with long-term follow-up. Medicine. 2019;98.
Chen SL, Zhang JJ, Han Y, Kan J, Chen L, Qiu C, et al. Double kissing crush versus provisional stenting for left main distal bifurcation lesions: DKCRUSH-V randomized trial. J Am Coll Cardiol. 2017;70(21):2605–17.
Chen SL, Xu B, Han YL, Sheiban I, Zhang JJ, Ye F, et al. Clinical outcome after DK crush versus culotte stenting of distal left main bifurcation lesions: the 3-year follow-up results of the DKCRUSH-III study. JACC Cardiovasc Interv. 2015;8(10):1335–42.
Gyldenkerne C, Olesen KKW, Jensen LO, Junker A, Veien KT, Terkelsen CJ, et al. Everolimus-eluting versus biolimus-eluting coronary stent implantation in patients with and without diabetes mellitus. Am J Cardiol. 2019;124(5):671–7.
Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. 2016 ACC/AHA Guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: an update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA Guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC Guideline for the management of patients with non-ST-elevation acute coronary syndromes, and 2014 ACC/AHA Guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Circulation. 2016;134(10):e123–55.
Fihn SD, Blankenship JC, Alexander KP, Bittl JA, Byrne JG, Fletcher BJ, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Thorac Cardiovasc Surg. 2015;149(3):e5–23.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60(16):1581–98.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138(20):e618–e51.
Cavalcante R, Sotomi Y, Lee CW, Ahn JM, Farooq V, Tateishi H, et al. Outcomes after percutaneous coronary intervention or bypass surgery in patients with unprotected left main disease. J Am Coll Cardiol. 2016;68(10):999–1009.
Valle JA, Tamez H, Abbott JD, Moussa ID, Messenger JC, Waldo SW, et al. Contemporary use and trends in unprotected left main coronary artery percutaneous coronary intervention in the United States: an analysis of the National Cardiovascular Data Registry Research to practice initiative. JAMA Cardiol. 2019;4(2):100–9.
Head SJ, Milojevic M, Daemen J, Ahn JM, Boersma E, Christiansen EH, et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet. 2018;391(10124):939–48.
Sardar P, Giri J, Elmariah S, Chatterjee S, Kolte D, Kundu A, et al. Meta-analysis of drug-eluting stents versus coronary artery bypass grafting in unprotected left main coronary narrowing. Am J Cardiol. 2017;119(11):1746–52.
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165.
Rihal CS, Naidu SS, Givertz MM, Szeto WY, Burke JA, Kapur NK, et al. 2015 SCAI/ACC/HFSA/STS clinical expert consensus statement on the use of percutaneous mechanical circulatory support devices in cardiovascular care: endorsed by the American Heart Association, the Cardiological Society of India, and Sociedad Latino Americana de Cardiologia Intervencionista; affirmation of value by the Canadian Association of Interventional Cardiology-Association Canadienne de Cardiologie d’intervention. J Am Coll Cardiol. 2015;65(19):2140–1.
Sukiennik A, Kasprzak M, Mazurek W, Niezgoda P, Bednarczyk L, Kubica J. High-risk percutaneous coronary intervention with Impella CP hemodynamic support. A case series and method presentation. Postepy Kardiol Interwencyjnej. 2017;13(1):67–71.
O’Neill WW, Kleiman NS, Moses J, Henriques JP, Dixon S, Massaro J, et al. A prospective, randomized clinical trial of hemodynamic support with Impella 2.5 versus intra-aortic balloon pump in patients undergoing high-risk percutaneous coronary intervention: the PROTECT II study. Circulation. 2012;126(14):1717–27.
Alazzoni A, Al-Saleh A, Jolly SS. Everolimus-eluting versus paclitaxel-eluting stents in percutaneous coronary intervention: meta-analysis of randomized trials. Thrombosis. 2012;2012:126369. https://doi.org/10.1155/2012/126369
Stone GW, Midei M, Newman W, Sanz M, Hermiller JB, Williams J, et al. Comparison of an everolimus-eluting stent and a paclitaxel-eluting stent in patients with coronary artery disease: a randomized trial. JAMA. 2008;299(16):1903–13.
Colombo A, Bramucci E, Sacca S, Violini R, Lettieri C, Zanini R, et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (coronary bifurcations: application of the crushing technique using sirolimus-eluting stents) study. Circulation. 2009;119(1):71–8.
Maeng M, Holm NR, Erglis A, Kumsars I, Niemela M, Kervinen K, et al. Long-term results after simple versus complex stenting of coronary artery bifurcation lesions: Nordic bifurcation study 5-year follow-up results. J Am Coll Cardiol. 2013;62(1):30–4.
Hildick-Smith D, de Belder AJ, Cooter N, Curzen NP, Clayton TC, Oldroyd KG, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British bifurcation coronary study: old, new, and evolving strategies. Circulation. 2010;121(10):1235–43.
Farooq V, Serruys PW, Garcia-Garcia HM, Zhang Y, Bourantas CV, Holmes DR, et al. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J Am Coll Cardiol. 2013;61(3):282–94.
Clark RE, The STS. Cardiac Surgery National Database: an update. Ann Thorac Surg. 1995;59(6):1376–80 Discussion 80-1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Harsha S. Nagarajarao, Chandra P. Ojha, Venkatachalam Mulukutla, Ahmed Ibrahim, Adriana C. Mares, and Timir K. Paul declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Ischemic Heart Disease
Rights and permissions
About this article
Cite this article
Nagarajarao, H.S., Ojha, C.P., Mulukutla, V. et al. Current Use and Trends in Unprotected Left Main Coronary Artery Percutaneous Intervention. Curr Cardiol Rep 22, 16 (2020). https://doi.org/10.1007/s11886-020-1268-8
Published:
DOI: https://doi.org/10.1007/s11886-020-1268-8