Abstract
Purpose of Review
Interstitial cystitis (IC) and IC-related conditions such as painful bladder syndrome (PBS), bladder pain syndrome (BPS), and hypersensitive bladder (HSB) have a similar symptomatic profile but probably different etiologies. A reasonable classification of these diseases/conditions is mandatory for clinical and investigational progress. We reviewed definition of current terminology and recent research evidence regarding IC and related conditions to propose a sensible classification system.
Recent Findings
The condition with Hunner lesions (Hunner type IC: HIC) is obviously distinct from other categories in terms of histopathology, gene expression, and clinical management; HIC is a bladder-centric disease with heavy inflammation, epithelial denudation, and oligoclonal B cell expansion. Presence of glomerulations or mucosal bleeding after distension appears of least clinical significance. Classification should thus clearly differentiate the condition with Hunner lesions from those without Hunner lesions. The term covering patients as a whole should contain IC, since IC is historically a well-known name and used for insurance reimbursement.
Summary
The proposed classification/taxonomy features an umbrella term (IC/BPS) and two sub-groups, HIC (IC/BPS with Hunner lesions) and BPS (IC/BPS without Hunner lesions). IC/BPS is convenient for the initial management of symptomatic patients, and sub-groups can categorize the patients for the specific management. The characteristic symptom profile of bladder pain, urinary urgency, and increased urinary frequency is to be collectively termed as hypersensitive bladder symptoms.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21:167–78.
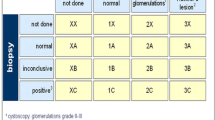
van de Merwe JP, Nordling J, Bouchelouche P, Bouchelouche K, Cervigni M, Daha LK, et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal. Eur Urol. 2008;53:60–7.
Hanno PM, Erickson D, Moldwin R, Faraday MM, American UA. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193:1545–53.
Homma Y, Ueda T, Tomoe H, Lin AT, Kuo HC, Lee MH, et al. Clinical guidelines for interstitial cystitis and hypersensitive bladder updated in 2015. Int J Urol. 2016;23:542–9.
Meijlink JM. Patient-centred standardization in interstitial cystitis/bladder pain syndrome-a PLEA. Transl Androl Urol. 2015;4:499–505.
Meijlink JM. Interstitial cystitis and the painful bladder: a brief history of nomenclature, definitions and criteria. Int J Urol. 2014;21(Suppl 1):4–12.
Hanno PM, Landis JR, Matthews-Cook Y, Kusek J, Nyberg L Jr. The diagnosis of interstitial cystitis revisited: lessons learned from the National Institutes of Health Interstitial Cystitis Database study. J Urol. 1999;161:553–7.
Castro-Diaz D, Cardozo L, Chapple CR, Espuna M, Kelleher C, Kirby M, et al. Urgency and pain in patients with overactive bladder and bladder pain syndrome. What are the differences? Int J Clin Pract. 2014;68:356–62.
Yamada Y, Nomiya A, Niimi A, Igawa Y, Ito T, Tomoe H, et al. A survey on clinical practice of interstitial cystitis in Japan. Transl Androl Urol. 2015;4:486–90.
•• Maeda D, Akiyama Y, Morikawa T, Kunita A, Ota Y, Katoh H, et al. Hunner-type (classic) interstitial cystitis: a distinct inflammatory disorder characterized by pancystitis, with frequent expansion of clonal B-cells and epithelial denudation. PLoS One. 2015;10:e0143316 Quantitative assessment of histological changes of interstitial cystitis with Hunner lesions.
• Akiyama Y, Morikawa T, Maeda D, Shintani Y, Niimi A, Nomiya A, et al. Increased CXCR3 expression of infiltrating plasma cells in Hunner type interstitial cystitis. Sci Rep. 2016;6:28652 Characterization of inflammatory cells infiltrating the bladder of interstitial cystitis with Hunner lesions.
Logadottir Y, Delbro D, Fall M, Gjertsson I, Jirholt P, Lindholm C, et al. Cytokine expression in patients with bladder pain syndrome/interstitial cystitis ESSIC type 3C. J Urol. 2014;192:1564–8.
• Offiah I, Didangelos A, Dawes J, Cartwright R, Khullar V, Bradbury EJ, et al. The expression of inflammatory mediators in bladder pain syndrome. Eur Urol. 2016;70:283–90 Overexpression of multiple inflammatory mediators in interstitial cystitis with Hunner lesions.
Gamper M, Viereck V, Geissbuhler V, Eberhard J, Binder J, Moll C, et al. Gene expression profile of bladder tissue of patients with ulcerative interstitial cystitis. BMC Genomics. 2009;10:199.
• Gamper M, Viereck V, Eberhard J, Binder J, Moll C, Welter J, et al. Local immune response in bladder pain syndrome/interstitial cystitis ESSIC type 3C. Int Urogynecol J. 2013;(24):2049–57 Active immunological responses in the bladder of interstitial cystitis with Hunner lesions.
Tseng LH, Chen I, Wang CN, Lin YH, Lloyd LK, Lee CL. Genome-based expression profiling study of Hunner’s ulcer type interstitial cystitis: an array of 40-gene model. Int Urogynecol J. 2010;21:911–8.
•• Akiyama Y, Maeda D, Katoh H, Morikawa T, Niimi A, Nomiya A, Sato Y, Kawai T, Goto A, Fujimura T, Fukuhara H, Nakagawa T, Igawa Y, Ishikawa S, Fukayama M, Kume H, Homma Y. Molecular taxonomy of interstitial cystitis/bladder pain syndrome based on whole transcriptome profiling by next-generation RNA sequencing of bladder mucosal biopsies. J Urol. 2019;202:290-300. Distinct transcriptome profiling of intersitial cystitis with Hunner lesions.
• Wennevik GE, Meijlink JM, Hanno P, Nordling J. The role of glomerulations in bladder pain syndrome: a review. J Urol. 2016;195:19–25 A review article to evaluate diagnositic value of glomerulations or mucosal bleeding after distension.
Akiyama Y, Homma Y, Maeda D. Pathology and terminology of interstitial cystitis/bladder pain syndrome: a review. Histol Histopathol. 2019;34:25–32.
Akiyama Y, Niimi A, Nomiya A, Yamada Y, Nakagawa T, Fujimura T, et al. Extent of Hunner lesions: the relationships with symptom severity and clinical parameters in Hunner type interstitial cystitis patients. Neurourol Urodyn. 2018;37:1441–7.
Chennamsetty A, Khourdaji I, Goike J, Killinger KA, Girdler B, Peters KM. Electrosurgical management of Hunner ulcers in a referral center’s interstitial cystitis population. Urology. 2015;85:74–8.
Cox M, Klutke JJ, Klutke CG. Assessment of patient outcomes following submucosal injection of triamcinolone for treatment of Hunner’s ulcer subtype interstitial cystitis. Can J Urol. 2009;16:4536–40.
Ogawa T, Ishizuka O, Ueda T, Tyagi P, Chancellor MB, Yoshimura N. Pharmacological management of interstitial cystitis /bladder pain syndrome and the role cyclosporine and other immunomodulating drugs play. Expert Rev Clin Pharmacol. 2018;11:495–505.
Van Moh F, Vetter J, Lai HH. Comparison of urologic and non-urologic presentation in interstitial cystitis/bladder pain syndrome patients with and without Hunner lesions. Neurourol Urodyn. 2018;37:2911–8.
Lai HH, Vetter J, Jain S, Gereau RW, Andriole GL. The overlap and distinction of self-reported symptoms between interstitial cystitis/bladder pain syndrome and overactive bladder: a questionnaire based analysis. J Urol. 2014;192:1679–85.
Regauer S, Gamper M, Fehr MK, Viereck V. Sensory hyperinnervation distinguishes bladder pain syndrome/interstitial cystitis from overactive bladder syndrome. J Urol. 2017;197:159–66.
Homma Y, Nomiya A, Tagaya M, Oyama T, Takagaki K, Nishimatsu H, et al. Increased mRNA expression of genes involved in pronociceptive inflammatory reactions in bladder tissue of interstitial cystitis. J Urol. 2013;190:1925–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Yukio Homma has received speaker honorarium from Astellas, Nippon Chemiphar, and Pfizer, outside the submitted work.
Yasuhiko Igawa has received grants from Kissei, Kyorin, RaQualia, Nippon-Shinyaku, Astellas, Lilium Otuka, Takeda, Tsukada Research Medical, Integral, and Medicon, outside the submitted work. Yasuhiko Igawa has received speaker honorarium from Kissei, Kyorin, Nippon-Shinyaku, Astellas, outside the submitted work.
Yoshiyuki Akiyama, Aya Niimi, and Akira Nomiya declare that they have no conflict interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on BPS/Interstitial Cystitis
Rights and permissions
About this article
Cite this article
Homma, Y., Akiyama, Y., Niimi, A. et al. Classification, Characterization, and Sub-Grouping of Interstitial Cystitis. Curr Bladder Dysfunct Rep 14, 294–300 (2019). https://doi.org/10.1007/s11884-019-00542-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-019-00542-7