Abstract
Purpose of Review
To highlight the gender-based differences in presentation and disparities in care for women with familial hypercholesterolemia (FH).
Recent Findings
Women with FH experience specific barriers to care including underrepresentation in research, significant underappreciation of risk, and interrupted therapy during childbearing. National and international registry and clinical trial data show significant healthcare disparities for women with FH. Women with FH are less likely to be on guideline-recommended high-intensity statin medications and those placed on statins are more likely to discontinue them within their first year. Women with FH are also less likely to be on regimens including non-statin agents such as PCSK9 inhibitors. As a result, women with FH are less likely to achieve target low-density lipoprotein cholesterol (LDL-C) targets, even those with prior atherosclerotic cardiovascular disease (ASCVD).
Summary
FH is common, under-diagnosed, and under-treated. Disparities of care are more pronounced in women than men. Additionally, FH weighs differently on women throughout the course of their lives starting from choosing contraceptives as young girls along with lipid-lowering therapy, timing pregnancy, choosing breastfeeding or resumption of therapy, and finally deciding goals of care during menopause. Early identification and appropriate treatment prior to interruptions of therapy for childbearing can lead to marked reduction in morbidity and mortality. Women access care differently than men and increasing awareness among all providers, especially cardio-obstetricians, may improve diagnostic rates. Understanding the unique challenges women with FH face is crucial to close the gaps in care they experience.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
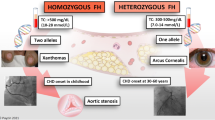
• Onorato A, Sturm AC. Heterozygous familial hypercholesterolemia. Circulation. 2016;133(14):e587–9 Comprehensive review on the diagnosis and treatment of familial hypercholesterolemia.
Gidding SS, Champagne MA, de Ferranti SD, Defesche J, Ito MK, Knowles JW, et al. The agenda for familial hypercholesterolemia. Circulation. 2015;132(22):2167–92.
•• Amrock SM, et al. Health disparities among adult patients with a phenotypic diagnosis of familial hypercholesterolemia in the CASCADE-FH patient registry. Atherosclerosis. 2017;267:19–26 Provides analysis of gender and racial disparities of data obtained from the CASCADE-FH, highlighting biases that lead to later diagnosis and less aggressive treatment of familial hypercholesterolemia in the USA.
Turgeon RD, Barry AR, Pearson GJ. Familial hypercholesterolemia. Review of diagnosis, screening, and treatment. 2016;62(1):32–7.
• Mundal L, et al. Cardiovascular disease in patients with genotyped familial hypercholesterolemia in Norway during 1994-2009, a registry study. Eur J Prev Cardiol. 2016;23(18):1962–9 Describes the difference in the incidence and prevalence of cardiovascular disease between men and women with familial hypercholesterolemia in Norway.
• McSweeney JC, et al. Preventing and experiencing ischemic heart disease as a woman: state of the science. Circulation. 2016;133(13):1302–31 Comprehensive review of research related to the diagnosis and treatment of women with ischemic heart disease.
Victor BM, Teal V, Ahedor L, Karalis DG. Gender differences in achieving optimal lipid goals in patients with coronary artery disease. Am J Cardiol. 2014;113(10):1611–5.
Schoen MW, Tabak RG, Salas J, Scherrer JF, Buckhold FR. Comparison of adherence to guideline-based cholesterol treatment goals in men versus women. Am J Cardiol. 2016;117(1):48–53.
Hammond G, Mochari-Greenberger H, Liao M, Mosca L. Effect of gender, caregiver, on cholesterol control and statin use for secondary prevention among hospitalized patients with coronary heart disease. Am J Cardiol. 2012;110(11):1613–8.
Rodriguez F, Olufade T, Heithoff K, Friedman HS, Navaratnam P, Foody JAM. Frequency of high-risk patients not receiving high-potency statin (from a large managed care database). Am J Cardiol. 2015;115(2):190–5.
O’Brien EC, et al. Rationale and design of the familial hypercholesterolemia foundation CAscade SCreening for Awareness and DEtection of Familial Hypercholesterolemia registry. Am Heart J. 2014;167(3):342–349.e17.
Daugherty SL, et al. Implicit gender bias and the use of cardiovascular tests among cardiologists. J Am Heart Assoc. 2017;6(12):e006872.
Ahmad ZS, Andersen RL, Andersen LH, O’Brien EC, Kindt I, Shrader P, et al. US physician practices for diagnosing familial hypercholesterolemia: data from the CASCADE-FH registry. J Clin Lipidol. 2016;10(5):1223–9.
•• Singh, A., et al., Familial hypercholesterolemia among young adults with myocardial infarction. J Am Coll Cardiol, 2019. 73(19): p. 2439–2450. Approximately 10% of patients younger than 50 years old with a history of myocardial infarctions had familial hypercholesterolemia, stressing the importance of FH screening in young adults with ischemic heart disease.
Al-Rasadi K, et al. The gulf familial hypercholesterolemia registry (gulf FH): design, rationale and preliminary results. Curr Vasc Pharmacol. 2020;18(1):57–64.
Beliard S, et al. High burden of recurrent cardiovascular events in heterozygous familial hypercholesterolemia: the French Familial Hypercholesterolemia Registry. Atherosclerosis. 2018;277:334–40.
Rizos CV, Elisaf MS, Skoumas I, Tziomalos K, Kotsis V, Rallidis L, et al. Characteristics and management of 1093 patients with clinical diagnosis of familial hypercholesterolemia in Greece: data from the Hellenic Familial Hypercholesterolemia Registry (HELLAS-FH). Atherosclerosis. 2018;277:308–13.
Robinson JG, Farnier M, Krempf M, Bergeron J, Luc G, Averna M, et al. Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372(16):1489–99.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379(22):2097–107.
Raal FJ, Stein EA, Dufour R, Turner T, Civeira F, Burgess L, et al. PCSK9 inhibition with evolocumab (AMG 145) in heterozygous familial hypercholesterolaemia (RUTHERFORD-2): a randomised, double-blind, placebo-controlled trial. Lancet. 2015;385(9965):331–40.
•• Ray KK, et al. Safety and efficacy of bempedoic acid to reduce LDL cholesterol. N Engl J Med. 2019;380(11):1022–32 Inclisiran, an siRNA molecule that targets PCSK-9, given at one or two doses, was associated with a 20% reduction of LDL at 1-year follow-up.
• Bhatt DL, et al. REDUCE-IT USA. Circulation. 2020;141(5):367–75 Trial studying the use of icosapent ethyl (icosapent ethyl provided a 30% relative risk reduction and a 2.6% absolute risk reduction in all-cause mortality (P = .004)).
•• Duell PB, et al. Longitudinal low density lipoprotein cholesterol goal achievement and cardiovascular outcomes among adult patients with familial hypercholesterolemia: the CASCADE FH registry. Atherosclerosis. 2019;289:85–93 Women with FH were less likely to achieve LDL goals than men.
Wong B, Kruse G, Kutikova L, Ray KK, Mata P, Bruckert E. Cardiovascular disease risk associated with familial hypercholesterolemia: a systematic review of the literature. Clin Ther. 2016;38(7):1696–709.
FH diagnosis by FH foundation. April 17, 2020]; Available from: https://apps.apple.com/us/app/fh-diagnosis/id543676258.
Mihalopoulos NL, Stipelman C, Hemond J, Brown LL, Young PC. Universal lipid screening in 9- to 11-year-olds before and after 2011 guidelines. Acad Pediatr. 2018;18(2):196–9.
• de Ferranti SD, et al. Cholesterol screening and treatment practices and preferences: a survey of United States pediatricians. J Pediatr. 2017;185:99–105.e2 Lipid screening practices among the pediatric population are not ideal.
Knowles JW, Rader DJ, Khoury MJ. Cascade screening for familial hypercholesterolemia and the use of genetic testing. JAMA. 2017;318(4):381–2.
• Wald DS, et al. Child–parent familial hypercholesterolemia screening in primary care. N Engl J Med. 2016;375(17):1628–37 Routine testing of pediatric patients for hypercholesterolemia was shown to be an effective way of identifying children with familial hypercholesterolemia.
Keenan KF, Finnie RM, Simpson WG, McKee L, Dean J, Miedzybrodzka Z. Parents’ views of genetic testing and treatment of familial hypercholesterolemia in children: a qualitative study. J Community Genet. 2019;10(1):129–41.
Sturm AC, Knowles JW, Gidding SS, Ahmad ZS, Ahmed CD, Ballantyne CM, et al. Clinical genetic testing for familial hypercholesterolemia: JACC scientific expert panel. J Am Coll Cardiol. 2018;72(6):662–80.
Gautschi M, Pavlovic M, Nuoffer J-M. Fatal myocardial infarction at 4.5 years in a case of homozygous familial hypercholesterolaemia. JIMD Rep. 2012;2:45–50.
Ekici F, Özçobanoğlu S, Kardelen F. Premature coronary artery disease due to homozygous familial hypercholesterolemia in a 12-year-old girl. Balkan Med J. 2018;35(2):208–11.
Kumar AA, Shantha G, Srinivasan Y, Senthil N, Rajkumar K, Paunikar N, et al. Acute myocardial infarction in an 18 year old South Indian girl with familial hypercholesterolemia: a case report. Cases J. 2008;1(1):71.
Wiegman A, Gidding SS, Watts GF, Chapman MJ, Ginsberg HN, Cuchel M, et al. Familial hypercholesterolaemia in children and adolescents: gaining decades of life by optimizing detection and treatment. Eur Heart J. 2015;36(36):2425–37.
Holven KB, et al. Sex differences in cholesterol levels from birth to 19 years of age may lead to increased cholesterol burden in females with FH. J Clin Lipidol. 2018;12(3):748–755.e2.
• Kusters DM, et al. Ten-year follow-up after initiation of statin therapy in children with familial hypercholesterolemia. JAMA. 2014;312(10):1055–7 Ten-year follow-up to a randomized controlled study showed that long-term pravastatin use was safe and effective in preventing worsening of carotid intima-media thickness in children with FH.
https://www.cdc.gov/reproductivehealth/contraception/mmwr/mec/appendixa_tables.html. Accessed 7 May 2020.
Toleikyte I, Retterstøl K, Leren TP, Iversen PO. Pregnancy outcomes in familial hypercholesterolemia. Circulation. 2011;124(15):1606–14.
Pugh SJ, Schisterman EF, Browne RW, Lynch AM, Mumford SL, Perkins NJ, et al. Preconception maternal lipoprotein levels in relation to fecundability. Hum Reprod. 2017;32(5):1055–63.
Wang S, Wang J, Jiang Y, Jiang W. Association between blood lipid level and embryo quality during in vitro fertilization. Medicine. 2020;99(13):e19665.
Napoli C, Glass CK, Witztum JL, Deutsch R, D’Armiento FP, Palinski W. Influence of maternal hypercholesterolaemia during pregnancy on progression of early atherosclerotic lesions in childhood: Fate of Early Lesions in Children (FELIC) study. Lancet. 1999;354(9186):1234–41.
Goldberg AC, Hopkins PN, Toth PP, Ballantyne CM, Rader DJ, Robinson JG, et al. Familial hypercholesterolemia: screening, diagnosis and management of pediatric and adult patients: clinical guidance from the National Lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipidol. 2011;5(3 Suppl):S1–8.
Russi G. Severe dyslipidemia in pregnancy: the role of therapeutic apheresis. Transfus Apher Sci. 2015;53(3):283–7.
Amundsen AL, Khoury J, Iversen PO, Bergei C, Ose L, Tonstad S, et al. Marked changes in plasma lipids and lipoproteins during pregnancy in women with familial hypercholesterolemia. Atherosclerosis. 2006;189(2):451–7.
• Smith CJ, et al. Maternal dyslipidemia and risk for preterm birth. PLoS One. 2018;13(12):e0209579 This study details the risks of maternal lipid profiles on infants.
Karalis DG, Hill AN, Clifton S, Wild RA. The risks of statin use in pregnancy: a systematic review. J Clin Lipidol. 2016;10(5):1081–90.
Jeejeebhoy FM, Zelop CM, Lipman S, Carvalho B, Joglar J, Mhyre JM, et al. Cardiac arrest in pregnancy. Circulation. 2015;132(18):1747–73.
Schutte AE, Symington EA, du Preez JL. Rosuvastatin is transferred into human breast milk: a case report. Am J Med. 2013;126(9):e7–8.
Product Information: LIPITOR(R) oral tablets, atorvastatin calcium oral tablets. Pfizer (Per FDA), New York, NY, Feb, 2012. Accessed on 14 Apr 2020.
Product Information: PRAVACHOL(R) oral tablets, pravastatin sodium oral tablets. Bristol-Myers Squibb Company (per FDA), Princeton, NJ, Jul, 2016. Accessed on 14 Apr 2020.
Product Information: LESCOL(R) oral capsules, fluvastatin sodium oral capsules. Novartis Pharmaceuticals Corporation, East Hanover, NY, Oct 1, 2006. Accessed on 14 Apr 2020.
Product Information: WELCHOL oral tablets, colesevelam hcl oral tablets. Daiichi Sankyo Inc, Parsippany, NJ, Jan 1, 2008. Accessed on 14 Apr 2020.
Product Information: Zetia(R), ezetimibe. Merck/Schering-Plough Pharmaceuticals, North Wales, PA, April, 2004. Accessed on 14 Apr 2020.
Patel G, King A, Dutta S, Korb S, Wade JR, Foulds P, et al. Evaluation of the effects of the weak CYP3A inhibitors atorvastatin and ethinyl estradiol/norgestimate on lomitapide pharmacokinetics in healthy subjects. J Clin Pharmacol. 2016;56(1):47–55.
Product Information: JUXTAPID(TM) oral capsules, lomitapide oral capsules. Aegerion Parmaceuticals (per manufacturer), Cambridge, MA, Dec, 2012. Accessed on 14 Apr 2020.
https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/211616s000lbl.pdf. Accessed 9 May 2020.
https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/202057s019lbl.pdf. Accessed 9 May 2020.
Winterfeld U, Allignol A, Panchaud A, Rothuizen LE, Merlob P, Cuppers-Maarschalkerweerd B, et al. Pregnancy outcome following maternal exposure to statins: a multicentre prospective study. Bjog. 2013;120(4):463–71.
Zarek J, Koren G. The fetal safety of statins: a systematic review and meta-analysis. J Obstet Gynaecol Can. 2014;36(6):506–9.
Bateman BT, Hernandez-Diaz S, Fischer MA, Seely EW, Ecker JL, Franklin JM, et al. Statins and congenital malformations: cohort study. Bmj. 2015;350:h1035.
Botha TC, Pilcher GJ, Wolmarans K, Blom DJ, Raal FJ. Statins and other lipid-lowering therapy and pregnancy outcomes in homozygous familial hypercholesterolaemia: a retrospective review of 39 pregnancies. Atherosclerosis. 2018;277:502–7.
Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomström-Lundqvist C, Cífková R, de Bonis M, et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;39(34):3165–241.
Pieper PG. Use of medication for cardiovascular disease during pregnancy. Nat Rev Cardiol. 2015;12(12):718–29.
Evolocumab Pregnancy Exposure Registry. https://clinicaltrials.gov/ct2/show/NCT02957604. Accessed 17 Apr 2020.
Rutherford JD. Maternal heterozygous familial hypercholesterolemia and its consequences for mother and child. Circulation. 2011;124(15):1599–601.
Watts GF, Gidding S, Wierzbicki AS, Toth PP, Alonso R, Brown WV, et al. Integrated guidance on the care of familial hypercholesterolaemia from the International FH Foundation. Int J Cardiol. 2014;171(3):309–25.
Santos RD, Gidding SS, Hegele RA, Cuchel MA, Barter PJ, Watts GF, et al. Defining severe familial hypercholesterolaemia and the implications for clinical management: a consensus statement from the International Atherosclerosis Society Severe Familial Hypercholesterolemia Panel. Lancet Diabetes Endocrinol. 2016;4(10):850–61.
Stefanutti C, et al. Toward an international consensus-integrating lipoprotein apheresis and new lipid-lowering drugs. J Clin Lipidol. 2017;11(4):858–871.e3.
Risk of fatal coronary heart disease in familial hypercholesterolaemia. Scientific Steering Committee on behalf of the Simon Broome Register Group. BMJ (Clinical research ed.), 1991. 303(6807):893–896.
France M, Rees A, Datta D, Thompson G, Capps N, Ferns G, et al. HEART UK statement on the management of homozygous familial hypercholesterolaemia in the United Kingdom. Atherosclerosis. 2016;255:128–39.
Lloyd-Jones DM, Morris PB, Ballantyne CM, Birtcher KK, Daly DD Jr, DePalma S, et al. 2017 focused update of the 2016 ACC expert consensus decision pathway on the role of non-statin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: a report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2017;70(14):1785–822.
Expert Panel on Integrated Guidelines for Cardiovascular, H, et al. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213–56.
de Ferranti SD, Steinberger J, Ameduri R, Baker A, Gooding H, Kelly AS, et al. Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association. Circulation. 2019;139(13):e603–34.
Ward NC, Watts GF, Eckel RH. Statin toxicity. Circ Res. 2019;124(2):328–50.
•• Myers KD, et al. Effect of access to prescribed PCSK9 inhibitors on cardiovascular outcomes. Circ Cardiovasc Qual Outcomes. 2019;12(8):e005404 Analysis of healthcare claims from a private dataset showed that women, minorities, and individuals of lower socioeconomic status were less likely to receive approval for PCSK9i prescriptions, which was associated with a small increase in the risk of cardiovascular events.
Ballantyne CM, Banach M, Mancini GBJ, Lepor NE, Hanselman JC, Zhao X, et al. Efficacy and safety of bempedoic acid added to ezetimibe in statin-intolerant patients with hypercholesterolemia: a randomized, placebo-controlled study. Atherosclerosis. 2018;277:195–203.
Laufs U, et al. Efficacy and safety of bempedoic acid in patients with hypercholesterolemia and statin intolerance. J Am Heart Assoc. 2019;8(7):e011662.
https://thefhfoundation.org/find-fh-specialist. Accessed on 17 Apr 2020.
Robinson JG, Williams KJ, Gidding S, Borén J, Tabas I, Fisher EA, et al. Eradicating the burden of atherosclerotic cardiovascular disease by lowering apolipoprotein B lipoproteins earlier in life. J Am Heart Assoc. 2018;7(20):e009778.
Funding
J. Knowles is funded by the National Institute of Health grants (NIH U41HG009649, NIDDK P30DK116074). F. Rodriguez was funded by a career development award from the National Heart, Lung, and Blood Institute (K01 HL 144607) and the American Heart Association/Robert Wood Johnson Harold Amos Medical Faculty Development Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Fatima Rodriguez reports personal fees from HealthPals, personal fees from Janssen, The Medicines Company and personal fees from NovoNordisk outside the submitted work. Sujana Balla, Eson P. Ekpo, Katherine Wilemon, and Joshua W. Knowles declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Women and Ischemic Heart Disease
Rights and permissions
About this article
Cite this article
Balla, S., Ekpo, E.P., Wilemon, K.A. et al. Women Living with Familial Hypercholesterolemia: Challenges and Considerations Surrounding Their Care. Curr Atheroscler Rep 22, 60 (2020). https://doi.org/10.1007/s11883-020-00881-5
Published:
DOI: https://doi.org/10.1007/s11883-020-00881-5