Abstract
Purpose of Review
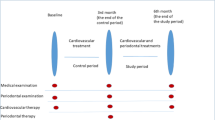
This review aims to discuss the existing evidence on the link between atherosclerosis and periodontitis by particularly presenting new findings that link the pathology and therapy of these diseases. Acute vascular ischemic events that can lead to stroke or myocardial infarction are initiated by inflammatory processes leading to rupture or erosion of plaques susceptible to thrombosis (“high risk” or “vulnerable”). These are highly inflamed plaques residing in the media and adventitia that may not be detected by angiography measurments of luminal narrowing. Statistically significant excess risk for atherosclerotic cardiovascular disease has been reported in persons with periodontitis independent of established risk factors. We hypothesized that the systemic pathologic links also represent potential therapeutic links.
Recent Findings
We recently demonstrated that periodontal inflammation promotes atherosclerotic plaque inflammation and destabilization. As discrete pathological regions, these plaques with a high susceptibility to rupture can be imaged and differentiated from lower risk plaques. In cholesterol-fed rabbits with periodontal disease, circulating inflammatory mediators were also significantly elevated thereby contributing to “vulnerable blood,” a systemic characteristic of high risk for cardiovascular events. New studies show that certain lipid mediators, including lipoxins and resolvins, are potent in preventing and possibly treating a number of inflammation-associated diseases, including periodontitis and vascular inflammation.
Summary
The concept of the vulnerable patient and the pro-resolving approach open new terrain for discovery of paradigm-changing therapies for the prevention and treatment of two of the most common diseases of man. Importantly, lipoxins and resolvins are natural receptor agonists that do not exhibit the same pro-atherogenic side effects attributed to anti-inflammatory medications (e.g., NSAIDs) but rather coordinate resolution of inflammation and a return to homeostasis.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, et al. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119(3):e21–181. https://doi.org/10.1161/CIRCULATIONAHA.108. 191261
• Hansson GK, Libby P, Tabas I. Inflammation and plaque vulnerability. J Intern Med. 2015;278(5):483–93. https://doi.org/10.1111/joim.12406. This review highlights the importance of inflammation in atherosclerotic plaque vulnerability and addresses the need for identifying the inflammatory mechanisms, high-risk conditions and novel plaque-stabilizing therapies beyond lipid lowering in order to successfully prevent rupture-prone plaques and acute coronary syndromes.
Vilahur G, Padro T, Badimon L. Atherosclerosis and thrombosis: insights from large animal models. J Biomed Biotechnol. 2011;2011:907575. https://doi.org/10.1155/2011/907575.
Shah PK. Mechanisms of plaque vulnerability and rupture. J Am Coll Cardiol. 2003;41(4 Suppl S):15S–22S.
Davies MJ. Pathology of arterial thrombosis. Br Med Bull. 1994;50(4):789–802.
Qiao Y, Farber A, Semaan E, Hamilton JA. Images in cardiovascular medicine. Healing of an asymptomatic carotid plaque ulceration. Circulation. 2008;118(10):e147–8. https://doi.org/10.1161/CIRCULATIONAHA.108.764779.
Calvert PA, Liew TV, Gorenne I, Clarke M, Costopoulos C, Obaid DR, et al. Leukocyte telomere length is associated with high-risk plaques on virtual histology intravascular ultrasound and increased proinflammatory activity. Arterioscler Thromb Vasc Biol. 2011;31(9):2157–64. https://doi.org/10.1161/ATVBAHA.111.229237.
Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364(3):226–35. https://doi.org/10.1056/NEJMoa1002358.
Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ, CDC. Periodontal Disease Surveillance workgroup: James Beck GDRP. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91(10):914–20. https://doi.org/10.1177/0022034512457373.
Dietrich T, Sharma P, Walter C, Weston P, Beck J. The epidemiological evidence behind the association between periodontitis and incident atherosclerotic cardiovascular disease. J Clin Periodontol. 2013;40(Suppl 14):S70–84. https://doi.org/10.1111/jcpe.12062.
Ryden L, Buhlin K, Ekstrand E, de Faire U, Gustafsson A, Holmer J, et al. Periodontitis increases the risk of a first myocardial infarction: a report from the PAROKRANK Study. Circulation. 2016;133(6):576–83. https://doi.org/10.1161/CIRCULATIONAHA.115.020324.
Slocum C, Kramer C, Genco CA. Immune dysregulation mediated by the oral microbiome: potential link to chronic inflammation and atherosclerosis. J Intern Med. 2016;280(1):114–28. https://doi.org/10.1111/joim.12476.
Jain A, Batista EL Jr, Serhan C, Stahl GL, Van Dyke TE. Role for periodontitis in the progression of lipid deposition in an animal model. Infect Immun. 2003;71(10):6012–8.
•• Hasturk H, Abdallah R, Kantarci A, Nguyen D, Giordano N, Hamilton J, et al. Resolvin E1 (RvE1) attenuates atherosclerotic plaque formation in diet and inflammation-induced atherogenesis. Arterioscler Thromb Vasc Biol. 2015;35(5):1123–33. https://doi.org/10.1161/ATVBAHA.115.305324. This study demostrated that uncontrolled periodontal inflammation is capable of inducing a distal inflammatory pathology in vessel walls promoting atherosclerotic plaque to rupture-prone "high-risk" plaque characterized with large necrotic areas, this fibrous cap and dense inflammatory infiltration. Further, the study revealed that resolution of local periodontal inflammation by topical application of RvE1 averts atherosclerosis. This study is the first to demonstrate that a topical treatment for periodontal disease can have profound systemic actions.
Reyes L, Herrera D, Kozarov E, Roldan S, Progulske-Fox A. Periodontal bacterial invasion and infection: contribution to atherosclerotic pathology. J Clin Periodontol. 2013;40(Suppl 14):S30–50. https://doi.org/10.1111/jcpe.12079.
de Boer SP, Cheng JM, Range H, Garcia-Garcia HM, Heo JH, Akkerhuis KM, et al. Antibodies to periodontal pathogens are associated with coronary plaque remodeling but not with vulnerability or burden. Atherosclerosis. 2014;237(1):84–91. https://doi.org/10.1016/j.atherosclerosis.2014.08.050.
Campbell LA, Rosenfeld ME. Persistent C. pneumoniae infection in atherosclerotic lesions: rethinking the clinical trials. Front Cell Infect Microbiol. 2014;4:34. https://doi.org/10.3389/fcimb.2014.00034.
Kebschull M, Demmer RT, Papapanou PN. "Gum bug, leave my heart alone!"—epidemiologic and mechanistic evidence linking periodontal infections and atherosclerosis. J Dent Res. 2010;89(9):879–902. https://doi.org/10.1177/0022034510375281.
Hajishengallis G. Periodontitis: from microbial immune subversion to systemic inflammation. Nat Rev Immunol. 2015;15(1):30–44. https://doi.org/10.1038/nri3785.
Hasturk H, Kantarci A, Goguet-Surmenian E, Blackwood A, Andry C, Serhan CN, et al. Resolvin E1 regulates inflammation at the cellular and tissue level and restores tissue homeostasis in vivo. J Immunol. 2007;179(10):7021–9.
Fredman G, Spite M. Specialized pro-resolving mediators in cardiovascular diseases. Mol Asp Med. 2017; https://doi.org/10.1016/j.mam.2017.02.003.
Norling LV, Perretti M. The role of omega-3 derived resolvins in arthritis. Curr Opin Pharmacol. 2013;13(3):476–81. https://doi.org/10.1016/j.coph.2013.02.003.
Levy BD, Serhan CN. Resolution of acute inflammation in the lung. Annu Rev Physiol. 2014;76:467–92. https://doi.org/10.1146/annurev-physiol-021113-170408.
• Bertrand MJ, Tardif JC. Inflammation and beyond: new directions and emerging drugs for treating atherosclerosis. Expert Opin Emerg Drugs. 2017;22(1):1–26. https://doi.org/10.1080/14728214.2017.1269743. This review discusses novel therapies that can address the inflammatory etiology of the atherosclerosis in the prevention of acute cardiovascular events. It highlights the urgent need in drug development aiming to target inflammatory pathways as a promising avenue for novel therapies in atherosclerosis.
Elajami TK, Colas RA, Dalli J, Chiang N, Serhan CN, Welty FK. Specialized proresolving lipid mediators in patients with coronary artery disease and their potential for clot remodeling. FASEB J. 2016;30(8):2792–801. https://doi.org/10.1096/fj.201500155R.
Serhan CN, Chiang N. Endogenous pro-resolving and anti-inflammatory lipid mediators: a new pharmacologic genus. Br J Pharmacol. 2008;153(Suppl 1):S200–15. https://doi.org/10.1038/sj.bjp.0707489.
Serhan CN. Pro-resolving lipid mediators are leads for resolution physiology. Nature. 2014;510(7503):92–101. https://doi.org/10.1038/nature13479.
Fredman G, Hellmann J, Proto JD, Kuriakose G, Colas RA, Dorweiler B, et al. An imbalance between specialized pro-resolving lipid mediators and pro-inflammatory leukotrienes promotes instability of atherosclerotic plaques. Nat Commun. 2016;7:12859. https://doi.org/10.1038/ncomms12859.
Maekawa T, Takahashi N, Tabeta K, Aoki Y, Miyashita H, Miyauchi S, et al. Chronic oral infection with Porphyromonas gingivalis accelerates atheroma formation by shifting the lipid profile. PloS one. 2011;6(5):e20240. https://doi.org/10.1371/journal.pone.0020240.
Subramanian S, Emami H, Vucic E, Singh P, Vijayakumar J, Fifer KM, et al. High-dose atorvastatin reduces periodontal inflammation: a novel pleiotropic effect of statins. J Am Coll Cardiol. 2013;62(25):2382–91. https://doi.org/10.1016/j.jacc.2013.08.1627.
Serhan CN, Jain A, Marleau S, Clish C, Kantarci A, Behbehani B, et al. Reduced inflammation and tissue damage in transgenic rabbits overexpressing 15-lipoxygenase and endogenous anti-inflammatory lipid mediators. J Immunol. 2003;171(12):6856–65.
Wu B, Mottola G, Schaller M, Upchurch GR Jr, Conte MS. Resolution of vascular injury: Specialized lipid mediators and their evolving therapeutic implications. Mol Asp Med. 2017; https://doi.org/10.1016/j.mam.2017.07.005.
•• Serhan CN. Treating inflammation and infection in the 21st century: new hints from decoding resolution mediators and mechanisms. FASEB J. 2017;31(4):1273–88. https://doi.org/10.1096/fj.201601222R. This review is an extensive overview of a series of studies over a decade that opened a new avenue in our understanding of inflammation and resolution of inflammation by specialized proresolving mediators, endogenous mediators that include the n-3-derived families resolvins, protectins, and maresins, as well as arachidonic acid-derived (n-6) lipoxins. Identified in recent years, these mediatos promote resolution of inflammation, clearance of microbes, reduction of pain, and tissue regeneration via novel mechanisms and offer a prardign shift in the treatment of inflammatory diseases.
Serhan CN, Clish CB, Brannon J, Colgan SP, Chiang N, Gronert K. Novel functional sets of lipid-derived mediators with antiinflammatory actions generated from omega-3 fatty acids via cyclooxygenase 2-nonsteroidal antiinflammatory drugs and transcellular processing. J Exp Med. 2000;192(8):1197–204.
Serhan CN, Clish CB, Brannon J, Colgan SP, Gronert K, Chiang N. Anti-microinflammatory lipid signals generated from dietary N-3 fatty acids via cyclooxygenase-2 and transcellular processing: a novel mechanism for NSAID and N-3 PUFA therapeutic actions. J Physiol Pharmacol : Off J Pol Physiol Soc. 2000;51(4 Pt 1):643–54.
Oh SF, Pillai PS, Recchiuti A, Yang R, Serhan CN. Pro-resolving actions and stereoselective biosynthesis of 18S E-series resolvins in human leukocytes and murine inflammation. J Clin Invest. 2011;121(2):569–81. https://doi.org/10.1172/JCI42545.
Serhan CN, Hong S, Gronert K, Colgan SP, Devchand PR, Mirick G, et al. Resolvins: a family of bioactive products of omega-3 fatty acid transformation circuits initiated by aspirin treatment that counter proinflammation signals. J Exp Med. 2002;196(8):1025–37.
Arita M, Bianchini F, Aliberti J, Sher A, Chiang N, Hong S, et al. Stereochemical assignment, antiinflammatory properties, and receptor for the omega-3 lipid mediator resolvin E1. J Exp Med. 2005;201(5):713–22. https://doi.org/10.1084/jem.20042031.
Oh SF, Dona M, Fredman G, Krishnamoorthy S, Irimia D, Serhan CN. Resolvin E2 formation and impact in inflammation resolution. J Immunol. 2012;188(9):4527–34. https://doi.org/10.4049/jimmunol.1103652.
Tjonahen E, Oh SF, Siegelman J, Elangovan S, Percarpio KB, Hong S, et al. Resolvin E2: identification and anti-inflammatory actions: pivotal role of human 5-lipoxygenase in resolvin E series biosynthesis. Chem Biol. 2006;13(11):1193–202. https://doi.org/10.1016/j.chembiol.2006.09.011.
Arita M, Ohira T, Sun YP, Elangovan S, Chiang N, Serhan CN. Resolvin E1 selectively interacts with leukotriene B4 receptor BLT1 and ChemR23 to regulate inflammation. J Immunol. 2007;178(6):3912–7.
Schwab JM, Chiang N, Arita M, Serhan CN. Resolvin E1 and protectin D1 activate inflammation-resolution programmes. Nature. 2007;447(7146):869–74. https://doi.org/10.1038/nature05877.
Spite M, Claria J, Serhan CN. Resolvins, specialized proresolving lipid mediators, and their potential roles in metabolic diseases. Cell metabolism. 2014;19(1):21–36. https://doi.org/10.1016/j.cmet.2013.10.006.
El Kebir D, Gjorstrup P, Filep JG. Resolvin E1 promotes phagocytosis-induced neutrophil apoptosis and accelerates resolution of pulmonary inflammation. Proc Natl Acad Sci U S A. 2012;109(37):14983–8. https://doi.org/10.1073/pnas.1206641109.
Ohira T, Arita M, Omori K, Recchiuti A, Van Dyke TE, Serhan CN. Resolvin E1 receptor activation signals phosphorylation and phagocytosis. J Biol Chem. 2010;285(5):3451–61. https://doi.org/10.1074/jbc.M109.044131.
Haworth O, Cernadas M, Yang R, Serhan CN, Levy BD. Resolvin E1 regulates interleukin 23, interferon-gamma and lipoxin A4 to promote the resolution of allergic airway inflammation. Nat Immunol. 2008;9(8):873–9. https://doi.org/10.1038/ni.1627.
Hasturk H, Kantarci A, Ohira T, Arita M, Ebrahimi N, Chiang N, et al. RvE1 protects from local inflammation and osteoclast- mediated bone destruction in periodontitis. FASEB J. 2006;20(2):401–3. https://doi.org/10.1096/fj.05-4724fje.
Campbell EL, MacManus CF, Kominsky DJ, Keely S, Glover LE, Bowers BE, et al. Resolvin E1-induced intestinal alkaline phosphatase promotes resolution of inflammation through LPS detoxification. Proc Natl Acad Sci U S A. 2010;107(32):14298–303. https://doi.org/10.1073/pnas.0914730107.
Rajasagi NK, Reddy PB, Suryawanshi A, Mulik S, Gjorstrup P, Rouse BT. Controlling Herpes simplex virus-induced ocular inflammatory lesions with the lipid-derived mediator resolvin E1. J Immunol. 2011;186(3):1735–46. https://doi.org/10.4049/jimmunol.1003456.
Li N, He J, Schwartz CE, Gjorstrup P, Bazan HE. Resolvin E1 improves tear production and decreases inflammation in a dry eye mouse model. J Ocul Pharmacol Ther : Off J Assoc Ocul Pharmacol Ther. 2010;26(5):431–9. https://doi.org/10.1089/jop.2010.0019.
Serhan CN, Savill J. Resolution of inflammation: the beginning programs the end. Nature immunology. 2005;6(12):1191–7. https://doi.org/10.1038/ni1276.
Qu X, Zhang X, Yao J, Song J, Nikolic-Paterson DJ, Li J. Resolvins E1 and D1 inhibit interstitial fibrosis in the obstructed kidney via inhibition of local fibroblast proliferation. J Pathol. 2012;228(4):506–19. https://doi.org/10.1002/path.4050.
Keyes KT, Ye Y, Lin Y, Zhang C, Perez-Polo JR, Gjorstrup P, et al. Resolvin E1 protects the rat heart against reperfusion injury. Am J Physiol Heart Circ Physiol. 2010;299(1):H153–64. https://doi.org/10.1152/ajpheart.01057.2009.
Levy BD, Zhang QY, Bonnans C, Primo V, Reilly JJ, Perkins DL, et al. The endogenous pro-resolving mediators lipoxin A4 and resolvin E1 preserve organ function in allograft rejection. Prostaglandins Leukot Essent Fat Acids. 2011;84(1–2):43–50. https://doi.org/10.1016/j.plefa.2010.09.002.
Dalli J, Serhan CN. Specific lipid mediator signatures of human phagocytes: microparticles stimulate macrophage efferocytosis and pro-resolving mediators. Blood. 2012;120(15):e60–72. https://doi.org/10.1182/blood-2012-04-423525.
Endo J, Sano M, Isobe Y, Fukuda K, Kang JX, Arai H, et al. 18-HEPE, an n-3 fatty acid metabolite released by macrophages, prevents pressure overload-induced maladaptive cardiac remodeling. J Exp Med. 2014;211(8):1673–87. https://doi.org/10.1084/jem.20132011.
Chiang N, Fredman G, Backhed F, Oh SF, Vickery T, Schmidt BA, et al. Infection regulates pro-resolving mediators that lower antibiotic requirements. Nature. 2012;484(7395):524–8. https://doi.org/10.1038/nature11042.
Ishida T, Yoshida M, Arita M, Nishitani Y, Nishiumi S, Masuda A, et al. Resolvin E1, an endogenous lipid mediator derived from eicosapentaenoic acid, prevents dextran sulfate sodium-induced colitis. Inflamm Bowel Dis. 2010;16(1):87–95. https://doi.org/10.1002/ibd.21029.
Abela OG, Ahsan CH, Alreefi F, Salehi N, Baig I, Janoudi A, et al. Plaque rupture and thrombosis: the value of the atherosclerotic rabbit model in defining the mechanism. Curr Atheroscler Rep. 2016;18(6):29. https://doi.org/10.1007/s11883-016-0587-0.
Bodary PF, Eitzman DT. Animal models of thrombosis. Curr Opin Hematol. 2009;16(5):342–6. https://doi.org/10.1097/MOH.0b013e32832e9ddd.
Constantinides P, Chakravarti RN. Rabbit arterial thrombosis production by systemic procedures. Arch Pathol. 1961;72:197–208.
Baumgartner HRSA. Folgen des gefa¨sskatheterismus am normo- und hypercholesterinaemischen kaninchen. Path Microbiol. 1966;29:393–405.
Abela GS, Picon PD, Friedl SE, Gebara OC, Miyamoto A, Federman M, et al. Triggering Of plaque disruption and arterial thrombosis in an atherosclerotic rabbit model. Circulation. 1995;91(3):776–84.
Phinikaridou A, Hallock KJ, Qiao Y, Hamilton JA. A robust rabbit model of human atherosclerosis and atherothrombosis. J Lipid Res. 2009;50(5):787–97.
Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL, et al. ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. Circulation. 2011;124(4):489–532. https://doi.org/10.1161/CIR.0b013e31820d8d78.
Crignon C. The discovery of blood circulation: revolution or revision? Gesnerus. 2011;68(1):5–25.
Kalani MY, Martirosyan NL, Eschbacher JM, Nakaji P, Albuquerque FC, Spetzler RF. Large hemangiopericytoma associated with arteriovenous malformations and dural arteriovenous fistulae. World Neurosurg. 2011;76(6):592 e7–10. https://doi.org/10.1016/j.wneu.2011.05.023.
Kaltman JR, Thompson PD, Lantos J, Berul CI, Botkin J, Cohen JT, et al. Screening for sudden cardiac death in the young: report from a national heart, lung, and blood institute working group. Circulation. 2011;123(17):1911–8. https://doi.org/10.1161/CIRCULATIONAHA.110.017228.
Polkinghorne BG, Muscatello DJ, Macintyre CR, Lawrence GL, Middleton PM, Torvaldsen S. Relationship between the population incidence of febrile convulsions in young children in Sydney, Australia and seasonal epidemics of influenza and respiratory syncytial virus, 2003–2010: a time series analysis. BMC Infect Dis. 2011;11:291. https://doi.org/10.1186/1471-2334-11-291.
Hua N, Baik F, Pham T, Phinikaridou A, Giordano N, Friedman B, et al. Identification of high-risk plaques by MRI and fluorescence imaging in a rabbit model of atherothrombosis. PloS one. 2015;10(10):e0139833. https://doi.org/10.1371/journal.pone.0139833.
Stein-Merlob AF, Hara T, McCarthy JR, Mauskapf A, Hamilton JA, Ntziachristos V et al. Atheroma susceptible to thrombosis exhibit impaired endothelial permeability in vivo as assessed by nanoparticle-based fluorescence molecular imaging. Circ Cardiovasc Imaging. 2017;10(5). doi:https://doi.org/10.1161/CIRCIMAGING.116.005813.
Calcagno C, Fayad ZA. Intraplaque and cellular distribution of dextran-coated iron oxide fluorescently labeled nanoparticles: insights into atherothrombosis and plaque rupture. Circ Cardiovasc Imaging. 2017;10(5). doi:https://doi.org/10.1161/CIRCIMAGING.117.006533.
Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006;47(8_Suppl_C):C13–8. https://doi.org/10.1016/j.jacc.2005.10.065.
Hao H, Gabbiani G, Camenzind E, Bacchetta M, Virmani R, Bochaton-Piallat ML. Phenotypic modulation of intima and media smooth muscle cells in fatal cases of coronary artery lesion. Arterioscler Thromb Vasc Biol. 2006;26(2):326–32. https://doi.org/10.1161/01.ATV.0000199393.74656.4c.
Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part I. Circulation. 2003;108(14):1664–72. https://doi.org/10.1161/01.CIR.0000087480.94275.97.
Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part II. Circulation. 2003;108(15):1772–8. https://doi.org/10.1161/01.CIR.0000087481.55887.C9.
Myerburg RJ, Interian A Jr, Mitrani RM, Kessler KM, Castellanos A. Frequency of sudden cardiac death and profiles of risk. Am J Cardiol. 1997;80(5B):10F–9F.
de Gaetano M, Crean D, Barry M, Belton O. M1- and M2-type macrophage responses are predictive of adverse outcomes in human atherosclerosis. Front Immunol. 2016;7:275. https://doi.org/10.3389/fimmu.2016.00275.
Pasceri V, Willerson JT, Yeh ET. Direct proinflammatory effect of C-reactive protein on human endothelial cells. Circulation. 2000;102(18):2165–8.
Verma S, Li SH, Badiwala MV, Weisel RD, Fedak PW, Li RK, et al. Endothelin antagonism and interleukin-6 inhibition attenuate the proatherogenic effects of C-reactive protein. Circulation. 2002;105(16):1890–6.
Kiechl S, Egger G, Mayr M, Wiedermann CJ, Bonora E, Oberhollenzer F, et al. Chronic infections and the risk of carotid atherosclerosis: prospective results from a large population study. Circulation. 2001;103(8):1064–70.
Cimmino G, Loffredo FS, Morello A, S DE, De Palma R, Cirillo P et al. Immune-inflammatory activation in acute coronary syndromes: a look into the heart of unstable coronary plaque. Curr Cardiol Rev. 2016. https://doi.org/10.2174/1573403X12666161014093812.
Lindy O, Suomalainen K, Makela M, Lindy S. Statin use is associated with fewer periodontal lesions: a retrospective study. BMC Oral Health. 2008;8:16. https://doi.org/10.1186/1472-6831-8-16.
Hayashi C, Viereck J, Hua N, Phinikaridou A, Madrigal AG, Gibson FC 3rd, et al. Porphyromonas gingivalis accelerates inflammatory atherosclerosis in the innominate artery of ApoE deficient mice. Atherosclerosis. 2011;215(1):52–9. https://doi.org/10.1016/j.atherosclerosis. 2010.12. 009.
Zaromytidou M, Antoniadis AP, Siasos G, Coskun AU, Andreou I, Papafaklis MI, et al. Heterogeneity of coronary plaque morphology and natural history: current understanding and clinical significance. Curr Atheroscler Rep. 2016;18(12):80. https://doi.org/10.1007/s11883-016-0626-x.
Westrick R, Fredman G, Early CC. Platelets: context-dependent vascular protectors or mediators of disease. Arterioscler Thromb Vasc Biol. 2015;35(7):e25–9. https://doi.org/10.1161/ATVBAHA.115.305898.
Daugherty A, Tall AR, Daemen M, Falk E, Fisher EA, Garcia-Cardena G, et al. Recommendation on design, execution, and reporting of animal atherosclerosis studies: a scientific statement From the American Heart Association. Arterioscler Thromb Vasc Biol. 2017;37(9):e131–e57. https://doi.org/10.1161/ATV.0000000000000062.
Granada JF, Kaluza GL, Wilensky RL, Biedermann BC, Schwartz RS, Falk E. Porcine models of coronary atherosclerosis and vulnerable plaque for imaging and interventional research. EuroIntervention: J EuroPCR Collab Work Group Interventional Cardiol Eur Soc Cardiol. 2009;5(1):140–8.
Phinikaridou A, Ruberg FL, Hallock KJ, Qiao Y, Hua N, Viereck J, et al. In vivo detection of vulnerable atherosclerotic plaque by MRI in a rabbit model. Circ Cardiovasc Imaging. 2010;3(3):323–32. https://doi.org/10.1161/CIRCIMAGING.109.918524.
Tabas I. Macrophage death and defective inflammation resolution in atherosclerosis. Nat Rev Immunol. 2010;10(1):36–46. https://doi.org/10.1038/nri2675.
Acknowledgements
We thank Grace Yee for help in preparing the manuscript. The authors also thank Daniel Nguyen, Olivia Nguyen, and Konstantinia Almpani for their assistance in periodontitis and the CVD model in rabbits and histopathology. The preliminary studies were supported by the Forsyth Institute Pilot Grant Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
James A. Hamilton, Hatice Hasturk, Alpdogan Kantarci, Charles Serhan, and Thomas Van Dyke declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Vascular Biology
Rights and permissions
About this article
Cite this article
Hamilton, J.A., Hasturk, H., Kantarci, A. et al. Atherosclerosis, Periodontal Disease, and Treatment with Resolvins. Curr Atheroscler Rep 19, 57 (2017). https://doi.org/10.1007/s11883-017-0696-4
Published:
DOI: https://doi.org/10.1007/s11883-017-0696-4