Abstract
MicroRNAs (miRs) are short non-coding RNA molecules involved in post-transcriptional gene regulation by binding to the 3′ untranslated region of a messenger RNA (mRNA), thereby inhibiting the translation or inducing mRNA destabilization. MiRs are generally considered to act as intracellular mediators essential for normal cardiac function, and their deregulated expression profiles have been associated with cardiovascular diseases. Recent studies have revealed the existence of freely circulating miRs in human peripheral blood, which are present in a stable nature. This has raised the possibility that miRs may be released in the circulation and can serve as novel diagnostic markers for acute or chronic human disorders, including myocardial infarction (MI). This review summarizes the recent findings of miRs that fulfill the criteria of candidate biomarkers for MI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myocardial infarction (MI) is a major cause of mortality and morbidity in Western hemisphere. Annually, around 15 million patients in the United States and Europe are presented to the emergency department with chest pain or other symptoms indicative of MI [1, 2]. Early diagnosis and treatment of patients with acute MI could prevent or reduce ischemic damage to the myocardium and, therefore, could prevent subsequent cardiac remodeling and failure.
MI reflects cardiomyocyte death (necrosis) as a consequence of prolonged ischemia [3], which results from acute thrombotic occlusion of a coronary artery. Myocardial cell death can be detected by release of multiple proteins from the damaged cells into the circulation [4]. Cardiac troponin (Tn) I and T are structural proteins predominantly expressed in the heart, and are currently considered as the “gold standard” for acute MI (AMI) [4]. Their detection in peripheral blood indicates cardiomyocyte necrosis, and in combination with 12-lead electrocardiogram (ECG) and creatine kinase isoenzyme MB (CK-MB) they form the diagnostic cornerstones for MI [2, 5, 6]. However, although elevated biomarkers in the blood indicate myocardial damage, they do not diagnose the underlying mechanisms. For example, elevated values of the biomarkers in the absence of clinical evidence of ischemia could also occur as a consequence of other causes of cardiac injury, such as myocarditis, sepsis, cardioversion, or ablation [7–10]. Cardiac troponins are superior to all other biomarkers that have been clinically available in the diagnosis of MI [11–14] and they directly correlate with the size of MI [15, 16]. A major drawback of the contemporary Tn assays is their inadequate sensitivity during the first few hours after the onset of MI, as they are released slowly from damaged cardiomyocytes and do not peak until 6 to 12 h after the onset of symptoms [17]. Therefore, sampling is needed every 6 h. However, high-sensitive Tn assays are already on the market, and recent multicenter studies [18•, 19•] have shown that these assays improved the early diagnosis of MI, even if patients are presented within 3 h after the onset of chest pain. These assays contributed to safely “rule out” or “rule in” coronary causes of acute chest pain.
microRNAs (miRs) are evolutionary conserved, short, non-coding (~ 22 nucleotides) RNA molecules involved in post-transcriptional gene regulation [20–22]. Their binding potency to the 3′ untranslated region (UTR) of messenger RNAs (mRNAs) determines their mode of action: translational inhibition and/or augmented mRNA degradation, both pathways resulting in endogenous gene silencing. Around 1500 human miRs (http://www.mirbase.org/ v 18.0) have been cloned and sequenced and it is estimated that they regulate up to 50% of the protein-coding genes [23–25].
MiRs are generally considered to act as intracellular mediators essential for normal cardiac function [26] and their deregulated expression profiles have been associated with cardiovascular diseases [26–29]. Recent studies have revealed existence of freely circulating miRs in human peripheral blood that are stably expressed [30–32]. This has raised the possibility that microRNAs may be probed in the circulation and can serve as novel diagnostic markers for cardiovascular diseases. An important characteristic of miRs is their tissue and cell specificity [33] providing unique signature with diagnostic opportunities for diverse diseases [34]. In line with this, several studies have demonstrated circulating miRs reflecting pathologic condition, such as cancer and liver injury indicating that miRs could be used as sensitive and specific biomarkers of various pathologies and tissue injuries [35, 36]. In addition, another advantage is the relative ease with which miRs can be measured: polymerase chain reaction (PCR) allows being more sensitive and specific than classic antibody-based assays. A major improvement comes within reach to measure dozens of circulating miRs at once. This could become feasible against reasonable costs, comparable to the costs of measurement of only two or three protein markers. This induces a completely novel way of designing and using biomarkers in heart disease: instead of seeking one or two gold standard diagnostics, a more complete profile can be routinely measured to allow sensitive characterization of subtypes of disease. It is already known for classical biomarkers that adding a novel marker to the existing ones adds information and increases diagnostic power but also sharply increases the associated costs. Designing oligonucleotides for miRs and performing subsequent quantitative reverse transcriptase (qRT)-PCRs are much less time- and cost-consuming processes when compared to the development and production of new and specific antibodies and enzyme-linked immunosorbent assays (ELISAs). Therefore, circulating miRs as biomarkers for MI could increase the number of markers measured and continue to increase diagnostic power without increasing costs to a larger extent.
Ideal blood biomarkers of MI should comprehend the following characteristics: they should be 1) abundant and preferably exclusively expressed in the tissue of interest, 2) expressed at low levels in the blood under normal/healthy circumstances, 3) released into the circulation after tissue injury, 4) stable in the circulation, and 5) easily detected with high sensitivity and specificity. Here we will review the recent findings of circulating miRs that fulfill the mentioned criteria and discuss their potential to be used as biomarkers for MI (Table 1).
miR-1 and miR-133
miR-1-1/miR-133a-2 and miR-1-2/miR-133a-1 are two bi-cistronic miR clusters expressed in both skeletal and cardiac muscle. The sequence of mature miR-1-1 and miR-1-2 is identical and the same holds true for miR-133a-1 and miR-133-2. MiR-133b differs from miR-133a in the 2 nucleotides at the 3′ terminus and is specifically expressed in skeletal muscle.
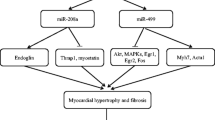
miR-1 is the most abundantly expressed miR in the heart. Both miR-1 and miR-133 are anti-hypertrophic miRs, involved in regulation of signaling cascades and sarcomeric organization [37]. Six hours after coronary artery occlusion in mice, miR-1 and miR-133 levels were decreased in infarcted and border zone area of the heart whereas their levels were increased in the peripheral blood [38], indicating release of these miRs into the circulation after tissue injury. Also, in AMI patients, significantly higher circulating levels of miR-1 and miR-133 levels could be detected in the circulation [38••, 39••, 40••, 41••, 42••, 43••, 44••] as soon as 5 h after the onset of symptoms [40••]. In addition, when plasma samples were obtained 156 min after the onset of symptoms, miR-1 and miR-133 levels had a significantly higher peak than TnI, indicating their early release after MI [38]. However, one study showed no significant differences in miR-1 expression between AMI and controls [44••], which could be explained by possible renal elimination of miR-1 [39••] or by conceivable presence of higher skeletal muscle turnover in the control patients [40••]. In addition, enhanced miR-1 and miR-133 levels in the circulation were detected after sham operated hearts [40••], demonstrating that damaged muscle could also contribute to induced levels of mR-1 and miR-133 in the circulation.
Both miR-1 and miR-133 levels augment in the circulation of the ST-elevated MI (STEMI) patients compared to the healthy controls within the first 12 h after the onset of the symptoms, followed by a return to adjacent baseline levels after 12 to 24 h [39••]. In contrast, one study demonstrated significantly high levels of miR-133 in the plasma after 20 h of the onset of the symptoms [35], although not precisely describing which miR-133 isoform was studied. In 8 of 25 STEMI patients, miR-1 and miR-133a could be detected in the urine within 24 h after the onset of symptoms indicating renal elimination. This is in line with another study showing a correlation between miR-1 and miR-133a and estimated glomerular filtration rate (eGFR) in STEMI patients but not between miR-133b and eGFR [43••]. Furthermore, both miR-1 and miR-133 correlated with TnT [43••] implying myocardial damage. Moreover, miR-1 also positively correlates with creatine kinase-MB [42••] and QRS widening in AMI patients [41], with infarct size in an animal model of MI and with cell damage in vitro [42••].
Receiver operator characteristics (ROC) curves for miR-1 demonstrate area under the curve (AUC) varying from 0.77 [41••] to 0.98 [39••, 40••] indicating fair to excellent accuracy of this miR for the use of a biomarker in MI. For miR-133, the ROC analysis reveal AUC values between 0.86 and 0.89 indicating good sensitivity and specificity distinguishing between STEMI patients and healthy controls [39••, 40••]. Together with their high expression in the heart, and increased levels in the blood after the MI, miR-1 and miR-133 could be suitable candidates as biomarkers for the MI. However, other injuries to the skeletal muscle should be preferably excluded to rule out the non-specific effects. In addition, the oscillations of these miRs after MI should be studied accurately to reveal their exact times of increase and decrease in the circulation and to study to which extent they could contribute to the already existing biomarkers. Finally, larger study populations are essential to make correct conclusions if miR-1 and miR-133 could be used as biomarkers in MI.
miR-499 and miR-208
miR-499 is an evolutionary conserved muscle-specific miR that is located in an intronic region of the MYH7B gene and plays a role in myosin gene regulation [45, 46]. Although miR-499 is highly expressed under normal conditions in the heart [45, 47], its expression decreases in the ischemic heart [48], suggesting its release from the damaged tissue. Indeed, miR-499 levels could be detected in plasma of AMI patients [38••, 39••, 40••, 44••, 49], whereas one study did not detect differences in miR-499 expression between STEMI, non–ST-elevated MI (NSTEMI), and patients with unstable angina [43••]. Although miR-1 and miR-133a peaked around 156 min after the onset of MI symptoms, miR-499 is at its highest point around 12 h [38••, 39••], suggesting possible slower kinetics compared to miR-1 and miR-133. However, similar to miR-1 and miR-133, miR-499 levels increase in the circulation in the sham operated hearts, indicating that damaged muscle contributes to enhanced circulating miR-499 levels.
Besides parallel expression of miR-499 and TnI in an animal model of MI [38••], miR-499 correlates with TnT [44••] and CK-MB [49] in AMI patients. ROC analysis demonstrates AUC values varying between 0.82 and 0.99, indicating good to excellent sensitivity and specificity [39••, 40••, 44••].
Other miRs encoded by the myosin genes are miR-208a and miR-208b, which are located in MYH6 and MYH7 genes, respectively. MiR-208a and miR-208b are abundantly and exclusively expressed in the heart, making them most suitable candidates to be used as biomarkers for the MI. Indeed, miR-208a [40••] and miR-208b [39••, 43••, 44••] levels are increased in the circulation after the MI. Two studies showed that miR-208b was the most abundantly elevated miR in the plasma, with 1600 [44••] and 3000 [39••] times more expression in the AMI patients than in the controls. Furthermore, miR-208b levels correlated with TnT levels reflecting myocardial damage [39••, 43••, 44••]. Moreover, the amount of miR-208b in blood inversely correlates with left ventricular ejection fraction, raising the possibility in using this miR not only for diagnostic purposes but also for potential prognostic use in long-term cardiac function and probability of developing heart failure. Nevertheless, one larger population study of 444 subjects revealed that although circulating levels of miR-208b were associated with all-cause mortality at 6 months, after adjustment for TnT levels, its association was lost with the outcome. This implies that miR-208b does not add prognostic information to an already sensitive necrosis marker. However, it should be taken into account that this does not exclude the potential of miR-208b to augment its prognostic value when measuring at an earlier or later time point.
Only one study detected significantly higher circulating miR-208a levels in the AMI patients [40••] in contrast to the others [38••, 39••, 49]. This could have several explanations. The first is related to the time point of sampling and could explain why miR-208a was not detected in the circulation [49]. In this study, blood sampling occurred within 48 h after the onset of symptoms [49], although miR-208a peaks around 3 h after the AMI [38••, 40••] and is restored to the baseline after 24 h [40••]. The second explanation is related to the myosin isoform expression between a mouse and a human heart. miR-208a is abundantly and exclusively expressed in the adult mouse heart, whereas miR-208b is more expressed during development and in response to stress. However, MYH7, harboring miR-208b, is the primary isoform in the human cardiac muscle [50, 51], providing an explanation why miR-208b is abundantly present in the human heart. This could explain why two studies could not detect miR-208a in the circulation, although sampling the blood within the appropriate time line [38••, 39••].
Specificity and sensitivity analysis for miR-208b reveal AUCs between 0.94 and 1.00, indicating excellent accuracy for discrimination between AMI patients and the controls [39••, 44••]. In combination with its exclusive expression in the heart, and high increase in blood after the MI, miR-208b could be a suitable candidate as a biomarker for the MI. Nevertheless, the kinetics of miR-208a should be studied extensively and in bigger populations to reveal its exact incline and decline after the MI and to decide what its contribution could be to the already existing biomarkers such as hs-TnT and TnI.
Non-specific Cardiac and Skeletal Muscle miRs
In theory, candidate biomarkers for MI should display cardiac specific expression patterns. Recently, one study revealed miR-663b and miR-1291 as the most predictive miRs for the MI with 92.5% and 85% accuracy, respectively [52•]. In addition, miR-30c and smooth muscle cell-enriched miR-145 were significantly increased in these STEMI patients and correlated with hs-TnT, indicting their potency to reflect cell death. Moreover, the same study reported an miRs signature, which could serve as a new class of biomarkers [52•]. This signature represents a combination of 20 most up- and down-regulated miRs in 20 STEMI patients in contrast to the controls and could enhance diagnostic discrimination of STEMI patients from the control with 96% specificity, 90% sensitivity, and the AUC of 0.99, indicating excellent accuracy. These results are promising, but because these miRs are not cardiac specific, other pathologic processes could underlie the effects seen in this study. Furthermore, the patient population is too small to drawn correct conclusions about this particular miRs signature and because these miRs are isolated from the whole peripheral blood, circulating cells could also contribute to the miRs expression levels. Nevertheless, such a multi-marker approach could be of interest to increase diagnostic power and to gain more information about the time line of MI, which in turn could lead to faster and accurate treatments and prevent subsequent cardiac remodeling and failure.
Stability of Circulating miRs
Extracellular miRs have been found recently in multiple human body fluids, such as blood plasma, urine, and saliva [30, 53, 54]. MiRs are surprisingly stable in the plasma regardless of high RNAase activity [30], contributing to the possibility that that miRs could be used as new class of blood-based biomarkers. Several mechanisms influencing the miR stability in the circulation are discussed below.
Circulating miRs can be carried in different types of vesicles, such as exosomes [55•] and microvesicles [56•]. Exosomes are small (50–90 nm) vesicles that are released into the extracellular environment by fusion of the multivesicular bodies and the plasma membrane. Production of exosomes occurs through the inward budding of the endosomes. One study showed that 121 miRs are associated with exosomes and that several miRs were abundantly expressed in exosomes compared to the cells, suggesting packing regulation [55•]. These miRs are not localized on the external structures or macromolecules, but instead are restricted to the inner part [55•]. Besides exosomes, microvesicles can also contain miRs [56•]. These particles are larger (up to 1um) and shed from the cell membrane. In addition, microvesicles are enriched in bio-active molecules and contain nucleic acids and/or proteins [57]. MiRs located in exosomes or microvesicles are extremely resistant to RNAase-dependent degradation with necessity to first destroy the lipid bilayer of the vesicles before miRs can become accessible for RNAase degradation [55•].
Previous studies have shown that nucleic acids can bind and form stable complexes with specific lipids found on lipoproteins [58–60] by divalent cation bridging [61]. High-density lipoproteins (HDL) are used as carrier to deliver lipophilic anti-tumor drug to human hepatocellular carcinoma cells in vitro [62]. In animal models, liposomes containing apolipoprotein A-I, which is the main protein component of HDL, have been used to the delivery of several siRNAs to the liver [63]. Recently, one study revealed that HDL (8–12 nm) isolated from patients with hypercholesterolemia contained small RNAs including miRs [64•]. The exact mechanism of how miRs are loaded into the HDL particles and how they are protected from the external RNAases has to be elucidated.
miRs can also be stabilized in the circulation when localized in the apoptotic bodies. One study demonstrated that endothelial cell-derived apoptotic bodies, which are produced during atherosclerosis, carry miR-126 as well as other miRs [65]. The majority of extracellular miRs in blood plasma are bound to protein complexes protecting these miRs from degradation. In line with this, one study has shown that a RNA binding protein, nucleophosmin 1 (NPM1), and nucleolin were highly abundant in the fibroblast medium after serum deprivation and that especially NPM1 could bind and protect miR-122 against degradation [66]. However, it needs to be investigated if NPM1 is present and operative in binding and protecting miRs in the human circulation.
Very recently, two studies have demonstrated that vesicle-encapsuled miRs represent only a minor fragment of circulating miRs and that over 90% of circulating miRs are exosome free and bound to Argonaute proteins [67•, 68]. These proteins are naturally occurring within the cell and are a part of RNA-induced silencing complex. Argonaute 2 (Ago2) plays an especially important role in stabilizing miRs in the plasma as Ago2/miRs complexes are extremely nuclease and protease resistant.
In conclusion, several mechanisms are described for miRs export and their subsequent stabilization in the circulation. Export of most miRs is energy dependent and active transport, suggesting complex regulation of this process [66]. However, miR release after an AMI would reflect a rather passive form due to necrosis. Mature miRs in the cells that are Ago2 bound and necessary for the stabilization are localized in the cytoplasm or in the P-bodies, suggesting that extracellular miRs detected in the plasma after an AMI would represent Ago2-bound miRs.
Conclusions
Myocardial-derived miRs, such as miR-1, miR-133, miR-499, and miR-208, might be useful as potential biomarkers for MI. These miRs are abundantly expressed in the heart but less so in the circulation under normal/healthy circumstances. In addition, they are released into the circulation after the MI, where they are in a stable conformation and can be detected with high accuracy. Larger study populations and exact time points of blood sampling are required to study the kinetics of these myocardial-derived miRs in AMI patients and to investigate their potential to be used as new biomarkers in MI. It is already known for classical biomarkers that adding a novel marker to the existing ones adds information and increases diagnostic power but also sharply increases the associated costs. Designing primers for miRs and performing subsequent qRT-PCRs are much less time- and cost-consuming processes when compared to the development and production of new and specific antibodies and ELISAs. In this way, a multi-miRs marker approach also becomes attractive, which could lead to increased diagnostic power and provide more information about the time line of MI, with the faster and accurate treatments with the subsequent improvement of the clinical outcome. To promote the use of miRs as biomarkers, it is essential to develop new techniques that can provide quick detection of miRs in the circulation.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Adv Data. 2007;29(386):1–32.
Bassand JP, Hamm CW, Ardissino D, Boersma E, Budaj A, Fernandez-Aviles F, et al. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J. 2007;28(13):1598–660.
Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J. 2000 Sep; 21(18): 1502–13.
Jaffe AS, Ravkilde J, Roberts R, Naslund U, Apple FS, Galvani M, et al. It’s time for a change to a troponin standard. Circulation. 2000;102(11):1216–20.
Thygesen K, Alpert JS, White HD, Jaffe AS, Apple FS, Galvani M, et al. Universal definition of myocardial infarction. Circulation. 2007;116(22):2634–53.
Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey Jr DE, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007;116(7):e148–304.
Lauer B, Niederau C, Kuhl U, Schannwell M, Pauschinger M, Strauer BE, et al. Cardiac troponin T in patients with clinically suspected myocarditis. J Am Coll Cardiol. 1997;30(5):1354–9.
Spies C, Haude V, Fitzner R, Schroder K, Overbeck M, Runkel N, et al. Serum cardiac troponin T as a prognostic marker in early sepsis. Chest. 1998;113(4):1055–63.
Allan JJ, Feld RD, Russell AA, Ladenson JH, Rogers MA, Kerber RE, et al. Cardiac troponin I levels are normal or minimally elevated after transthoracic cardioversion. J Am Coll Cardiol. 1997;30(4):1052–6.
Katritsis DG, Hossein-Nia M, Anastasakis A, Poloniecki J, Holt DW, Camm AJ, et al. Myocardial injury induced by radiofrequency and low energy ablation: a quantitative study of CK isoforms, CK-MB, and troponin-T concentrations. Pacing Clin Electrophysiol. 1998;21(7):1410–6.
Thygesen K, Mair J, Katus H, Plebani M, Venge P, Collinson P, et al. Recommendations for the use of cardiac troponin measurement in acute cardiac care. Eur Heart J. Sep; 31(18): 2197-204.
Morrow DA, Antman EM, Tanasijevic M, Rifai N, de Lemos JA, McCabe CH, et al. Cardiac troponin I for stratification of early outcomes and the efficacy of enoxaparin in unstable angina: a TIMI-11B substudy. J Am Coll Cardiol. 2000;36(6):1812–7.
Hochholzer W, Buettner HJ, Trenk D, Laule K, Christ M, Neumann FJ, et al. New definition of myocardial infarction: impact on long-term mortality. Am J Med. 2008;121(5):399–405.
Eggers KM, Oldgren J, Nordenskjold A, Lindahl B. Diagnostic value of serial measurement of cardiac markers in patients with chest pain: limited value of adding myoglobin to troponin I for exclusion of myocardial infarction. Am Heart J. 2004;148(4):574–81.
Kurz K, Schild C, Isfort P, Katus HA, Giannitsis E. Serial and single time-point measurements of cardiac troponin T for prediction of clinical outcomes in patients with acute ST-segment elevation myocardial infarction. Clin Res Cardiol. 2009;98(2):94–100.
Tzivoni D, Koukoui D, Guetta V, Novack L, Cowing G. Comparison of Troponin T to creatine kinase and to radionuclide cardiac imaging infarct size in patients with ST-elevation myocardial infarction undergoing primary angioplasty. Am J Cardiol. 2008;101(6):753–7.
Panteghini M, Pagani F, Bonetti G. The sensitivity of cardiac markers: an evidence-based approach. Clin Chem Lab Med. 1999;37(11-12):1097–106.
• Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361(9):858–67. This work demonstrates that high-sensitive TnI can improve early diagnosis of AMI in 718 constitutive patients.
• Keller T, Zeller T, Peetz D, Tzikas S, Roth A, Czyz E, et al. Sensitive troponin I assay in early diagnosis of acute myocardial infarction. N Engl J Med. 2009;361(9):868–77. This study shows that high-sensitive TnI improves early diagnosis of acute MI in 1818 constitutive patients on admission and 3 hours and 6 hours after the admission.
Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116(2):281–97.
Ambros V. The functions of animal microRNAs. Nature. 2004;431(7006):350–5.
Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136(2):215–33.
Bentwich I, Avniel A, Karov Y, Aharonov R, Gilad S, Barad O, et al. Identification of hundreds of conserved and nonconserved human microRNAs. Nat Genet. 2005;37(7):766–70.
Lewis BP, Burge CB, Bartel DP. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell. 2005;120(1):15–20.
Baek D, Villen J, Shin C, Camargo FD, Gygi SP, Bartel DP. The impact of microRNAs on protein output. Nature. 2008;455(7209):64–71.
da Costa Martins PA, Bourajjaj M, Gladka M, Kortland M, van Oort RJ, Pinto YM, et al. Conditional dicer gene deletion in the postnatal myocardium provokes spontaneous cardiac remodeling. Circulation. 2008;118(15):1567–76.
da Costa Martins PA, Salic K, Gladka MM, Armand AS, Leptidis S, el Azzouzi H, et al. MicroRNA-199b targets the nuclear kinase Dyrk1a in an auto-amplification loop promoting calcineurin/NFAT signalling. Nat Cell Biol. Dec; 12(12): 1220-7.
van Rooij E, Sutherland LB, Liu N, Williams AH, McAnally J, Gerard RD, et al. A signature pattern of stress-responsive microRNAs that can evoke cardiac hypertrophy and heart failure. Proc Natl Acad Sci U S A. 2006;103(48):18255–60.
Thum T, Gross C, Fiedler J, Fischer T, Kissler S, Bussen M, et al. MicroRNA-21 contributes to myocardial disease by stimulating MAP kinase signalling in fibroblasts. Nature. 2008;456(7224):980–4.
Mitchell PS, Parkin RK, Kroh EM, Fritz BR, Wyman SK, Pogosova-Agadjanyan EL, et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci U S A. 2008;105(30):10513–8.
Gilad S, Meiri E, Yogev Y, Benjamin S, Lebanony D, Yerushalmi N, et al. Serum microRNAs are promising novel biomarkers. PLoS One. 2008;3(9):e3148.
Chen X, Ba Y, Ma L, Cai X, Yin Y, Wang K, et al. Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res. 2008;18(10):997–1006.
Lagos-Quintana M, Rauhut R, Yalcin A, Meyer J, Lendeckel W, Tuschl T. Identification of tissue-specific microRNAs from mouse. Curr Biol. 2002;12(9):735–9.
Zhang C. MicroRNomics: a newly emerging approach for disease biology. Physiol Genomics. 2008;33(2):139–47.
Wang K, Zhang S, Marzolf B, Troisch P, Brightman A, Hu Z, et al. Circulating microRNAs, potential biomarkers for drug-induced liver injury. Proc Natl Acad Sci U S A. 2009;106(11):4402–7.
Laterza OF, Lim L, Garrett-Engele PW, Vlasakova K, Muniappa N, Tanaka WK, et al. Plasma MicroRNAs as sensitive and specific biomarkers of tissue injury. Clin Chem. 2009;55(11):1977–83.
Gladka MM, da Costa Martins PA, De Windt LJ. Small changes can make a big difference - MicroRNA regulation of cardiac hypertrophy. J Mol Cell Cardiol. Sep 24.
•• D’Alessandra Y, Devanna P, Limana F, Straino S, Di Carlo A, Brambilla PG, et al. Circulating microRNAs are new and sensitive biomarkers of myocardial infarction. Eur Heart J. Nov; 31(22): 2765–73. This work identifies miR-1, miR-133a, miR-133b, and miR-499 as the most up-regulated miRs in the circulation early after the MI in 33 STEMI patients. In addition, miR-208a is increased in a mouse model of MI.
•• Gidlof O, Andersson P, van der Pals J, Gotberg M, Erlinge D. Cardiospecific microRNA plasma levels correlate with troponin and cardiac function in patients with st elevation myocardial infarction, are selectively dependent on renal elimination, and can be detected in urine samples. Cardiology. 118(4): 217–26. This study demonstrates an increase in miR-1, miR-133a, miR-208b, and miR-499 in the circulation after MI in 25 STEMI patients and in a pig model. In addition, miR-208b correlates with TnT levels after myocardial infarction.
•• Wang GK, Zhu JQ, Zhang JT, Li Q, Li Y, He J, et al. Circulating microRNA: a novel potential biomarker for early diagnosis of acute myocardial infarction in humans. Eur Heart J. Mar; 31(6): 659-66. This study shows an increase in miR-1, miR-133a, miR-208a, and miR-499 in the circulation after MI in 33 AMI patients and in a rat model. Among these miRs, miR-208a has the best specificity and sensitivity and is detected early after the onset of symptoms.
•• Ai J, Zhang R, Li Y, Pu J, Lu Y, Jiao J, et al. Circulating microRNA-1 as a potential novel biomarker for acute myocardial infarction. Biochem Biophys Res Commun. Jan 1; 391(1): 73-7. This work shows increase in circulating miR-1 levels in 93 AMI patients and correlation with QRS widening.
•• Cheng Y, Tan N, Yang J, Liu X, Cao X, He P, et al. A translational study of circulating cell-free microRNA-1 in acute myocardial infarction. Clin Sci (Lond). Jul; 119(2): 87-95. This study demonstrates increased levels of miR-1 in the circulation after the MI in 31 AMI patients and in a rat model of MI. Furthermore, miR-1 correlates with CK-MB in AMI patients, with infarct size in the animal model and with cell damage in vitro.
•• Widera C, Gupta SK, Lorenzen JM, Bang C, Bauersachs J, Bethmann K, et al. Diagnostic and prognostic impact of six circulating microRNAs in acute coronary syndrome. J Mol Cell Cardiol. Nov; 51(5): 872-5. This work shows elevated miR-1, miR-133a, and miR-208b levels in the circulation of 196 STEMI patients. These miRs correlated with high-sensitive TnT.
•• Corsten MF, Dennert R, Jochems S, Kuznetsova T, Devaux Y, Hofstra L, et al. Circulating MicroRNA-208b and MicroRNA-499 reflect myocardial damage in cardiovascular disease. Circ Cardiovasc Genet. Dec; 3(6): 499-506. This study indentifies miR-208b and miR-499 as the most upregulated miRs in the circulation after MI in 32 AMI patients and both miRs correlate with TnT levels.
van Rooij E, Quiat D, Johnson BA, Sutherland LB, Qi X, Richardson JA, et al. A family of microRNAs encoded by myosin genes governs myosin expression and muscle performance. Dev Cell. 2009;17(5):662–73.
Bell ML, Buvoli M, Leinwand LA. Uncoupling of expression of an intronic microRNA and its myosin host gene by exon skipping. Mol Cell Biol. Apr; 30(8): 1937-45.
Kim HJ, Cui XS, Kim EJ, Kim WJ, Kim NH. New porcine microRNA genes found by homology search. Genome. 2006;49(10):1283–6.
Wang JX, Jiao JQ, Li Q, Long B, Wang K, Liu JP, et al. miR-499 regulates mitochondrial dynamics by targeting calcineurin and dynamin-related protein-1. Nat Med. Jan; 17(1): 71-8.
Adachi T, Nakanishi M, Otsuka Y, Nishimura K, Hirokawa G, Goto Y, et al. Plasma microRNA 499 as a biomarker of acute myocardial infarction. Clin Chem. Jul; 56(7): 1183-5.
Morkin E. Control of cardiac myosin heavy chain gene expression. Microsc Res Tech. 2000;50(6):522–31.
Narolska NA, Eiras S, van Loon RB, Boontje NM, Zaremba R, Spiegelen Berg SR, et al. Myosin heavy chain composition and the economy of contraction in healthy and diseased human myocardium. J Muscle Res Cell Motil. 2005;26(1):39–48.
• Meder B, Keller A, Vogel B, Haas J, Sedaghat-Hamedani F, Kayvanpour E, et al. MicroRNA signatures in total peripheral blood as novel biomarkers for acute myocardial infarction. Basic Res Cardiol. Jan; 106(1): 13-23. This work demonstrates a multi-marker approach for an miR signature as novel biomarkers for the MI.
Hanke M, Hoefig K, Merz H, Feller AC, Kausch I, Jocham D, et al. A robust methodology to study urine microRNA as tumor marker: microRNA-126 and microRNA-182 are related to urinary bladder cancer. Urol Oncol. Nov-Dec; 28(6): 655-61.
Park NJ, Zhou H, Elashoff D, Henson BS, Kastratovic DA, Abemayor E, et al. Salivary microRNA: discovery, characterization, and clinical utility for oral cancer detection. Clin Cancer Res. 2009;15(17):5473–7.
• Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, Lotvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9(6):654–9. This study shows that exosomes contain both mRNAs and miRs, which can be transported to other cells and are stable in the circulation.
• Hunter MP, Ismail N, Zhang X, Aguda BD, Lee EJ, Yu L, et al. Detection of microRNA expression in human peripheral blood microvesicles. PLoS One. 2008;3(11):e3694. This work demonstrates that microvesicles in peripheral blood carry miRs with high stability.
Ratajczak J, Wysoczynski M, Hayek F, Janowska-Wieczorek A, Ratajczak MZ. Membrane-derived microvesicles: important and underappreciated mediators of cell-to-cell communication. Leukemia. 2006;20(9):1487–95.
Suleymanoglu E. Phospholipid-nucleic acid recognition: developing an immobilized liposome chromatography for DNA separation and analysis. PDA J Pharm Sci Technol. 2006;60(4):232–9.
Janas T, Yarus M. Specific RNA binding to ordered phospholipid bilayers. Nucleic Acids Res. 2006;34(7):2128–36.
Manavbasi Y, Suleymanoglu E. Nucleic acid-phospholipid recognition: Fourier transform infrared spectrometric characterization of ternary phospholipid-inorganic cation-DNA complex and its relevance to chemicopharmaceutical design of nanometric liposome based gene delivery formulations. Arch Pharm Res. 2007;30(8):1027–40.
Mengistu DH, Bohinc K, May S. Binding of DNA to zwitterionic lipid layers mediated by divalent cations. J Phys Chem B. 2009;113(36):12277–82.
Lou B, Liao XL, Wu MP, Cheng PF, Yin CY, Fei Z. High-density lipoprotein as a potential carrier for delivery of a lipophilic antitumoral drug into hepatoma cells. World J Gastroenterol. 2005;11(7):954–9.
Kim SI, Shin D, Choi TH, Lee JC, Cheon GJ, Kim KY, et al. Systemic and specific delivery of small interfering RNAs to the liver mediated by apolipoprotein A-I. Mol Ther. 2007;15(6):1145–52.
• Vickers KC, Palmisano BT, Shoucri BM, Shamburek RD, Remaley AT. MicroRNAs are transported in plasma and delivered to recipient cells by high-density lipoproteins. Nat Cell Biol. Apr; 13(4): 423-33. This study identifies HDL as transport system for miRs in the circulation, which enables intracellular communication between the cells.
Zernecke A, Bidzhekov K, Noels H, Shagdarsuren E, Gan L, Denecke B, et al. Delivery of microRNA-126 by apoptotic bodies induces CXCL12-dependent vascular protection. Sci Signal. 2009;2(100):ra81.
Wang K, Zhang S, Weber J, Baxter D, Galas DJ. Export of microRNAs and microRNA-protective protein by mammalian cells. Nucleic Acids Res. Nov; 38(20): 7248-59.
• Arroyo JD, Chevillet JR, Kroh EM, Ruf IK, Pritchard CC, Gibson DF, et al. Argonaute2 complexes carry a population of circulating microRNAs independent of vesicles in human plasma. Proc Natl Acad Sci U S A. Mar 22; 108(12): 5003-8. This work implies that the majority of the circulating miRs are protein and especially Ago2 bound.
Turchinovich A, Weiz L, Langheinz A, Burwinkel B. Characterization of extracellular circulating microRNA. Nucleic Acids Res. Sep 1; 39(16): 7223-33.
Wang R, Li N, Zhang Y, Ran Y, Pu J. Circulating MicroRNAs are promising novel biomarkers of acute myocardial infarction. Intern Med. 50(17): 1789-95.
Disclosure
L.J. De Windt has received grants (payable to his institution) from Dutch Heart Foundation program (grant NHS2007B167), the Center of Translational Molecular Medicine (CTMM), VIDI award 917-863-72 from the Netherlands Organization for Health Research and Development, the Fondation Leducq Transatlantic Network of Excellence program 08-CVD-03, and CVON, an initiative of the Dutch Heart Foundation, NFU, KNAW and NWO/ZonMW.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Salic, K., De Windt, L.J. MicroRNAs as Biomarkers for Myocardial Infarction. Curr Atheroscler Rep 14, 193–200 (2012). https://doi.org/10.1007/s11883-012-0238-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11883-012-0238-z