Abstract
Purpose of Review
Chemosensory dysfunction in the patients with COVID-19 has been reported frequently in the studies from different regions of the world. However, the prevalence of smell and/or taste disorders presents significant ethnic and geographic variability. In addition, the pathogenesis of chemosensory dysfunction remains unclarified.
Recent Findings
This is a narrative review on the recent state of the prevalence, mechanism, and diagnostic and therapeutic strategy of chemosensory dysfunction in COVID-19 patients during the global pandemic. The chemosensory dysfunction was analysis based on recent studies, which either used questionnaires, Likert scales (0–10), or smell tests to estimate the smell and taste dysfunction. The ethnic and geographic difference of the prevalence of smell and/or taste disorders and the potential underlying mechanisms have been discussed. Several suggestions on the diagnosis and treatment of COVID-19 patients with smell and taste disorders were summarized for the physicians.
Summary
This review provides a comprehensive overview of the current studies regarding the chemosensory dysfunction during the COVID-19 worldwide outbreak.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A cluster of viral pneumonia cases named as coronavirus disease 2019 (COVID-19) has been reported since the end of 2019. Subsequently, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been identified to be the pathogenic cause of COVID-19 [1, 2]. This newly recognized illness has spread rapidly and affects tens of millions of people all over the world [1,2,3]. The clinical spectrum of COVID-19 ranges from asymptomatic to severe ill cases [1,2,3]. Although the most common symptoms of COVID-19 include fever, dyspnea, cough, nausea, and vomiting [1,2,3,4], loss of smell and/or taste has been increasingly recognized as prevalent and early onset symptoms in a considerable number of patients [3, 5,6,7]. However, the clinical characteristics and underlying mechanisms of the smell and/or taste disorders remain incompletely understood. In fact, the etiopathogenesis of chemosensory dysfunction is very complicated [8, 9]. Due to the difficulty in classification of chemosensory disorders, increasing chemosensory researches have evolved to describe olfactory dysfunction according to putative underlying etiologies [8]. The common causes of olfactory dysfunction include olfactory dysfunction secondary to sinonasal diseases, post-infectious olfactory dysfunction, post-traumatic olfactory dysfunction, olfactory dysfunction associated with neurological disease, and olfactory dysfunction associated with exposure or drugs/toxins [8]. Among these causes contributing to the clinically presented smell and taste disorders, upper respiratory tract infections are one of the most common causes [8, 9]. Although a variety of pathogens can cause post-infectious olfactory dysfunction, including viruses, bacteria, fungi, and even some rare organisms such as microfilaria [8], the most common pathogens are respiratory viruses including those causing common cold and influenza [8]. It is very likely that SARS-CoV-2 may cause a typical post-infectious olfactory and smell dysfunction as viruses causing common cold, such as rhinovirus and adenovirus [10, 11••, 12••, 13••]. However, as a newly identified disease, many details in the SARS-CoV-2 induced chemosensory dysfunction including its prevalence, clinical features, underlying mechanism, and treatment in patients with COVID-19 remain to be clarified.
The Prevalence of Chemosensory Dysfunction in COVID-19 Patients with Different Ethnic Background and in Different Geographic Area
A number of studies have reported the prevalence of smell and taste dysfunction in COVID-19 patients, however, the results initially appeared to be confusing [14]. In the first few months of the COVID-19 pandemic, smell and taste dysfunction have not been noted as a common symptom of the patients with COVID-19. Mao and colleagues found that only 5.1% and 5.6% patients with COVID-19 in Wuhan, China reported smell and taste impairment, respectively [15]. Other early studies on the clinical characteristics of COVID-19 in China even did not mentioned the smell or taste dysfunctions [1, 16, 17]. Nevertheless, almost at the same time period, Giacomelli A et al. in Italy, where is the original epicenter of the COVID-19 pandemic in Europe, found that 20 (33.9%) of patients had at least one taste or olfactory disorder based on an interview to 59 hospitalized patients [2]. Later, Gane SB et al. discovered that the increase in the reported and referred sudden anosmia correlated with the numbers of diagnosed cases of COVID-19 at the beginning of the outbreak in the UK [6]. Subsequent further studies in Europe reported that about 75–85% of COVID-19 patients had olfactory dysfunction [3, 10, 18,19,20]. In Spain, the incidence of chemosensory dysfunction in COVID-19 patients reached up to 90% [10, 21]. Similar prevalence of smell and taste disorder has been found in COVID-19 patients in the USA [5, 22,23,24,25,26]. Although several later studies in China reported higher prevalence of chemosensory dysfunction than that reported by Mao, none reported a prevalence as high as those reported in Europe and the USA, without exceeding 50% [27, 28]. Thus, the incidence of chemosensory dysfunction in COVID-19 patients seems much lower in China compared with those in Europeans and Americans [3, 5, 15, 19, 22,23,24,25,26,27,28,29]. One of the potential reasons may be that the symptom of chemosensory dysfunction was overlooked due to the incomplete medical recording under urgent admission. During the outbreak of COVID-19 in Wuhan, China, a lot of physicians in the departments other than internal medicine and otolaryngology, such as those in general surgery department, were recruited to participate in dealing with surging patients with COVID-19. Unlike general symptoms (i.e., fever, dyspnea, and cough), smell and taste dysfunction were likely to be overlooked by those physicians. In order to explore the frequencies of COVID-19 patients with chemosensory dysfunction in China more accurately, we have conducted telephone follow-up to rechecked the hospital medical records for COVID-19 patients discharged from Tongji Hospital, the largest designated hospital to treat patients with COVID-19, in Wuhan, China [29]. Nevertheless, even with this effort, we still found low incidences of smell and taste dysfunction in Chinese patients with COVID-19, with 11.4 and 20.6% of them complaining loss of smell and taste, respectively [29]. It should be noted that most studies from China including ours only investigated the hospitalized patients. Several studies have indicated that smell loss in COVID-19 patients may associate with a milder clinical course [5, 30]. Loss of smell and taste may be more common in mild patients or asymptomatic patients, who are not hospitalized. Therefore, in order to get an accurate figure of smell and taste disorder in COVID-19 patients, both hospitalized and non-hospitalized patients with a large sample size should be investigated. Notwithstanding, similar to Chinese data, low incidences of smell and taste dysfunction have been reported in COVID-19 patients in Japan and Korea (Fig. 1) [31,32,33]. The potential ethnic difference in the prevalence of chemosensory disorders of COVID-19 patients, especially between the populations in East Asia and Western countries (Fig. 1), has also been noted by other researches [14, 34,35,36]. A meta-analysis including one hundred four studies and over thirty thousand patients revealed that Caucasians had a three times higher prevalence of chemosensory dysfunctions than Asians [14]. However, there are not sufficient data yet on populations in Africa, South America, or South Asia to compare the prevalence of smell and taste disorder in these populations with the populations in East Asia, Europe and North America. In the meta-analysis by Bartheld and colleagues, the overall prevalence of smell and taste dysfunction in patients with COVID-19 was calculated to be about 43–44% globally [12••, 14].
Until now, most of studies calculated the prevalence of smell and taste disorder depending on the patients’ self-report and subjective impressions without smell function test [34, 36, 37]. But, Agyeman et al. have discovered a higher prevalence of olfactory dysfunction with the use of objective measurements compared with that self-reported [36]. Moreover, a systematic review and meta-analysis indicated that the frequencies of olfactory dysfunction in COVID-19 patients tended to differ between those generated via smell testing (76%) and those based on survey/questionnaire report (53%), which was close to reach statistical significance (P = 0.089) [38]. Therefore, more studies based on objective estimation of chemosensory function are needed to clarify the precise incidences of smell and/or taste dysfunction in COVID-19 patients.
There are several other possible explanations for the ethnic and geographic difference of chemosensory dysfunctions in COVID-19 patients. First, the genetic variation of the virus may influence the virulence of SARS-CoV-2. Variants of SARS-CoV-2 show geographic differences, and mutations in the gene encoding Spike protein are being continuously reported [39, 40]. Three central variants of SARS-CoV-2 distinguished by amino acid changes have been found, which are named as types A, B, and C, with type A being the ancestral type [41]. Type B is predominant in East Asia, while both Type A and Type C occur outside of East Asia [41]. In addition, recent studies demonstrated that a new SARS-CoV-2 strain with one particular mutation or rather SNP variant of Spike protein (G614) has become the dominant strain in the pandemic, while the ancestral strain with the Spike protein variant of D614 was initially dominant in East Asia [40]. The frequency of G614 is increasing in Europe significantly in a few months after outbreak [40]. In addition, the patients with G614 variant may have higher upper respiratory tract viral loads, although it is likely but not yet entirely clear that it is clinically more infectious than D614 [42]. However, it is possible that the COVID-19 patients infected by different variants of SARS-CoV-2 may present different severities of chemosensory dysfunctions, due to the different viral loads in upper respiratory tract. This possibility requires further attention and in-depth studies to determine.
The second factor that may contribute to the difference in chemosensory dysfunctions is the variation of the host susceptibility. Similar to the variation of virus, there may be genetic polymorphisms in the SARS-CoV-2 receptor angiotensin-converting enzyme 2 (ACE2) and transmembrane serine protease 2 (TMPRSS2) in humans. Recent evidences have revealed the genetic differences in ACE2 between East Asians and Europeans [43,44,45]. However, these studies were focused on the expression of ACE2 variants in lung tissues and their association with the disease severity of COVID-19. There is no study yet that has explored the expression of ACE2 variants in the olfactory epithelium and their association with the prevalence of chemosensory dysfunction in COVID-19 patients. In addition to ACE2, a preprinted study demonstrated that TMPRSS2, which is able to facilitate the entry of SARS-CoV-2 by cleaving the Spike protein, presented much higher levels in lung tissues in Europeans than in East Asians [46]. Generally, based on the data to date, there are probably two main factors causing the different prevalence of chemosensory dysfunction in different populations. First, the ethnic background may lead to different susceptibilities and host responses to the infection of SARS-CoV-2; second, there are different dominated strains of SARS-CoV-2 in different geographic regions. The specific regional prevalence of chemosensory dysfunction in COVID-19 patients potentially depends on the interaction of these two factors. Apparently, more studies are needed to clarify the relationship between these two factors.
With the swift spread of COVID-19 cases, development of reliable, accurate, and simplified methodologies to predict and diagnose SARS-CoV-2 infection is critical to control its spread. Since many patients reported chemosensory dysfunctions as their first or one of the early onset symptoms in Western countries, several studies assessed the predictive value of chemosensory dysfunction in the diagnosis of COVID-19 [47,48,49]. Roland et al. developed a smell and taste symptom-based model for COVID-19 diagnosis based on the data in the USA, which predicted 75% of COVID-19 test results [48]. Similarly, several European groups also suggested the predictive value of chemosensory dysfunction in the diagnosis of COVID-19 [47, 49]. Nevertheless, given the lower incidence of smell and/or taste disorders in East Asians compared with Western populations, the value of using chemosensory dysfunction as a diagnostic parameter of COVID-19 in East Asia patients is questionable (Fig. 1).
The Underlying Mechanism of Chemosensory Dysfunction in Patients with COVID-19
To date, the exact pathogenesis of chemosensory dysfunction in patients with COVID-19 remains unclear. The chemosensory dysfunctions of COVID-19 patients usually are sudden onset and typically transient, which last for several days to a few weeks [3, 29, 32]. The timing and duration of the smell and taste disorders in COVID-19 patients can provide important clues about their underlying mechanisms. The COVID-19-related chemosensory dysfunctions seem similar to those occurred after infection of common upper respiratory tract viruses such as rhinovirus, adenovirus, and coronavirus [8, 9, 50]. However, the chemosensory dysfunctions caused by SARS-CoV-2 show rather distinct clinical features from those in SARS pandemic, in which few cases of anosmia were reported [51].
Regarding the mechanisms underlying smell and/or taste disorders in COVID-19 patients, the first question required to be answered is the relationship between chemosensory dysfunction and nasal obstruction/congestion and rhinorrhea. Common respiratory viral infections cause nasal obstruction, congestion, and rhinorrhea [8, 52, 53]. The physical obstruction may impede odorant access to the sensory epithelium, which cause the loss of smell by preventing the binding of the odorants to olfactory receptors [8]. However, this possibility in COVID-19 is disfavored by findings that most of the COVID-19 patients with smell disorder do not have nasal obstruction or rhinorrhea [3, 47, 54, 55]. We also found that there was no correlation between the severity scores of the chemosensory disorders and the upper respiratory symptom scores including nasal obstruction, rhinorrhea, and sneezing [29] in patients with COVID-19. Nevertheless, the localized edema of the olfactory clefts (OC) has recently been revealed by magnetic resonance imaging in patients with COVID-19 [56], which may impair odorant access to the sensory epithelium without resulting in obvious nasal obstruction. Another important mechanism underlying acute respiratory viral-induced smell disorder is the pathological alteration of olfactory epithelium caused by viral infection, including mucosa swelling, mucus overproduction, and disruption of olfactory cells [13••]. Although ACE2 has been found expressed by nasal ciliated and secretory cells [57, 58], olfactory neurons have no significant expression of ACE2 and TMPRSS2 [58, 59, 60••]. In contrast, support cells in the olfactory epithelium, such as sustentacular cells, have abundant expression of ACE2 and TMPRSS2 [12••]. The function of olfactory neurons may be impaired indirectly by the disruption of olfactory epithelium structure, which is caused by the infection of supporting cells. A recent murine study demonstrated that the damages of olfactory nervous system were associated with infection of a large proportion of sustentacular cells, but no SARS-CoV-2 was detected in the olfactory bulbs [61]. Regeneration of sustentacular cells occurs much faster than olfactory neurons [61, 62]; thereby rapid replenishment of sustentacular cells is consistent with the rapid recovery of the smell disorder observed in COVID-19 patients. Nevertheless, long-lasting olfactory dysfunction was reported in a small portion of COVID-19 cases, which is possible due to the persistent impairment of olfactory sensory neurons after the disruption of olfactory epithelium structure. It is also possible that the dysfunction of olfactory nervous system may be secondary to the inflammatory response induced by viral infection. Local cytokines such as IL-6 have been found associated with the olfactory neuron dysfunction [63, 64]. An autopsy study revealed that the olfactory epithelium of COVID-19 patients had prominent leukocytic infiltration, which is associated with neuritis and axonal damage of olfactory nerve [65]. It indicates that the localized inflammation caused by SARS-CoV-2 can damage the neuron or olfactory nerve.
Besides smell disorder, taste functions are also impaired in a considerable number of patients with COVID-19 [11••, 12••, 29]. In some cases, the taste dysfunction was more significant than smell dysfunction [29, 50]. It suggests that taste disturbances in COVID-19 patients appear to reflect an impairment in gustatory abilities, and not purely a retronasal olfactory dysfunction [50]. Taste disorder can result from both peripheral and central pathological involvement of the pathways of gustatory. It was shown that inflammatory cytokines induced by virus infection was able to alter normal taste transduction and cell turnover in taste buds [63, 66]. Due to the cytokine storm in patients with COVID-19, it can be proposed that high levels of inflammatory cytokines, such as IL-6, IL-1β, and tumor necrosis factor α, may induce damage of taste receptors and alters their transduction function. ACE2 and TMPRSS2 have been found expressed by taste receptor cells [13, 64], suggesting that the machinery necessary for SARS-CoV-2 infection in taste-relevant cells may be present. Adult taste stem cells locate in the posterior tongue [67]. A murine study revealed that murine stem cells also express ACE2 and TRMPSS2 [68], underling the possibility that taste dysfunction may be caused or exacerbated by insufficient taste receptor cell renewal due to SARS-CoV-2-induced stem cell damage. In addition, the inflammation response can reduce taste stem cell output, which in turn leads to depopulated taste buds and perturbed taste function [13, 69,70,71]. It has been demonstrated that the local inflammation induced by SARS-CoV-2 was able to alter stem cell properties and ultimately influence taste perception [13••]. However, the evidence so far is limited, and obtaining more extensive data regarding SARS-CoV-2 relevant gene and protein expressions in taste epithelial cells may provide a better basis from which to propose mechanistic hypotheses.
The Diagnostic and Therapeutic Strategy of Chemosensory Dysfunctions in Patients with COVID-19
The chemosensory dysfunctions in COVID-19 patients present several characteristics, including high prevalence, particularly in Western countries, sudden onset, a rapid recovery in most cases, as well as the fact that the smell or taste dysfunction can be the only symptom and presents without nasal congestion and rhinorrhea [11••, 12••, 29]. In patients with mild diseases or at the early stage of the disease, chemosensory dysfunction may have certain diagnostic value of COVID-19 during the pandemic.
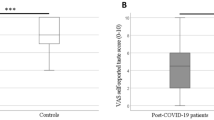
To date, the majority of clinical studies on the chemosensory dysfunction in COVID-19 patients were based on the self-reported data [3, 12••, 13••, 29, 43, 45]. These data were anamnestic-observational and lack of quantitative assessment. To quantify the severity of smell and taste disorder, a visual analogue scale (VAS, 0–10 cm) can be used. It is easy to use and safe to be performed in daily clinical practice without close contact between health professionals and patients, although it is also a sort of self-reported information of patients [11••, 29]. In addition, subjective tests including olfactometry and chemical gustometry are more precise with the ability to quantify the extent of the dysfunction and to monitor the recovery over time [36, 37]. However, due to the risk of virus transmission, the objective chemosensory tests used in a face-to-face application in COVID-19 pandemic must be chosen with extreme caution. With appropriate training, some of these tests can be performed by using video consultations via telemedicine, and this would be safe for both patients and examiners [11••, 72].
General preventive measures of chemosensory dysfunction in the COVID-19 pandemic are to avoid the spread of the virus. Personal hygiene including hand washing, mask wearing, as well as the policies of social distancing, preventive home isolation, and extensive diagnostic tests are the first and most important measures [73]. Although several treatments have been recommended for the post-viral loss of smell and taste, there is no sufficient evidence for any specific pharmacological option for the virus-caused chemosensory dysfunction including SARS-CoV-2 [74]. The most common empirical treatment for olfactory disorder is corticosteroids, including intranasal and/or systemic [8]. However, the benefit of steroids for the post-virus olfactory dysfunction, especially in COVID-19 patients, remains unclear. The corticosteroids are the first-line therapy for a nasal inflammatory diseases such as allergic rhinitis (AR) and chronic rhinosinusitis (CRS), which present high prevalence in general population, and the discontinuation of intranasal glucocorticoid treatment is not recommended in the COVID-19 pandemic [11••, 75]. Whether this strategy may show benefit on limiting the onset or duration of olfactory dysfunction in COVID-19 patients with concomitant AR or CRS is interesting to know. Further retrospective or prospective studies may focus on this issue to promote the therapeutic strategy for chemosensory dysfunction in COVID-19 patients with AR or CRS. Of note, most of the COVID-19 patients with loss of smell and/or taste disorders may recover within the first month after disease onset, at least partly [11••, 12••, 13••, 29, 50]. For those with unrecovered or partly recovered smell disorder after 1 month of disease onset, olfactory training is the recommended, which is the only evidence-based therapeutic option for post-viral smell loss currently [11••, 74].
Conclusion and Take-Home Messages
The prevalence of chemosensory dysfunction in patients with COVID-19 show significant geographic and ethnic difference, with up to 70% in western countries, but much lower in East Asia. Chemosensory dysfunction may have diagnostic value for COVID-19 patients during the pandemic, particularly in the western countries. The possible pathogenesis of smell and taste disorders after SARS-CoV-2 infection is complicated. The localized obstruction caused by olfactory cleft edema and the virus induced damage of olfactory epithelium or olfactory central nervous system may be involved. Notwithstanding, it is not too bad that most of the chemosensory dysfunctions in COVID-19 patients recover spontaneously in a short period of time after infection and glucocorticoids treatment and olfactory and gustatory training may be considered for the unrecovered patients.
Grant Support
This study was supported by grants from the National Natural Science Foundation of China (NSFC) [81920108011 and 81630024 (Z.L.), and 82071025 (M.Z.)] and the Natural Science Foundation of Hubei Province, China [2018CFB602 (M.Z.)].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
Giacomelli A, Pezzati L, Conti F, Bernacchia D, Siano M, Oreni L, et al. Self-reported olfactory and taste disorders in patients with severe acute respiratory coronavirus 2 infection: a cross-sectional study. Clin Infect Dis. 2020;71(15):889–90.
Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020;277(8):2251–61.
Mullol J, Mariño-Sánchez F, Valls M, Alobid I, Marin C. The sense of smell in chronic rhinosinusitis. J Allergy Clin Immunol. 2020;145(3):773–6.
Yan CH, Faraji F, Prajapati DP, Ostrander BT, DeConde AS. Self-reported olfactory loss associates with outpatient clinical course in COVID-19. Int Forum Allergy Rhinol. 2020;10(7):821–31.
Gane SB, Kelly C, Hopkins C. Isolated sudden onset anosmia in COVID-19 infection. A novel syndrome? Rhinology. 2020;58(3):299–301.
Soler ZM, Patel ZM, Turner JH, Holbrook EH. A primer on viral-associated olfactory loss in the era of COVID-19. Int Forum Allergy Rhinol. 2020;10(7):814–20.
Hummel T, Whitcroft KL, Andrews P, Altundag A, Cinghi C, Costanzo RM, et al. Position paper on olfactory dysfunction. Rhinology. 2017;0(0):1–30.
Jaume F, Quintó L, Alobid I, Mullol J. Overuse of diagnostic tools and medications in acute rhinosinusitis in Spain: a population-based study (the PROSINUS study). BMJ Open. 2018;8(1).
Izquierdo-Domínguez A, Rojas-Lechuga MJ, Chiesa-Estomba C, Calvo-Henríquez C, Ninchritz-Becerra E, Soriano-Reixach M, et al. Smell and taste dysfunction in COVID-19 is associated with younger age in ambulatory settings: a Multicenter cross-sectional study. J Investig Allergol Clin Immunol. 2020;30(5):346–57.
•• Mullol J, Alobid I, Mariño-Sánchez F, Izquierdo-Domínguez A, Marin C, Klimek L, et al. The loss of smell and taste in the COVID-19 Outbreak: a tale of many countries. Curr Allergy Asthma Rep. 2020;20(10). COMMENT: Summary of the main points of the smell and taste disorders in the COVID-19 worldwide outbreak.
•• Butowt R, von Bartheld CS. Anosmia in COVID-19: Underlying mechanisms and assessment of an olfactory route to brain infection. The Neuroscientist. 2020:1073858420956905 COMMENT: Excellent overview of olfactory dysfunction in COVID-19 from the perspective of neuroscience.
•• Cooper KW, Brann DH, Farruggia MC, Bhutani S, Pellegrino R, Tsukahara T, et al. COVID-19 and the chemical senses: supporting players take center stage. Neuron. 2020;107(2):219–33. COMMENT: Explanation of the underlying mechanisms of chemical senses disorders in COVID-19.
von Bartheld CS, Hagen MM, Butowt R. Prevalence of chemosensory dysfunction in COVID-19 patients: a systematic review and meta-analysis reveals significant ethnic differences. ACS Chem Neurosci. 2020;11(19):2944–61.
Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6).
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China The Lancet. 2020;395(10223):497–506.
Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130(5):2620–9.
Patel A, Charani E, Ariyanayagam D, Abdulaal A, Denny SJ, Mughal N, et al. New-onset anosmia and ageusia in adult patients diagnosed with SARS-CoV-2 infection. Clin Microbiol Infect. 2020;26(9):1236–41.
Paderno A, Schreiber A, Grammatica A, Raffetti E, Tomasoni M, Gualtieri T, et al. Smell and taste alterations in COVID-19: a cross-sectional analysis of different cohorts. Int Forum Allergy Rhinol. 2020;10(8):955–62.
Villarreal IM, Morato M, Martínez-RuizCoello M, Navarro A, Garcia-Chillerón R, Ruiz Á, et al. Olfactory and taste disorders in healthcare workers with COVID-19 infection. Eur Arch Otorhinolaryngol. 2020;1–5.
Rojas-Lechuga MJ, Izquierdo-Domínguez A, Chiesa-Estomba C, Calvo-Henríquez C, Villarreal IM, Cuesta-Chasco G, et al. Chemosensory dysfunction in COVID-19 out-patients. Eur Arch Otorhinolaryngol. 2020.
Yan CH, Faraji F, Prajapati DP, Boone CE, DeConde AS. Association of chemosensory dysfunction and COVID-19 in patients presenting with influenza-like symptoms. Int Forum Allergy Rhinol. 2020;10(7):806–13.
Kempker RR, Kempker JA, Peters M, Rebolledo PA, Carroll K, Toomer L, et al. Loss of smell and taste among healthcare personnel screened for coronavirus 2019. Clin Infect Dis. 2020;ciaa877.
Chiesa-Estomba CM, Lechien JR, Portillo-Mazal P, Martínez F, Cuauro-Sanchez J, Calvo-Henriquez C, et al. Olfactory and gustatory dysfunctions in COVID-19. First reports of Latin-American ethnic patients. Am J Otolaryngol. 2020;41(5):102605.
Carignan A, Valiquette L, Grenier C, Musonera JB, Nkengurutse D, Marcil-Héguy A, et al. Anosmia and dysgeusia associated with SARS-CoV-2 infection: an age-matched case–control study. Can Med Assoc J. 2020;192(26):E702–E7.
Lee DJ, Lockwood J, Das P, Wang R, Grinspun E, Lee JM. Self-reported anosmia and dysgeusia as key symptoms of coronavirus disease 2019. Cjem. 2020;22(5):595–602.
Cho RHW, To ZWH, Yeung ZWC, Tso EYK, Fung KSC, Chau SKY, et al. COVID-19 viral load in the severity of and recovery from olfactory and gustatory dysfunction. Laryngoscope. 2020;130:2680–5.
Liang Y, Xu J, Chu M, Mai J, Lai N, Tang W, et al. Neurosensory dysfunction: a diagnostic marker of early COVID-19. Int J Infect Dis. 2020;98:347–52.
Song J, Deng Y-K, Wang H, Wang Z-C, Liao B, Ma J, et al. Self-reported taste and smell disorders in patients with COVID-19:distinct features in China. medRxiv preprint. 2020;2020. https://doi.org/10.1101/20200409034454.
Lechien JR, Chiesa-Estomba Md CM, Hans S, Barillari Md MR, Jouffe L, Saussez S. Loss of Smell and Taste in 2013 European patients with mild to moderate COVID-19. Ann Intern Med. 2020.
Noh JY, Yoon JG, Seong H, Choi WS, Sohn JW, Cheong HJ, et al. Asymptomatic infection and atypical manifestations of COVID-19: comparison of viral shedding duration. J Inf Secur. 2020.
Lee Y, Min P, Lee S, Kim S-W. Prevalence and duration of acute loss of smell or taste in COVID-19 patients. J Korean Med Sci. 2020;35(18).
Asai N, Sakanashi D, Nakamura A, Kishino T, Kato H, Hagihara M, et al. Clinical manifestations and radiological features by chest computed tomographic findings of a novel coronavirus disease-19 pneumonia among 92 patients in Japan. J Microbiol Immunol Infect. 2020.
Lovato A, Antonini A, de Filippis C. Comment on “The Prevalence of Olfactory and Gustatory Dysfunction in COVID-19 Patients: A Systematic Review and Meta-analysis”. Otolaryngology–Head and Neck Surgery. 2020;163(4):852.
Meng X, Deng Y, Dai Z, Meng Z. COVID-19 and anosmia: a review based on up-to-date knowledge. Am J Otolaryngol. 2020;41(5).
Agyeman AA, Chin KL, Landersdorfer CB, Liew D, Ofori-Asenso R. Smell and taste dysfunction in patients with COVID-19: a systematic review and meta-analysis. Mayo Clin Proc. 2020;95(8):1621–31.
Vaira LA, Deiana G, Fois AG, Pirina P, Madeddu G, De Vito A, et al. Objective evaluation of anosmia and ageusia in COVID-19 patients: single-center experience on 72 cases. Head Neck. 2020;42(6):1252–8.
Pang KW, Chee J, Subramaniam S, Ng CL. Frequency and clinical utility of olfactory dysfunction in COVID-19: a systematic review and meta-analysis. Curr Allergy Asthma Rep. 2020;20(12).
Li Q, Wu J, Nie J, Zhang L, Hao H, Liu S, et al. The impact of mutations in SARS-CoV-2 spike on viral infectivity and antigenicity. Cell. 2020;182(5):1284–94.e9.
Korber B, Fischer WM, Gnanakaran S, Yoon H, Theiler J, Abfalterer W, et al. Tracking Changes in SARS-CoV-2 Spike: Evidence that D614G Increases Infectivity of the COVID-19 Virus. Cell. 2020;182(4):812–27.e19.
Forster P, Forster L, Renfrew C, Forster M. Phylogenetic network analysis of SARS-CoV-2 genomes. Proc Natl Acad Sci. 2020;117(17):9241–3.
Grubaugh ND, Hanage WP, Rasmussen AL. Making sense of mutation: what D614G means for the COVID-19 pandemic remains unclear. Cell. 2020;182(4):794–5.
Benetti E, Tita R, Spiga O, Ciolfi A, Birolo G, Bruselles A, et al. ACE2 gene variants may underlie interindividual variability and susceptibility to COVID-19 in the Italian population. Eur J Hum Genet. 2020.
Cao Y, Li L, Feng Z, Wan S, Huang P, Sun X, et al. Comparative genetic analysis of the novel coronavirus (2019-nCoV/SARS-CoV-2) receptor ACE2 in different populations. Cell Discovery. 2020;6(1).
Strafella C, Caputo V, Termine A, Barati S, Gambardella S, Borgiani P, et al. Analysis of ACE2 genetic variability among populations highlights a possible link with COVID-19-related neurological complications. Genes. 2020;11(7).
Santos NPC, Khayat AS, Rodrigues JCG, Pinto PC, Araujo GS, Pastana LF, et al. TMPRSS2 variants and their susceptibility to COVID-19: focus in East Asian and European populations. medRxiv preprint. 2020;2020. https://doi.org/10.1101/2020060920126680.
Haehner A, Draf J, Dräger S, de With K, Hummel T. Predictive value of sudden olfactory loss in the diagnosis of COVID-19. Orl. 2020;82(4):175–80.
Roland LT, Gurrola JG, Loftus PA, Cheung SW, Chang JL. Smell and taste symptom-based predictive model for COVID-19 diagnosis. Int Forum Allergy Rhinol. 2020;10(7):832–8.
Boudjema S, Finance J, Coulibaly F, Meddeb L, Tissot-Dupont H, Michel M, et al. Olfactory and gustative disorders for the diagnosis of COVID-19. Travel Med Infect Dis. 2020;37:101875.
Huart C, Philpott C, Konstantinidis I, Altundag A, Trecca EMC, Cassano M, et al. Comparison of COVID-19 and common cold chemosensory dysfunction. Rhinology. 2020.
Hwang CS. Olfactory neuropathy in severe acute respiratory syndrome: report of a case. Acta Neurol Taiwanica. 2006;15(1):26–8.
Malhotra P, Luka A, McWilliams CS, Poeth KG, Schwartz R, Elfekey M, et al. Clinical features of respiratory viral infections among inpatients at a major US tertiary care hospital. South Med J. 2016;109(8):481–6.
Pellegrino R, Walliczek-Dworschak U, Winter G, Hull D, Hummel T. Investigation of chemosensitivity during and after an acute cold. Int Forum Allergy Rhinol. 2017;7(2):185–91.
Tong JY, Wong A, Zhu D, Fastenberg JH, Tham T. The prevalence of olfactory and gustatory dysfunction in COVID-19 patients: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2020;163(1):3–11.
Kaye R, Chang CWD, Kazahaya K, Brereton J, Denneny JC. COVID-19 anosmia reporting tool: initial findings. Otolaryngol Head Neck Surg. 2020;163(1):132–4.
Eliezer M, Hamel A-L, Houdart E, Herman P, Housset J, Jourdaine C, et al. Loss of smell in COVID-19 patients: MRI data reveals a transient edema of the olfactory clefts. Neurology. 2020;95:e3145–52.
Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26(5):681–7.
Ziegler CGK, Allon SJ, Nyquist SK, Mbano IM, Miao VN, Tzouanas CN, et al. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181(5):1016–35.e19.
Butowt R, Bilinska K. SARS-CoV-2: olfaction, brain infection, and the urgent need for clinical samples allowing earlier virus detection. ACS Chem Neurosci. 2020;11(9):1200–3.
•• Brann DH, Tsukahara T, Weinreb C, Lipovsek M, Van den Berge K, Gong B, et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Science Advances. 2020;6(31). COMMENT: Study suggests that SARS-CoV-2 infection of non-neuronal cell types leads to olfactory dysfunction in patients with COVID-19.
Bryche B, St Albin A, Murri S, Lacôte S, Pulido C, Ar Gouilh M, et al. Massive transient damage of the olfactory epithelium associated with infection of sustentacular cells by SARS-CoV-2 in golden Syrian hamsters. Brain Behav Immun. 2020;89:579–86.
Jia C, Roman C, Hegg CC. Nickel Sulfate induces location-dependent atrophy of mouse olfactory epithelium: protective and proliferative role of Purinergic receptor activation. Toxicol Sci. 2010;115(2):547–56.
Wang H, Zhou M, Brand J, Huang L. Inflammation and taste disorders. Ann N Y Acad Sci. 2009;1170(1):596–603.
Gibson G, Hevezi P, Moyer BD, Lu M, Gao N, White E, et al. Genome-wide analysis of gene expression in primate taste buds reveals links to diverse processes. PLoS One. 2009;4(7):e6395.
Kirschenbaum D, Imbach LL, Ulrich S, Rushing EJ, Keller E, Reimann RR, et al. Inflammatory olfactory neuropathy in two patients with COVID-19. The Lancet. 2020;396(10245).
Cazzolla AP, Lovero R, Lo Muzio L, Testa NF, Schirinzi A, Palmieri G, et al. Taste and smell disorders in COVID-19 patients: role of Interleukin-6. ACS Chem Neurosci. 2020;11(17):2774–81.
Yee KK, Li Y, Redding KM, Iwatsuki K, Margolskee RF, Jiang P. Lgr5-EGFP Marks taste bud stem/progenitor cells in posterior tongue. Stem Cells. 2013;31(5):992–1000.
Barlow LA, Qin Y, Sukumaran SK, Jyotaki M, Redding K, Jiang P, et al. Gli3 is a negative regulator of Tas1r3-expressing taste cells. PLoS Genet. 2018;14(2):e1007058.
Cadwell K, Kaufman A, Choo E, Koh A, Dando R. Inflammation arising from obesity reduces taste bud abundance and inhibits renewal. PLoS Biol. 2018;16(3):e2001959.
Meyerhof W, Kim A, Feng P, Ohkuri T, Sauers D, Cohn ZJ, et al. Defects in the peripheral taste structure and function in the MRL/lpr mouse model of autoimmune disease. PLoS One. 2012;7(4):e35588.
Cohn ZJ, Kim A, Huang L, Brand J, Wang H. Lipopolysaccharide-induced inflammation attenuates taste progenitor cell proliferation and shortens the life span of taste bud cells. BMC Neurosci. 2010;11(1):72.
Klimek L, Hagemann J, Alali A, Spielhaupter M, Huppertz T, Hörmann K, et al. Telemedicine allows quantitative measuring of olfactory dysfunction in COVID-19. Allergy. 2020.
Pfaar O, Klimek L, Jutel M, Akdis CA, Bousquet J, Breiteneder H, et al. COVID-19 pandemic: practical considerations on the organization of an allergy clinic – an EAACI/ARIA position paper. Allergy. 2020.
Hummel T, Whitcroft KL, Andrews P, Altundag A, Cinghi C, Costanzo RM, et al. Position paper on olfactory dysfunction. Rhinol Suppl. 2017;54(26):1–30.
Bousquet J, Akdis C, Jutel M, Bachert C, Klimek L, Agache I, et al. Intranasal corticosteroids in allergic rhinitis in COVID-19 infected patients: an ARIA-EAACI statement. Allergy. 2020;75:2440–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Rhinosinusitis
Rights and permissions
About this article
Cite this article
Zeng, M., Wang, DY., Mullol, J. et al. Chemosensory Dysfunction in Patients with COVID-19: What Do We Learn from the Global Outbreak?. Curr Allergy Asthma Rep 21, 6 (2021). https://doi.org/10.1007/s11882-020-00987-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s11882-020-00987-5