Abstract
Indoor air pollution is increasingly recognized as a significant risk for respiratory illness, particularly in vulnerable populations. Thirty-six children aged 6–14 years with moderate/severe asthma from inner city areas in New York City were studied for 2-week periods (summer and winter) using diaries and spirometry. Seven-day integrated indoor samples of PM10, PM2.5, trace elements, elemental/organic carbon, black carbon, and criteria gases (NO2, SO2, and O3) were collected in the subjects’ residences. Asthma outcomes included cough and wheeze severity, albuterol use, and pulmonary function. Mixed effects regression models for longitudinal data were used to relate weekly indoor pollutant concentrations to asthma outcomes. Odds ratios (ORs) were calculated for ordinal outcomes. During winter, significant positive associations for average weekly symptom severity scores were seen for NO2 (OR = 2.83; p = 0.02), calcium (OR = 3.29; p = 0.02), and silicon (OR = 3.64; p = 0.04). In summer, chlorine was associated with average weekly symptom scores (OR = 1.85; p = 0.004). Average albuterol puff use per day in winter was associated with NO2 (OR = 5.89; p = 0.009), nickel (OR = 2.27; p = 0.05), and silicon (OR = 5.59; p = 0.05). Albuterol use was not associated with indoor pollutants in summer. Asthma severity was associated with specific indoor pollutants. Seasonal differences were observed by pollutant and by clinical index studied.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the USA, asthma is the most important chronic disease in children and young adults, affecting over 5 million in ages 5 to 17 years (Wang et al. 2005). Asthmatic children are particularly susceptible to the airway effects of inhaled irritants as a result of their smaller lung volumes and unique features of their immune, endocrine, and nervous systems (Selgrade et al. 2006).
Outdoor air pollutants, notably fine particulate matter [PM2.5] and criteria gases (ozone [O3], nitrogen dioxide [NO2], and sulfur dioxide [SO2]), are well recognized as important contributors to exacerbations of asthma (Selgrade et al. 2006; Gielen et al. 1997; Iskandar et al. 2012; Larsen et al. 2002; Peters et al. 1997; Roy et al. 2011; Schachter et al. 2016; Vedal et al. 1998). Indoor air hazards, while recognized as a problem of major concern (Habre et al. 2014a), remain less well characterized. On average, children spend up to 20 h per day indoors (Franklin, 2007, Schwab et al. 1992). While infiltration of outdoor air pollution does significantly contribute to the indoor environment, our previous analysis in these inner-city data indicate that ~ 72% of PM2.5 mass in these homes likely originated from indoor sources (Habre et al. 2014b). Of note, concentrations of indoor pollutants, like outdoor pollutants, are subject to seasonal variation and their effects may also vary from one season to another (Bielroy and Deener, 1998).
In prior analyses of this panel, we examined outdoor pollutants, and their associations with symptoms as well as possible sources of outdoor pollutants (Schachter et al.2016; Habre et al. 2014a; Habre et al. 2014b; Rohr et al. 2014). In this study, we examine the associations of measured indoor pollutants and their seasonal variation on measures of asthma exacerbation in children with moderate to severe asthma living in inner city New York.
Subjects and methods
Overall study design
The study was performed during the summers and winters of 2008 and 2009. Each household was monitored for two 14-day periods, one in each season. Thirty-six children with moderate to severe asthma living in East Harlem and the South Bronx were recruited over this 2-year study period. These areas were selected because of high asthma prevalence (NYC Department of Health and mental Hygiene 2008). Details of the study design may be found in prior publications (Schachter et al. 2016; Habre et al. 2014a; Habre et al. 2014b; Rohr et al. 2014) and are briefly described here. Participants were recruited (day 1) from the Mount Sinai Hospital Emergency Department (ED) and Outpatient Asthma Clinics (OAC). Of the 43 subjects screened, 39 were eligible and 36 completed at least one season’s data collection. Thirty-two subjects completed both seasons.
During each season, indoor air quality was monitored and health outcomes were assessed over 14 days for each subject. On day 7, homes were revisited, equipment and diaries were checked, and subjects re-instructed in proper data collection and spirometry maneuvers. Filters in indoor samplers were switched to allow for the second week’s collection of monitoring data. On day 15, the monitoring equipment and the health outcome data were collected. For each subject beginning on day 1, parents and children recorded pulmonary function twice daily (AM and PM), as well as daily symptom scores and other outcome measures. Outdoor (central site) monitoring for a subset of pollutants started 7 days before the first subject was tested.
Subjects
Subject demographics are listed in Table 1.
Inclusion criteria
Children aged 6–14 years old with moderate to severe asthma living in the studied areas were recruited. Asthma was diagnosed based on the Guidelines for the Diagnosis and Management of Asthma NAEPP Expert Panel Report (2007). Daily use of controller medication for at least 3 months in the past year, use of a beta-agonist at least 4 times per month in any one of the past 3 months, or nocturnal awakenings twice a month in the past 3 months were required for eligibility. All children were determined to be using short acting beta agonists at least once daily at time of recruitment.
Exclusion criteria
We excluded children with active disease other than asthma such as hematologic, endocrine, or cardiac conditions requiring daily medications; families planning to move from their current home within the next 6 months; and families that had members who smoked at home.
Baseline visit
A baseline visit was conducted at the hospital upon recruitment, during which the objectives and requirements were explained to the child’s primary caretaker and the child. A Mount Sinai Institutional Review Board approved the informed consent form (IRB Project 05-0679) and a HIPAA form was read and signed by the parent.
A respiratory history and asthma questionnaire, based on an NIH questionnaire previously used in the Inner City Asthma Study (Kattan et al. 1997), was administered. A physical examination was performed by the study physicians.
In order to determine the allergic status of our subjects, skin prick testing was conducted with 12 standard antigens and 2 controls administered with Multi-Test equipment (Alk-Abello, Horsholm, Denmark) (see Table 2).
Three reproducible spirometric tests meeting American Thoracic Society criteria (Wanger et al. 2005) were administered using the ML 3500 spirometer (Micro Medical, Lewiston, ME). Baseline measurements in the clinic included forced vital capacity (FVC), forced expiratory volume in one second (FEV1), and peak expiratory flow (PEF). Baseline measurements were performed at least 8 h after any bronchodilator treatment had been administered. Results were expressed as their value in L or L/s and as a percent of predicted based on predicted values obtained from NHANES III (children 8–14 years) and Wang et al. (for children less than 8 years) (Hankinson et al. 1999; Wang et al. 1993).
Morbidity assessment
A daily symptom diary (cough and wheeze) with each symptom graded on a scale of 0 to 3 (none = 0, mild = 1, moderate = 2, and severe = 3) as well as medication use (albuterol puffs per day) was recorded by parent and child. The questionnaires were reviewed at the weekly visit. Unscheduled clinic or ED visits and hospitalizations were also recorded. Daily total symptom scores were obtained by adding the severity scores of both cough and wheeze. In order to analyze these data as a function of weekly indoor pollutants, we expressed symptoms in three ways: average daily scores for a given week, the maximum daily score for a given week, and the number of days during a given week with symptom scores greater than 1.
Albuterol use was quantified in two ways: the average number of albuterol inhalations (puffs) per day in a given week and the number of days in a week when the number of albuterol puffs was greater than zero.
Average values for symptom scores and albuterol usage are shown in Table 1.
Pulmonary function
Two daily lung function measurements each consisting of up to six attempts, using a Piko 1 handheld spirometer (nSpire Health Inc. Longmont, CO), were conducted at the subject’s home, with PEF and FEV1 measured morning and evening. Three successful blows (as indicated by the Piko 1 handheld spirometer) were performed at each time point and data exhibiting greater than 5% variability at any time point were discarded. Data were downloaded directly from the spirometer. Percent daily lability in PEF was calculated by dividing the absolute value of the difference between AM and PM values by the AM value as follows: 100 × [(|AM-PM|)/AM].
Air pollutant measurements
The indoor sampling apparatus was placed in participants’ main living area and described in detail in Habre et al. (2014b). Briefly, a multi-pollutant sampler (MPS) was used to collect 7-day integrated PM2.5 samples on 37 mm Teflon and quartz filters (Demokritou et al. 2001; Liu et al. 2003; Sarnat et al. 2005). Teflon filters were analyzed for PM2.5 mass concentration gravimetrically using a Mettler microbalance, and for elemental concentrations using X-ray fluorescence (XRF) analysis (detection limits provided in Supplemental Table 4). Elemental and organic carbon was measured using thermal optical reflectance (TOR) on quartz filters and black carbon using optical reflectance analysis on teflon filters.
Weekly indoor ozone (O3), nitrogen dioxide (NO2), and sulfur dioxide (SO2) gases were collected with passive diffusion using Ogawa badges (https://ogawausa.com/product-category/passive-sampler/) and analyzed using ion chromatography.
Daily outdoor O3 concentrations were obtained from Middle School 302 (MS302) New York State Department of Environmental Conservation ambient monitoring site in the South Bronx and used to calculate weekly averages corresponding to each participant’s home visit.
Data analysis
For symptoms and albuterol use data (ordinal outcomes), odds ratios (ORs) were calculated by employing regression models for longitudinal data using a cumulative logit link function to relate weekly indoor pollutant concentrations to health outcomes in that week. These models were run separately for summer and winter. The analysis was conducted in SAS using the GLIMMIX procedure which allows for the analysis of data sets with missing values. The average percentage of missing symptom data in winter was 5% and in summer 2%.
We analyzed pulmonary function (AM) FEV1 and peak flow lability index treating pulmonary function outcomes as continuous variables in a linear mixed regression model.
Odds ratios were reported per interquartile range (IQR) change in each pollutant’s concentration (Delfino et al. 2003). All ORs were calculated after adjusting for gender and Hispanic ethnicity. We also report ORs and their 95% confidence intervals (CIs) separately with adjustment for outdoor O3.
All statistical analyses were performed using SAS Version 9.2.
Results
Indoor exposure characterization
Descriptive statistics of weekly indoor pollutant concentrations are reported in Table 3 and Supplemental Figure 2. On average, indoor NO2 concentrations were higher in winter (33.2 ppb) than in summer (23.7 ppb), while the reverse was true for O3 with 1.8 ppb in winter and 3.9 ppb in summer. Seasonal differences in indoor PM2.5 and PM10 mass as well as organic and elemental carbon were negligible. Of the PM2.5 elements exhibiting the largest seasonal variation, Al, Ca, Cl, Na, Ni, and Zn measurements were higher in winter than in summer, while K and S measurements were higher in summer than in winter.
Asthma symptoms
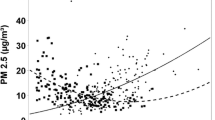
Odds ratios (ORs) and their 95% CIs for the likelihood of increased average daily symptoms scores for a given week (our primary measure) by IQR change in indoor pollutants are shown in (Fig. 1a and Tables 4 and 5). NO2, Ca, and Si were significantly associated with average symptom score during winter, with ORs of 2.83 (95% CI 1.17–6.83), 3.29 (1.26–8.55), and 3.64 (1.10–12.05), respectively. In models adjusted for outdoor O3, ORs were 2.82 (1.10–7.24), 3.46 (1.26–9.52), and 3.73 (1.07–12.99), respectively, and maintained significance (Supplemental Table 1a).
In summer, Cl was significantly associated with average daily symptom score for a given week with OR 1.85 (1.23–2.78). The association increased slightly in O3 adjusted models to 2.02 (1.31–3.12).
Results for other measures of asthma symptoms are shown in Table 4 (base models unadjusted for outdoor O3) and Supplemental Tables 1b-1e (adjusted for outdoor O3).
In winter, results for maximum daily symptom score in a given week (Table 4 and Supplemental Table 1b) were similar to our primary measure (average daily score in a given week). However, in addition to NO2, Ca, and Si for which ORs were 3.13 (1.23–7.96), 4.00 (1.41–11.35), and 5.14 (1.35–19.51), respectively, Ni was also significantly associated with maximum symptoms with OR 1.94 (1.08–3.49). In summer, the maximum symptom score was again significantly associated with Cl (OR 1.82; 95% CI 1.26–2.63) but also negatively with elemental carbon (0.19; 0.06–0.63). For all these associations, there was little change in indoor weekly exposure models adjusted for outdoor O3 (Table 4 and Supplemental Table 1c).
Similar season-specific results were observed when symptom severity was measured as number of days with symptom scores > 1 (or number of days with any reported symptoms) (Table 4 and Supplementary Table 1d). In winter, NO2 and Ca were significantly associated with the number of days with symptom scores > 1 (NO2: 2.56; 1.02–6.43 and Ca: 2.45; 1.01–5.95). In summer, Cl was significantly and positively associated with days with symptom scores > 1 (1.46; 1.01–2.10). Once again, elemental carbon was negatively associated with this index OR = 0.23 (0.06–0.82). Adjustment for outdoor O3 did not meaningfully change these results (Supplemental Table 1f).
Albuterol use
Results for daily average albuterol use for a given week are shown in Fig. 1b and Tables 4 and 6. In winter, there were significant associations for NO2 (5.89; 1.63–21.26), Ni (2.27; 1.02–5.07), and Si (5.59; 1.01–30.76); however, only NO2 remained significant in the models adjusted for outdoor O3, suggesting significant confounding of these effects by exposure to outdoor O3 (Supplemental Table 2a). No significant associations were found for any pollutant in summer.
Results for our secondary measure of albuterol use defined as the number of days with number of puffs > 0 are shown in Table 4 and Supplemental Table 2b. In winter, there were significant associations for NO2 (8.25; 2.21–30.75), PM2.5 (3.38; 1.04–10.98), PM10 (3.76; 1.12–12.61), and Si (6.07; 1.32–27.83). When adjustments for outdoor O3 were made, associations with PM2.5 and PM10 were no longer significant and those with NO2 and Si increased slightly (Supplemental Table 2c). In summer, no significant associations were noted.
Pulmonary function
No significant associations between either average morning (AM) FEV1 or PEF lability and indoor pollutant exposures were observed in either winter or summer. Results are presented in Table 4 (base models) and Supplemental Tables 3a-d (adjusted for outdoor O3).
Discussion
We observed significant associations between weekly indoor concentrations of several pollutants and respiratory outcomes, including symptom scores and albuterol use, in inner city children with moderate to severe asthma. We found most consistent associations in the winter season with indoor NO2, Si, and Ni for symptoms and albuterol, and in the summer with Cl for symptoms. Ca was also associated with symptoms only in the winter. We did not observe any significant associations with pulmonary function parameters. Taking into consideration our earlier analyses investigating sources of these indoor pollutants (Habre et al. 2014b, Rohr et al. 2014), the significant associations we found for indoor NO2, Si, Ni, Ca, and Cl suggest that indoor pollutants with important contributions from both indoor and outdoor sources might be important for pediatric asthma exacerbation. Additionally, our study contributes findings to the recognized role of seasons in asthma variability and in air pollution associations with asthma (Goldstein 1980).
Multiple prior studies have pointed out the association of NO2 with gas stoves which were present in all of the apartments we studied and were extensively used for cooking and in some cases heating. Water heaters and space heaters have also been identified as principal indoor sources of NO2 (Dedele at al. 2016). Levels of NO2 tend to rise in winter, with decreased ventilation in apartments, as well as the more frequent use of gas stoves for cooking and as a supplement for home heating (Uchiyama et al. 2015). In our earlier source modeling analyses of indoor pollutants in this study (Habre et al. 2014b), we found that cooking was a significant predictor of indoor NO2 levels, followed by outdoor NO2 levels concentrations, confirming that use of gas stoves for cooking and infiltration of outdoor NO2 (associated with traffic and fuel combustion in our study area) contributed to indoor NO2 levels. Recent studies of pediatric asthma severity confirm our observation of the relationship between NO2 exposures and asthma symptom scores and the use rescue medication (Belanger et al. 2013; Lin et al., 2013; Kattan et al. 2007).
Components of indoor PM2.5 of interest in our analysis included Ca, Si, Ni, and Cl. The majority of indoor Ca and Si concentrations were of indoor origin in our earlier analysis, likely related to the resuspension of settled crustal material and dust in these apartments (Habre et al. 2014b; Balasubramanian and Lee, 2007). These elements have also been associated with other indoor sources including cooking, particularly meat (Habre et al. 2014b; Meng et al. 2009; Sexton et al. 1986). Ca can also be emitted from humidifiers (Baxter et al. 2007; Highsmith et al. 1992). Ca is also associated with cigarette smoke (Ozkaynak et al. 1996) and although all of the families studied were composed of non-smokers some of the apartments had high levels of measured nicotine (as discussed by Schachter et al. (2011) using the method of Hammond and Leaderer (1987)). This was attributed to visitors to the apartment and smoking in the hallways or infiltration of secondhand smoke from nearby apartments.
Ni in New York City is a strong tracer of residual fuel oil combustion for building heating and shipping activity in the ports (Kim et al. 2014; Peltier et al. 2009; Peltier and Lippmann, 2010). Concentrations of this element tend to be higher in winter than in summer, specifically in New York City 2.5 times higher (Peltier and Lippmann, 2010), suggesting heating oil and major port operations (Hsu et al. 2012) are major sources. In Rohr et al. (2014), we conducted a source apportionment analysis of daily outdoor PM2.5 pollution in our study area and identified a shipping-related source factor with high loadings of Ni and V. When we analyzed the composition of indoor PM2.5 in our study, we also confirmed indoor Ni in these residences was almost exclusively from outdoor origin (Habre et al. 2014b). Complementing our findings, Patel (Patel and Miller, 2009) reported a significant association between a 3-month averaged inverse distance weighted concentration of ambient Ni and wheeze symptoms in children up to 2 years old in NYC.
Chlorine was the element with the second highest fraction of its concentration of indoor origin in our earlier analysis (Habre et al. 2014b). Chlorine has been associated with bleach-containing cleaning products and the aerosolization of chlorinated municipal water indoors (Zhao et al. 2006; Zhao et al. 2007). Chlorine has also been associated with cooking and environmental tobacco smoke (Habre et al. 2014b; Ozkaynak et al. 1996; Wallace, 1996). In our study, it is associated with higher summer symptom scores even when adjusting for outdoor ozone. While we also found an outdoor source factor with high loadings of Cl (as well as Na) that we labelled “salt” in our outdoor source apportionment work (Rohr et al. 2014), the highest contributions of the outdoor “salt” factor were in the winter time. Taken together, our previous indoor and outdoor source apportionment analyses suggest that the associations we are finding with indoor Cl and symptoms in the summer are related to indoor generation of Cl and not Cl of outdoor origin (related to sea salt from marine air or road salting in the winter). Table 3 shows that indoor Cl levels were lower in the summer compared to the winter in our study. This suggests that it is not the level of indoor Cl that is driving these stronger associations in the summer, but rather, the co-occurrence of other factors or pollutants in the summer that could be leading to indoor Cl having a stronger or larger effect in the summer. This warrants future investigation into possible exposures or behaviors that could be modifying the effect of indoor Cl in the summer.
The negative association between elemental carbon and symptom severity (Table 4) during summer months suggests that this component may be varying inversely with some other pollutant or environmental factor that exacerbates asthma.
Role of season
Positive associations were observed for symptoms in both winter and summer. In winter, NO2 was associated with increased respiratory symptoms. This finding confirms observations reported by many prior studies (Deal Jr. et al., 1979, Lin et al. 2013; Breysse et al. 2010; Fuentes-Leonarte et al. 2009; Heinrich, 2011) and is consistent with the higher indoor NO2 concentrations in winter. In our study, all homes had gas stoves which likely contributed significantly to indoor NO2 concentrations as we described earlier. Ca, Si, and Ni appeared consistently associated with symptoms in winter. Again, this seasonal specificity may reflect higher concentrations of pollutants indoors due to reduced ventilation (closed windows), or in the case of Ca its association with humidifiers. Increased fuel oil burning for heating of residential dwellings lead to increased Ni concentrations in winter. In summer, the association between Cl and symptoms warrants further investigation as described earlier.
No associations were noted for the albuterol parameters in summer, but in winter NO2 and to a lesser extent Ca, Si, and Ni were associated with albuterol use. This association with medication use may reflect similar sources and patterns as noted above for symptoms.
Overall, indoor NO2, Si, and Ni were the only three pollutants associated with both more subjective (symptoms) and somewhat objective (albuterol use) asthma symptoms, despite both of these outcomes being collected via self-report in a diary. This highlights the consistency of these findings.
In a prior analysis (Grunin et al. 2010), we analyzed the potential role of allergens collected in dust samples of these homes (mouse and cockroach) on their potential modifying role for modifying the relationship between pollutant and symptom severity by season. In that study, we did not observe any significant modification.
Ozone-adjusted models
In our previous analysis of the role of outdoor pollution in asthma exacerbation (Schachter et al. 2016), outdoor O3 concentrations were associated with increased symptom severity and albuterol use as were outdoor concentrations of PM10 and PM2.5 and a number of their components. In summer adjustment for outdoor O3 concentration resulted in loss of significance for the association of outdoor particulate matter and its components. In winter, by contrast, adjustment for outdoor O3 had only limited effect on the association with outdoor PM. Because of the documented role played by outdoor ozone in asthma exacerbation, we controlled for outdoor O3 in the analyses reported herein of indoor pollutants. In contrast to outdoor pollutants, adjustment for outdoor O3 concentrations had a limited impact on the associations between indoor pollutants and effects on symptoms in either season, possibly because indoor concentrations are more representative of true personal exposures given the large amount of time children tend to spend at home. In the case of primary and secondary symptom parameters, all the associations remained statistically significant when adjustment for O3 was made. For albuterol use on the other hand, significant associations in winter were lost for Ni and Si when the measure used was average daily albuterol use. When the measure for albuterol use was number of days when albuterol use was > 0, a change was seen with only the PM2.5 association losing significance in winter after O3 adjustment. This limited effect is not surprising given the lower outdoor O3 levels in winter, and our inability to find significant effect of ambient O3 on respiratory health in this season (Schachter et al. 2016). In summer, indoor O3 levels were not associated with health effects and outdoor O3 had no effect on the association of chlorine with asthma symptoms.
p values and multiple comparisons
Concern in the statistical literature has been raised about the use of p values and the excessive emphasis placed on interpreting them. The use of an arbitrary cutoff for significance must interpreted with care in determining the presence and importance of clinical effects (Wasserstein and Lazar, 2016, Wasserstein et al. 2019). In particular, multiple comparisons increase the likelihood that some of the “significant” associations calculated in this study have occurred by chance alone (Harrington and D’Agostino Sr, 2019). Considering a more stringent p value significant cutoff of < 0.01, only summer associations of indoor Cl with average or maximum symptoms scores are considered significant, even after adjusting for outdoor O3, and winter associations of indoor NO2 with average albuterol use and with days of albuterol use. However, only indoor NO2 and days of albuterol use remains significant at p value < 0.01 after adjusting for outdoor O3. The plausibility of our findings is however enhanced by the similarities noted with other studies and the consistency noted in the pattern of the effects across variations of the indices of asthma severity.
Conclusions
NO2 and PM2.5 elements—in particular, Ca, Si, Ni, and Cl—were associated in this study with aggravated asthma symptoms and the increased use of rescue medication among inner city children with moderate to severe asthma. Indoor pollutant levels were more likely to be associated with these clinical indices in winter than in summer, a season in which asthma exacerbations tend to be more frequent, with the exception of Cl. The elements and gases associated with asthma exacerbation suggest potential indoor and outdoor sources. The associations were relatively independent of the way in which the three symptom indices and the two albuterol measures were defined.
References
Balasubramanian R, Lee SS (2007) Characteristics of indoor aerosols in residential homes in urban locations: a case study in Singapore. J Air Waste Manage Assoc 57(8):981–990
Baxter LK, Clougherty JE, Laden F, Levy JI (2007) Predictors of concentrations of nitrogen dioxide, fine particulate matter, and particle constituents inside of lower socioeconomic status urban homes. 17(5):433–444
Belanger K, Holford TR, Gent JF, Hill ME, Kezik JM, Leaderer B (2013) Household levels of nitrogen dioxide and pediatric asthma severity. Epidemiology 24(2):320–330
Bielroy L, Deener A (1998) Seasonal variation in the effects of major indoor and outdoor environmental variables on asthma. J Asthma 35(1):7–48
Breysse PN, Diette GB, Matsui EC, Butz AM, Hansel NN, McCormack MC (2010) Indoor air pollution and asthma in children. Proc Am Thorac Soc 7(2):102–106
Deal EC Jr, McFadden ER Jr, Ingram RH Jr, Strauss RH, Jaeger JJ (1979) Role of respiratory heat exchange in production of exercise-induced asthma. J Appl Phys 46(3):467–475
Delfino RJ, Gong H Jr, Linn WS, Pellizzari ED, Hu Y (2003) Asthma symptoms in Hispanic children and daily ambient exposures to toxic and criteria air pollutants. Environ Health Perspect 111:647–656
Demokritou P, Kavouras IG, Harrison D, Koutrakis P (2001) Development and evaluation of an impactor for a PM2.5 speciation sampler. J Air Waste Manage Assoc 51(4):514–523
Franklin PJ (2007) Indoor air quality and respiratory health of children. Paediatr Respir Rev 8:281–286 https://www.ncbi.nlm.nih.gov/pubmed/18005895
Fuentes-Leonarte V, Tenías JM, Ballester F (2009) Levels of pollutants in indoor air and respiratory health in preschool children: a systematic review. Pediatr Pulmonol 44(3):231–243
Gielen MH, Van Der Zee SC, Van Wijnen JH, Van Steen C, Brunekeef B (1997) Acute effects of summer air pollution on respiratory health of asthmatic children. Am J Respir Crit Care Med 155:2105–2108
Goldstein I (1980) Weather patterns and asthma epidemics in New York City and New Orleans, USA. Intl J Biometeriol 24(4):329–339
Grunin A, Habre R, Castro W et al (2010): Can no2, ozone, or allergens modify PM2.5’s effect on airway symptoms? https://doi.org/10.1164/ajrccm-conference.2010.181.1_MeetingAbstracts.A4624
Habre R, Moshier E, Castro W, Nath A, Grunalin A, Rohr A et al (2014a) The effects of PM2.5 of outdoor and indoor origin and ozone on 1 cough and wheeze symptoms in asthmatic children. J Expo Sci Environ Epidemiol 24:380–387
Habre R, Coull B, Moshier E, Godbold J, Grunin A, Nath A et al (2014b) Sources of indoor air pollution in New York City residences of asthmatic children. J Expo Sci Environ Epidemiol 24:269–278
Hammond SK, Leaderer BP (1987) A diffusion monitor to measure exposure to passive smoking. Environ Sci Technol 21:494–497
Hankinson JL, Odencranz JR, Fedan KB (1999) Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med 159:179–187
Harrington D, D’Agostino RB Sr, Gatsonis C et al (2019) New guidelines for statistical reporting in the journal. N Engl J Med 381:285–286
Heinrich J (2011) Influence of indoor factors in dwellings on the development of childhood asthma. Int J Hyg Environ Health 214(1):1–25
Highsmith VR, Hardy RJ, Costa DL, Germani MS (1992) Physical and chemical characterization of indoor aerosols resulting from the use of tap water in portable home humidifiers. Environ Sci Technol 26(4):673–680
Hsu SI, Ito K, Kendall M, Lippmann M (2012) Factors affecting personal exposure to thoracic and fine particles and their components. J Expo Sci Eviron Epidemiol 22(5):439–447
Iskandar A, Andersen ZJ, Bønnelykke K, Ellermann T, Andersen KK, Bisgaard H (2012) Coarse and fine particles but not ultrafine particles in urban air trigger hospital admission for asthma in children. Thorax 67:252–257
Kattan M, Mitchell H, Eggleston P, Gergen P, Crain E, Redline S et al (1997) Characteristics of inner-city children with asthma: the National Cooperative Inner-City Asthma Study. Pediatr Pulmonol 24(4):253–262
Kattan M, Gergen PJ, Eggleston P, Visness CM, Mitchell HE (2007) Health effects of indoor nitrogen dioxide and passive smoking on urban asthmatic children. J Allergy Clin Immunol 120(3):618–624
Kim K, Shon Z, Mauuloida PT, Song S (2014) Long term monitoring of airborne nickel (Ni) pollution in association with some potential source processes in the urban environment. Chemosphere 111:312–319
Larsen GL, Beskid C, Shirnamé-Moré L (2002) Environmental air toxics: role in asthma occurrence? Environ Health Perspect 110(Suppl 4):501–504
Lin W, Brunekreef B, Gehring U (2013) Meta-analysis of the effects of indoor nitrogen dioxide and gas cooking on asthma and wheeze in children. Int J Epidemiol 42(6):1724–1723
Liu L, Box M, Kalman D, Kaufman J, Koenig J, Larson T et al (2003) Exposure assessment of particulate matter for susceptible populations in Seattle. Environ Health Perspect 111:909–918
Meng QY, Spector D, Colome S, Turpin B (2009) Determinants of indoor and personal exposure to PM2.5 of indoor and outdoor origin during the RIOPA Study. Atmos Environ 43(36):5750–5758
Ozkaynak H, Xue J, Spengler J, Wallace L, Pellizzari E, Jenkins P (1996) Personal exposure to airborne particles and metals: results from the Particle TEAM study in Riverside, California. J Expo Anal Environ Epidemiol 6(1):57–78
Patel MM, Miller RL (2009) Air pollution and child hood asthma recent advances and future directions. Curr Opin Pediatr 21:235–243
Peltier RE, Lippmann M (2010) Residual oil combustion: 2. Distributions of airborne nickel and vanadium within New York City. J Expo Sci Environ Epidemiol 20(4):342–350
Peltier RE, Hsu SI, Lall R, Lippmann M (2009) Residual oil combustion: a major source of airborne nickel in New York City. J Expo Sci Environ Epidemiol 19(6):603–612
Peters A, Dockery DW, Heinrich J, Wichmann HE (1997) Short-term effects of particulate air pollution on respiratory morbidity in asthmatic children. Eur Respir J 10:872–879
Rohr AC, Habre R, Godbold J, Moshier E, Schachter N, Kattan M et al (2014) Asthma exacerbation is associated with particulate matter source factors in children in New York City. Air Qual Atmos Health 7(2):239–250
Roy A, Sheffield P, Wong K, Trasande L (2011) The effects of outdoor air pollutants on the costs of pediatric asthma hospitalizations in the United States, 1999 to 2007. Med Care 49:810–817
Sarnat J, Brown K, Schwartz J, Coull B, Koutrakis P (2005) Ambient gas concentrations and personal particulate matter exposures- implications for studying the health effects of particles. Epidemiology 16:385–395
Schachter EN, Castro W, Perrino C, Nath A, Grunin A, Habre R et al (2011) Is a smoke free home really smoke free? Am J Respir Crit Care Med 183:Abstract 4029
Schachter EN, Moshier E, Habre R, Rohr A, Godbold J, Nath A et al (2016) Outdoor air pollution and health effects in urban children with moderate to severe asthma. Air Qual Atmos Health 9:251–263
Schwab M, McDermott A, Spengler JD (1992) Using longitudinal data to understand children’s activity patterns in an exposure context: data from the Kanawha County Health Study. Environ Health Perspect 18:173–189
Selgrade MK, Lemanske RF Jr, Gilmour MI, Neas LM, Ward MD, Henneberger PK et al (2006) Induction of asthma and the environment: what we know and need to know. Environ Health Perspect 114:615–661
Sexton K, Webber L, Hayward S, Sextro R (1986) Characterization of particle composition, organic vapor constituents and mutagenicity of indoor air pollutant emissions. Environ Int 12:351–362
Uchiyama S, Tomizawa T, Tokoro A, Aoki M et al (2015) Gaseous and chemical compounds in indoor and outdoor air of 602 houses throughout Japan in winter and summer. Environ Res 137:364–372
Vedal S, Petkau J, White R, Blair J (1998) Acute effects of ambient inhalable particulates in asthmatic and non-asthmatic children. Am J Respir Crit Care Med 157:1034–1043
Wallace L (1996) Indoor particles: a review. J Air Waste Manage Assoc 46:98–126
Wang X, Dockery DW, Wypij D, Fay ME, Ferris BG (1993) Pulmonary function between 6 and 18 years of age. Pediatr Pulmonol 15:75–88
Wang LY, Zhong Y, Wheeler L (2005) Direct and indirect costs of asthma in school age children. Prev Chronic Dis 2:1–10
Wanger J, Clausen JL, Coates A, Pedersen OF, Brusasco V, Burgos F et al (2005) Standardization of the measurement of lung volumes. Eur Respir J 26:511–522
Wasserstein RL, Lazar NA (2016) The ASA’s statement on p-values: context, process and purpose. Am Stat 70:129–133
Wasserstein RL, Schirm AL, Lazar NA (2019) Moving to a world beyond “p<0.05”. Am Stat 73(Supp):1–19
Zhao W, Hopke PK, Norris G, Williams R, Paatero P (2006) Source apportionment and analysis on ambient and personal exposure samples with a combined receptor model and an adaptive blank estimation strategy. Atmos Environ 40:3788–3801
Zhao W, Hopke PK, Gelfand EW, Rabinovitch N (2007) Use of an expanded receptor model for personal exposure analysis in schoolchildren with asthma. Atmos Environ 41:4084–4096
Acknowledgments
The authors would like to thank Tom Gentile, George O’Connor, and Lance Wallace, members of the CAPAS study scientific advisory committee, for their guidance in all phases of the study. Steve Ferguson and Mike Wolfson are also acknowledged for designing the air sampling monitors and conducting laboratory analyses. We thank Dr. Fred Moshary of CCNY for sharing his facilities. The authors would also like to thank all the individuals who participated in the study.
Funding
This study was supported by the Electric Power Research Institute (EP-P15909/C7932).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Rohr is employed by the Electric Power Research Institute (EPRI) which is primarily supported by the electric power industry in the USA and abroad. EPRI is a 501(c)(3) organization that funds external research at a number of universities and institutes worldwide. Other authors declare no conflict of interest personal, financial, or otherwise with the material presented in this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schachter, E.N., Rohr, A., Habre, R. et al. Indoor air pollution and respiratory health effects in inner city children with moderate to severe asthma. Air Qual Atmos Health 13, 247–257 (2020). https://doi.org/10.1007/s11869-019-00789-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11869-019-00789-3