Abstract
Accountability of air quality management is often measured by tracking ambient pollution concentrations over time. These changes in ambient air quality are rarely linked to changes in public health, a major driver for such programs. We propose a method to assess the accountability of air quality management programs with respect to improvements in public health by estimating national temporal trends in health risk attributable to air pollution. The air health indicator (AHI) is a function of two temporal functions, annual air pollutant concentrations and annual estimates of health risk obtained by time series statistical methods, to indicate the trend in annual percent attributable risk (the product of concentration and risk times 100). Random effects models are used to obtain a distribution of risk over space. The model is illustrated by examining the association between daily nonaccidental deaths in 24 of Canada’s largest cities and daily concentrations of ozone and nitrogen dioxide over the 17-year period 1984–2000. Our analysis demonstrates that examining trends in exposure alone, which has typically been the approach to air quality indicators, provides an incomplete picture of trends in the impact of air pollution. The AHI appears to provide a more informative measure of the population burden of illness associated with air pollution over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Canadian government has initiated a program to monitor the quality of the environment as one predictor of social and economic well-being. One way to assess environmental quality is to use indicators that convey complex information in a simple form. Canadian Environmental Sustainability Indicators (CESI) provides an indication of the health of our environment in much the same way as the gross domestic product, and other signals provide a sense of the health of the economy. CESI has three components: air quality, fresh water quality, and greenhouse gas emissions. Spatial–temporal trends in these components are reported annually (CESI 2006). Social, economic, and climatic factors are examined in order to understand the causes of observed spatial and temporal variations. Each successive reporting year is based on an additional year of monitoring data.
The air quality component of the CESI measures the April to September mean concentrations of ozone and fine particulate matter averaged over all monitors within a community and then population-weighted averaged over all communities. As of the 2007 report, April to September averages for ozone were reported from 1990 to 2005 while April to September averages of fine particulate matter were reported for the 2000 to 2005 time period. A nonparametric statistical test for monotonic trend in the annual averages is presented (Sen 1968)). Annual averages are also reported by region of the country.
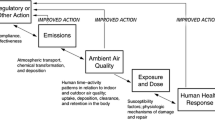
When more stringent air quality standards are set and subsequently met, it is implicitly assumed there will be some improvement in public health (USEPA 1997; De Civita et al. 1999). Such improvements in public health are rarely verified other than in a few isolated cases where a particular event or regulatory intervention resulted in a sharp, sometimes temporary, drop in air pollution. (Clancy et al. 2002; Friedman et al. 2001; Hedley et al. 2002; Pope 1989). In its recent monograph, the Health Effects Institute defined accountability as part of “a broad effort to assess the performance of… environmental regulatory policies” (Health Effects Institute 2003). Applied specifically to the area of air quality, this involves determining whether policies have actually resulted in the anticipated improvements in public health. The primary motivation for evaluating accountability is to be able to guide air quality policies based on evidence of their effectiveness and secondarily to demonstrate that investments to improve air quality have been warranted based on benefits to public health. There are numerous challenges in attempting to document improvements in public health as a consequence of air quality policies. These primarily relate to factors which confound or obscure the causal pathway between introduction of a regulation or policy to changes in emissions, exposure and dose, and finally health status. These factors include potential impacts of the policy on personal behaviour or economic activity which could also affect health, changes over the same time scale as the regulation in factors which also affect the health outcomes of interest, incomplete or delayed implementation of a regulation or policy, or along the time delay between changes in exposure and changes in the frequency of effects. If the relationship between concentrations of ambient air pollution and various health outcomes, such as mortality and hospital admissions, remains constant over time, then there would be little need to verify if improvements in air quality do in fact translate into improvements in public health. However, the relationship between outdoor air pollution and health can change over time and space for several reasons (Shin et al. 2008). First, the nature and extent of the at-risk population may change over time (e.g., through an aging population, changes in prevalence of health conditions) and may also vary across the country due to spatial–temporal variation in population demographics and disease status. Second, some measured ambient air pollutants may act as markers for the truly toxic but unmeasured atmospheric constituents. For example, particulate mass, a pollutant often linked to health, is composed of hundreds of chemical compounds, whose concentrations can vary dramatically over both space and time. Strategies to reduce the particulate phase of the mixture may reduce mass but not proportionately reduce the toxicity of the atmospheric mixture. Third, the shape of the concentration–response relationship may not be linear, and thus, changes in the distribution of exposures over time may lead to changes in the estimate of risk when such estimates are based on the commonly employed linear association between concentration and response. Finally, the relationship between measurements of pollution from fixed-site outdoor monitors and the exposure metric of most interest (i.e., population-average personal exposure) may also vary over space and time arising from changes in monitor location over decades, within and between community changes in population density, housing stock, air conditioning use, and time activity patterns. It is therefore of interest to be able to track changes in the relationship between outdoor air pollution in urban environments and health in both space and in time.
Several studies have used spatial variation in risk (between cities) to identify factors that modify risk, such as percent of homes in a city with air conditioning. We can also use time as a means of generating additional variation in risk estimates in order to understand what factors influence the relationship between exposure and health outcomes. There have been several studies linking daily variations in urban air pollution and daily variations in the number of deaths within a city throughout the world (Dominici et al. 2000, 2002; Stieb et al. 2002). Some countries maintain mortality records, thus providing a resource to routinely track an important aspect of adverse health risks associated with air pollution. Computerized records of admissions to hospital for all ages are also available and have been linked to air quality in Canada (Burnett et al. 1994, 1997, 1999, 2001; Lin et al. 2002). Hospital admissions indicating the number of patients admitted into hospitals are a marker for an adverse health event (Delfino et al. 1997; Burnett et al. 1995). One is interested in reducing the number of adverse events, not simply admissions to hospital. The fact of being admitted to a hospital can be influenced by a number of factors including the role the hospital plays in health care delivery. This role may be changing over time in Canada. For example, hospital admissions for asthma among those 0–24 years of age have declined by approximately one half between 1987 and 2004. This has been attributed to both improved medical care and reduced availability of hospital beds (PHAC 2007). Declines in age-adjusted hospital admission rates for cardiovascular disease have also been reported (Johansen et al. 2005). This issue is not as much a concern for emergency room visits because everyone who visits the emergency room is examined, and a record is created for that visit. Potentially changing patterns of how Canadians obtain their health care, such as increases in walk-in clinics, can also influence emergency room visit frequencies. Unfortunately, Canada does not have a centralized computerized emergency room record system, so universal coverage of this outcome is not currently available.
Our approach to estimating risk over space and time is illustrated by the case of the association between two pollutants shown to be related to mortality in Canadian cities (Burnett et al. 2004), nitrogen dioxide and ground level ozone, and nonaccidental mortality in 24 of Canada’s largest cities over the 17-year period from 1984 to 2000.
Air health indicator to monitor temporal trends in health risk
Air health indicator
Poor air quality negatively affects human health. Most specifically, air pollution affects heart and lung diseases. The health effects associated with poor air quality contribute to lost productivity, emergency room and hospital admissions, and mortality. The air health indicator (AHI) has been developed to monitor the trend over time in the percentage of daily mortalities resulting from exposure to air pollution. The AHI incorporates information on air pollutant concentrations and public health outcomes (e.g., daily hospital admissions or mortality), in order to identify which air pollutants are associated with health risks, and to track the effectiveness of air quality management actions at reducing adverse health effects on the population.
The AHI is a function of two temporal functions, annual air pollutant concentrations, and annual risks of the air pollutant, to indicate the trend in annual attributable risks (AR) defined as follows:
where C j and β j represents annual air pollution concentration and its risk, respectively, for year j. Air pollutant concentration is measured by monitoring stations, and risk is estimated by model. The outputs from our model, which will be discussed in the next section, are the annual pooled risk estimates and the annual city-specific shrunk estimates. The AR measures the percentage of daily mortality attributable to population exposure to the air pollutant.
The AHI provides information in terms of the slope that indicates the extent of incline or decline in the attributable health risk estimates over time if there exists a time trend. SEN’s method (Sen 1968), a nonparametric statistical test for monotonic trend, is a good tool for this purpose shown below.
The test result indicates compatibility with our proposed model; whether or not there has been an increasing, decreasing, or no trend in those annual risk estimates. Using the AHI, we are able to assess the accountability of air quality management programs with respect to improvements in public health as well as in air pollution concentration.
For example, an ozone air health indicator can establish a relationship between warm season ozone concentration and mortality due to heart (heart attacks, heart failure), vascular (stroke), and respiratory (pneumonia, bronchitis) causes.
Spatial–temporal model for risk of air pollution
The number of daily nonaccidental deaths was selected as the response variable reflecting the adverse short-term health effects from air pollution. To measure the association between short-term exposure to ambient air pollution and death, we consider a time series of the counts of daily deaths on day t within community i, Y i (t), and the corresponding concentration of an ambient air pollutant, x i (t). A Poisson regression model applied to the counts can be simplified as
The unknown parameter β i (t) represents the unit log-relative risk at time t for community i. The focus of our analysis is to model how risk varies over time and between communities. Since we are most interested in changes in risk over time periods on the order of years, we will assume the risk is constant within each calendar year. Temporal structure of risk can be therefore simplified as β i (t) = β ij for all t in the jth calendar year.
We consider three factors as potential confounding variables: calendar time; temperature; and indicators for days of the week (DOW). Time is included to control both temporal and seasonal variations, daily temperature controls for the short-term effect of weather on daily mortality, and day of the week accounts for variation in mortality and air pollution by day of the week. Daily counts of mortality are assumed to depend on time and temperature in a nonlinear fashion and on air pollution in a linear manner. To be consistent with the CESI reporting of ambient air pollution trends, we based our temporal–spatial risk estimator on the data for each city and year. The estimation procedure has two stages. City- and year-specific estimates \(\hat \beta _{ij} \) are obtained from an over-dispersed Poisson time series model in addition to estimates of their error variances \(\hat v_{ij} \)(Ramsay et al. 2003). We note that other estimation approaches can be considered in the first stage, such as case-crossover (Lin et al. 2002) or generalized linear mixed models (Szysykowicz 2006).
In the second stage, we consider a random effects model of the form:
where δ ij is an independent random variable with mean 0 and variance \(\sigma _\beta ^2 \left( j \right)\). This is a random effect model with the parameters fluctuating randomly around their mean μ β (j). The error term e ij is an independent random variable with zero expectation and variance \(\hat v_{ij} \) which is assumed known. The estimates \(\hat \beta _{ij} \) are assumed to be normally distributed with a common mean, μ β (j) and the variance modeled by the sum of two variances: the within community estimation variance, v ij , and between community variance indicating the heterogeneity of the true risks among cities, \(\sigma _\beta ^2 \left( j \right)\). Bayesian methods are used to obtain estimates of the distribution of risk among the communities annually, with expectation \(\hat \mu _\beta \left( j \right)\) and variance \(\hat \sigma _\beta ^2 \left( j \right)\) (Dominici et al. 2000). An estimate of the city-specific risk, \(\tilde \beta _{ij} \) say, under the random effects model is also obtained. Since this estimate is always closer to \(\hat \mu _\beta \left( j \right)\) than \(\hat \beta _{ij} \), it is termed a “shrinkage” estimator. If the estimate of the heterogeneity among cities is zero, i.e., \(\hat \sigma _\beta ^2 \left( j \right) = 0\), then the “best” estimate of risk for any community is the common risk estimate, i.e., \(\hat \mu _\beta \left( j \right)\). The larger the estimate of heterogeneity in risk (\(\hat \sigma _\beta ^2 \left( j \right)\)) compared to the within community error estimate (\(\hat \nu _{ij} \)), the closer the shrinkage estimator \(\tilde \beta _{ij} \) will be to the estimator of risk based solely on information from that city \(\hat \beta _{ij} \). Although the shrinkage estimators are biased, they have smaller variances than \(\hat \beta _{ij} \), thus providing more stable estimates. We are thus borrowing strength from all the communities to estimate risk for each specific community. This is particularly useful when examining smaller communities which inherently have large uncertainties with respect to their estimates of risk.
The estimate of heterogeneity in risk among cities is highly unstable over time (Shin et al. 2008). While the pooled risk estimates are relatively insensitive to this instability, the city-specific shrinkage estimates are not. We, therefore, use a common value of \(\hat \sigma _\beta ^2 \) for determining both the pooled annual risk and the city-specific annual shrunk risks. This common value is defined as the median of the annual estimates of \(\sigma _\beta ^2 \) over the entire time period of observation. The same number of observations (usually 365 days) are used to estimate both v ij and \(\sigma _\beta ^2 \).
Illustrative example
Daily variations in nonaccidental mortality in Canadian cities have been shown to be related to daily variations in both concentrations of ozone and nitrogen dioxide (Burnett et al. 2004). We illustrate our spatial–temporal model of risk using these pollutants. We consider the daily 8-h running maximum as the summary measure of population average exposure for ozone, since it is the metric employed for the Canada-Wide Ozone Standard (CCME 2000). The daily average concentration is used for nitrogen dioxide (NO2). We selected communities with a reasonably long time series of both pollutants, resulting in 24 Canadian cities having information from 1984 to 2000, the last year of nationally available mortality data. The cities span the geographic breadth of the country. The time series model comprises a natural spline term in the model for time with 9 df/year, two natural spline terms for daily average temperature with 3 df recorded on the day of and the day prior to death, indicator functions for the day of the week, and a linear term for the 2-day average of pollution concentrations.
The trivariate components for the AHI are presented in Fig. 1 for ozone. There is some evidence that ozone concentrations have increased over the time period (p = 0.0435) from 1984 to 2000 with a slope of 0.174 ppb/year and 95% confidence interval (CI) of (0.008, 0.346). This corresponds to a 10.8% increase in concentrations over the observation period. However, there is little evidence (p = 0.4338) that risk changes over time with a median slope of −1.96 × 10−5 and 95% CI of (−7.57 × 10−5, 2.82 × 10−5) log-mortality rate/ppb per year. There is also little evidence (p = 0.5367) that the percent attributable risk changes over time with a median slope of −0.033%/ppb per year with 95% CI of (−0.194, 0.114).
Annual average concentrations of ozone (daily 8-h maximum) over 24 Canadian cities with trend line (top panel, p = 0.0435), annual ozone-mortality unit risk × 100 and trend line (middle panel, p = 0.4338), percent attributable risk—product of concentration and risk × 100—and trend line (bottom panel, p = 0.5367)
The equivalent information is presented in Fig. 2 for nitrogen dioxide (three left-hand panels). Nitrogen dioxide concentrations have clearly declined over time (p < 0.0001) with a median slope of −0.275 ppb/year and 95% CI of (−0.382, −0.236) corresponding to a 20.1% decline in concentrations over the entire time period. However, there is some evidence to suggest (p = 0.1275) that risk has increased over time with a median slope of 4.180 × 10−5 log-mortality rate/ppb per year and 95% CI of (−2.033 × 10−5, 10.207 × 10−5). The percent attributable risk also has increased with a median slope of 0.046%/ppb per year and 95% CI of (−0.087, 0.160), but the evidence for this assertion is weak (p = 0.4840).
Annual average concentrations of NO2 (daily mean) over 24 Canadian cities with trend line (top left panel, p < 0.0001), annual NO2-mortality unit risk × 100 and trend line (middle left panel, p = 0.1275), percent attributable risk—product of concentration and risk × 100—and trend line (bottom left panel, p = 0.4840). Right panels are corresponding plots excluding the data for 1998. Annual average NO2 with trend line (top right panel, p < 0.0001), annual NO2-mortality unit risk × 100 with trend line (middle right panel, p = 0.0274), percent attributable with trend line (bottom right panel, p = 0.1917)
We note the unusually low-risk estimate for nitrogen dioxide estimated in 1998. Reasons for this lower risk value are unclear but are neither due to the time series model formulation (degrees of freedom for the nonlinear terms) nor the distribution of weather or air pollution concentrations. The trivariate components of the AHI were calculated excluding the information from 1998 (three right-hand panels of Fig. 2). The median slope in concentration was insensitive to this single year exclusion (median slope of −0.296 ppb/year with 95% CI of (−0.411, −0.255)) since the NO2 concentrations in 1998 were not unusual. Exclusion of 1998 information, however, increased the slope in risk from 4.180 × 10−5 log-mortality rate/ppb per year to 6.419 × 10−5 log-mortality rate/ppb per year with 95% CI of (0.878 × 10−5, 11.519 × 10−5) with much stronger evidence of a positive median slope (p = 0.0274). Sixteen additional models of risk were fit each excluding a single year of information. The risk trend line was most sensitive to the exclusion of 1998. The percent attributable risk median slope was 0.0839%/ppb per year with 95% CI of (−0.035, 0.0209) with weak evidence of a nonzero trend (p = 0.1917).
Information concerning the distribution of risk and time trend among cities can be visualized by plotting the time trend slope versus the shrunk risk among cities. This information is displayed in Fig. 3 for ozone (top panel) and nitrogen dioxide (bottom panel) to illustrate this analysis feature. The trend line of the shrunk risks is plotted against the median of the annual shrunk risks by city. Most trend lines are negative (y-axis) except for very small positive slopes for Niagara and Winnipeg for ozone, and positive for nitrogen dioxide, except for a very small negative slope for Hamilton. For both pollutants, the shrunk risks (x-axis) are all positive with about a twofold variation among cities.
City-specific median trend line (y-axis) of shrunk risks and median of annual city-specific shrunk risks (x-axis) for ozone (top panel) and nitrogen dioxide (bottom panel). City names indicated on plot. Pooled risk estimate represented by vertical dashed line and pooled linear trend estimate represented by horizontal dashed line
The amount of shrinkage of risk is illustrated in the top two panels of Fig. 4 which display the relationship between the estimates of the city-specific risks \(\hat \beta _{ij} \) and the shrunk risks \(\tilde \beta _{ij} \) by connecting the two estimates each year by a line with an arrow pointing in the direction of the pooled risk (solid line). The top left hand panel is for Toronto, Canada’s largest metropolitan community, and the top right hand panel is for Regina, a relatively small Canadian city. It is evident from these graphs that there is considerably more shrinkage of risk in the smaller community.
City-specific ozone risks and shrunk risks (connected by arrowed line), and pooled risk (solid line) for Toronto (upper left hand panel) and Regina (upper right hand panel). Ozone median time trend slope of city-specific shrunk risks (solid line), shrunk risks (points), and pooled time trend line (dashed line) for Winnipeg (middle left hand panel), Ottawa (middle right hand panel), Quebec (lower left hand panel), and York (lower right hand panel)
The middle and bottom two panels in Fig. 4 display the shrunk risks annually (points), the city-specific trend line (solid line) and the pooled trend line (dashed line) for Winnipeg (middle left hand panel), Ottawa (middle right hand panel), Quebec (bottom left hand panel), and York (bottom right hand panel). These four cities were selected based on their relatively extreme values of either the trend line or shrunk risk visualized in Fig. 3. First, there is considerable variation in the shrunk risks over time in each city. Second, although these cities represent the extremes in trend and risk, it is not clear that there is any real difference in either trend or risk between these cites or from the pooled estimates. Formal statistical tests confirm that none of the cities show any evidence that their trend lines or shrunk risks are different from their pooled counterparts (p > 0.2). Similar statistical tests on the nitrogen dioxide data lead to the same conclusions as that for ozone.
Discussion
In this paper, we propose a new method to estimate the association between daily variations in ambient air pollution and daily fluctuations in nonaccidental mortality over space and time. Spatial-temporal risk estimates, coupled with city-specific and national estimates in trends in air pollution, can be used to assess whether the adverse effect of air pollution related to mortality have changed over time.
We observed statistically significant changes in exposure to both ozone and nitrogen dioxide over time, although the magnitude of these changes was modest. Conversely, we observed much larger proportional changes in risk over time, but these were generally not statistically significant. This phenomenon results from low predictive power of air pollution to explain mortality translated into high uncertainty in estimates for both risk and trend over time. The trend in the product of exposure and risk was dominated by the trend in risk due to the larger variation in risk over time comparing to air pollution concentration. While this phenomenon is in fact simply a reflection of the data, it may be possible to equalize the impact of each element of the AHI by, e.g., normalizing the trend in each element prior to calculating the product. These findings also illustrate the value from the point of view of accountability, of evaluating trends in attributable risk in addition to the customary approach of examining solely trends in ambient air pollution concentrations. If the goal of regulatory efforts to control air pollution is to improve public health, then examining trends in ambient air pollution alone does not address this goal and, in fact, provides potentially misleading guidance on the effectiveness of air pollution controls,
Within the Bayesian modeling framework, city-specific estimates of risk and the time trend in risk can be obtained. The observed total variance among the city-specific risk estimates is quite small, and thus the estimate for heterogeneity among the cities often resulted in zero. Bayesian approach using MCMC enables estimation of the heterogeneity. Cities can then be identified which display unusual spatial–temporal patterns in risk. As seen in the previous section of example, the clear decline in NO2 concentrations in Canada has not translated into health benefits as measured by mortality. This may be due to the fact that NO2 is a marker of combustion for many sources and that the true toxic components of combustion have not declined at the same rate as NO2. Attempts to explain these patterns can be made in the second stage of the two-stage modeling approach. Here, the annual average community-specific risk estimates will be considered as the dependent variable and regressed on potential predictors of risk (community health status, air conditioning use, particle phase constituents, demographics, and measures of social welfare) within a Bayesian modeling framework over time and space. Nonlinear models of air pollution association with mortality can also be considered. Risk may be also summarized by region of the country. The second stage model would contain two levels of clustering: city within region and region within the country. Trend estimates could then be obtained for the country and each region.
We are also interested in the longer-term exposure effects on mortality. These effects are usually determined by examining cohorts of subjects followed over time in selected communities or neighborhoods with varying long-term air pollution concentrations (Pope et al. 2004; Rabl 2006). A dynamic risk model could be postulated including a time–air pollution interaction. However, due to the potential confounding of risk with age, a single static cohort cannot be used. In addition, ultimately all members of the cohort will die and thus time trends cannot be continually determined.
Health Canada is currently examining the effects of longer-term outdoor pollution on longevity by using a cohort determined from linking income tax records to vital status and cancer incidence. A pilot study is underway in which over 600,000 residents of ten Ontario communities have had their income tax records linked to both vital status and cancer incidence since the mid-1980s. Tax records report a subject’s address, age, gender, marital status, and income annually.
This income tax cohort can be dynamic in nature with all new filings included each year. There is no time restriction on the monitoring of this type of cohort. The time–air pollution interaction can then be used as an estimator of temporal changes in risk. Careful attention must be paid, however, to the changing age–gender distribution of tax filers over time.
We have chosen not to include in the AHI an estimate of the number of people whose lives would have been lengthened, on average, if air quality would have been improved. Although such calculations have been made for longer-term exposure metrics in Canada (Coyle et al. 2003) using risks based on cohort studies (Krewski et al. 2003), they have not been attempted for risks based on time series studies for methodological reasons. The time series studies do not necessarily measure risk to individuals in the same manner as they do in cohort studies. Time series risks can be used in a similar manner to that of the cohort study-based risks if one assumes that all members under study (in the time series case the entire population) have the same baseline hazard function and the same air pollution risk estimate at any given age (Miller and Armstrong 2001; Burnett et al. 2003; Rabl 2006). However, it is known that air pollution risk can vary by underlying disease status (Goldberg et al. 2005) and by age.
It is not possible to determine an individual’s risk or baseline hazard function and thus not possible to determine the true joint distribution of these quantities. However, we can estimate underlying hazard functions and risk for specific subgroups of the population. For example, Goldberg et al. (2005) have established a dynamic population study in the city of Montreal, Canada. All interactions with the provincial health care system for subjects over 65 years of age are recorded and linked to the individual over time, such as doctors’ billings, emergency visits, and hospital admissions, drug prescriptions, clinic visits, and vital status. The population can then be divided by presence of one or more chronic diseases. Time series of deaths for all nonaccidental causes can then be created for each subgroup and linked to air pollution using time series statistical methods. Thus, a disease-specific risk can be determined. The total attributable risk (sum of disease specific risk times number of daily nonaccidental deaths in that disease group) can be compared to the equivalent quantity based on the total number of nonaccidental daily deaths times the risk based on a time series of total deaths. The difference in these two quantities would give an indication of the degree of under(over)estimation of attributable risk using the standard time series risk. Disease-specific life tables would then be required to translate the disease-specific air pollution risks into years of life lost and number of individuals expected to survive a fixed time period under selected changes in ambient air pollution.
Conclusion
We have described the properties of an AHI which accounts for variation in air pollution exposure and risk over space and time. Our analysis demonstrates that examining trends in exposure alone, which has typically been the approach to air quality indicators, provides an incomplete picture of trends in the impact of air pollution. The AHI appears to be a more informative tool for measuring the change in air pollution attributable health risk over time as a means of addressing accountability for the impacts of programs to control air pollution. However, to be truly informative and advance the cause of accountability in air pollution reduction measures, the reasons for changes in the AHI, and conversely the lack of response in the AHI to changes in air pollution exposure levels must be examined. In this vein, additional research is required to attempt to explain sources of variation in risk over space and time.
References
Burnett RT, Dales RE, Raizenne ME, Krewski D, Summers PW, Roberts GR, Dann TF (1994) Effects of low ambient levels of ozone and sulphates on the frequency of respiratory admissions to Ontario hospitals. Environ Res 65:172–194 doi:10.1006/enrs.1994.1030
Burnett RT, Dales RE, Krewski D, Vincent R, Dann T, Brook JR (1995) Associations between ambient particulate sulfate and admissions to Ontario hospitals for cardiac and respiratory diseases. Am J Epidemiol 142:15–22
Burnett RT, Cakmak S, Brook J, Krewski D (1997) The role of particulate size and chemistry in the association between summertime ambient air pollution and hospitalization for cardio-respiratory diseases. Environ Health Perspect 105:614–620 doi:10.2307/3433607
Burnett RT, Smith-Doiron M, Stieb D, Cakmak S, Brook JR (1999) The effects of particulate and gaseous air pollution on cardiorespiratory hospitalizations. Arch Environ Health 54:130–139
Burnett RT, Smith-Doiron M, Stieb D, Raizenne M, Brook J, Dales RE, Leech JA, Krewski D (2001) The association between ozone and hospitalization for acute respiratory diseases in children under the age of two years. Am J Epidemiol 153:444–452 doi:10.1093/aje/153.5.444
Burnett RT, Dewanji A, Dominic F, Goldberg M, Cohen A, Krewski D (2003) On the relationship between time series studies, dynamic population studies, and estimating life lost due to short-term exposure to environmental risks. Environ Health Perspect 111:1170–1174
Burnett RT, Stieb D, Brook JR, Cakmak S, Dales R, Raizenne M, Vincent R, Dann T (2004) Associations between short-term changes in nitrogen dioxide and mortality in Canadian cities. Arch Environ Health 59:228–236 doi:10.3200/AEOH.59.5.228–236
Canadian Council of Ministers of Environment (CCME) 2000. Canada-wide Standards for Particulate Matter (PM) and Ozone: 11pp. www.ccme.ca/ourwork/air.html Accessed 8 Oct 2008
Canadian Environmental Sensitivity Indicators (CESI) Environment Canada Catalogue No. EN81–5/1–2006E-PDF: 61pp. http://www.environmentandresources.ca/default.asp?lang=En&n=6F66F932–1. Accessed 8 Oct 2008
Clancy L, Goodman P, Hamish S, Dockery DW (2002) Effect of air-pollution control on death rates in Dublin, Ireland: an intervention study. Lancet 360:1210–1214 doi:10.1016/S0140–6736(02)11281–5
Coyle D, Stieb D, Krewski D, Burnett R, Chen Y, DeCivita P, Thun M (2003) Impact of air pollution exposure on quality adjusted life expectancy in Canada. J Toxicol Environ Health 66:1847–1864 doi:10.1080/15287390306447
De Civita P, Chestnut LG, Mills D, Rowe RD, Stieb D. 1999. Human Health and Environmental Benefits of Achieving Alternative Canada-wide Standards for Inhalable Particles (PM2.5, PM10) and Ground Level Ozone. Prepared for the Canada-wide Standards Development Committee for Particulate Matter and Ozone. July 25, 1999
Delfino RJ, Murphy-Moulton AM, Burnett RT, Brook JR, Becklake MR (1997) Effects of ozone and particulate air pollution on emergency room visits for respiratory illnesses in Montreal. Am J Respir Crit Care Med 155:568–576
Dominici F, Samet J, Zeger L (2000) Combining evidence on air pollution and daily mortality from twenty largest US cities: a hierarchical modeling strategy. R Stat Soc 163:263–302 doi:10.1111/1467-985X.00170
Dominici F, McDermott A, Zeger SL, Samet JM (2002) On generalized additive models in time series studies of air pollution and health. Am J Epidemiol 156:193–203 doi:10.1093/aje/kwf062
Friedman MS, Powell KE, Hutwagner L, Graham LM, Teague WG (2001) Impact of changes in transportation and commuting behaviors during the 1996 summer Olympic games in Atlanta on air quality and childhood asthma. JAMA 285:897–905 doi:10.1001/jama.285.7.897
Goldberg MS, Burnett RT, Yale J-F, Valois M-F (2005) Associations between ambient air pollution and daily mortality among persons with diabetes and cardiovascular disease. Environ Res 100:255–267 doi:10.1016/j.envres.2005.04.007
Health Effects Institute 2003. Communication 11—Assessing the Health Impact of Air Quality Regulations: Concepts and Methods for Accountability Research. Boston: Health Effects Institute, 2003
Hedley AJ, Wong C-M, Thach TQ, Ma S, Lam T-H, Anderson HR. 2002. Cardiorespiratory and all-cause mortality after restrictions on sulphur content of fuel in Hong Kong: an intervention study
Johansen H, Thillaiampalam S, Nguyen D, Sambell C (2005) Diseases of the circulatory system—hospitalization and mortality. Health Rep 17:49–53
Krewski D, Burnett RT, Goldberg MS, Hoover K, Siemiatycki J, Jerrett M, Abrahamowicz M, White WH (2003) Overview of the Reanalysis of the Harvard Six Cities Study and American Cancer Society Study of Particulate Air Pollution and Mortality. J Toxicol Environ Health 66:1507–1552 doi:10.1080/15287390306424
Lin M, Chen Y, Burnett RT, Villeneuve PJ, Krewski K (2002) The influence of ambient coarse particulate matter on asthma hospitalization in children: case-crossover and time-series analyses. Environ Health Perspect 110:575–581
Miller BC, Armstrong B (2001) Quantification of the impact of air pollution on chronic cause-specific mortality. Institute of Occupational Medicine, Research Report TM/01/08, December 2001. Edinburgh, Scotland
PHAC - Public Health Agency of Canada Life and Breath: Respiratory Disease in Canada (2007) Ottawa: Public Health Agency of Canada. Published by authority of the Minister of Health (pp. 39–45) http://www.phac-aspc.gc.ca/publicat/2007/lbrdc-vsmrc/index-eng.php.
Pope CA (1989) Respiratory disease associated with community air pollution and a steel mill. Utah Valley. Am. J. Popul Health 79:623–628
Pope CA III, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, Godleski J (2004) Cardiovascular mortality and long-term exposure to particulate air pollution. Circulation 109:71–77 doi:10.1161/01.CIR.0000108927.80044.7F
Rabl A (2006) Analysis of air pollution mortality in terms of life expectancy changes: relation between time series, intervention, and cohort studies. Environ Health: A Global Access Sci Source 5:1–11
Ramsay T, Burnett RT, Krewski D (2003) Underestimation of standard errors in generalized additive models linking mortality to ambient particulate matter. Epidemiology 14:18–23 doi:10.1097/00001648-200301000-00009
Sen PK (1968) Estimates of the regression coefficient based on Kendall’s tau. J Am Stat Assoc 63:1379–1389 doi:10.2307/2285891
Shin HH, Stieb DM, Jessiman B, Goldberg MS, Brion O, Brook J et al (2008) A temporal, multi-city model to estimate the effects of short-term exposure to ambient air pollution on health. Environ Health Perspect 116(9):1147–1153
Stieb DM, Judek S, Burnett RT (2002) Meta-analysis of time-series studies of air pollution and mortality: effects of gases and particles and the influence of cause of death, age, and season. J Air Waste Manag Assoc 52:470–484
Szysykowicz M (2006) Use of generalized linear mixed models to examine the association between air pollution and health outcomes. Int J Occup Med Environ Health 19:224–227 doi:10.2478/v10001-006-0032-7
United States Environmental Protection Agency. The Benefits and Costs of the Clean Air Act: 1970 to 1990. October, 1997
Acknowledgement
We acknowledge that this article is part of the proceedings of the workshop on methodologies for environmental public health tracking of air pollution effects held in Baltimore in January 2008.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Shin, H.H., Burnett, R.T., Stieb, D.M. et al. Measuring public health accountability of air quality management. Air Qual Atmos Health 2, 11–20 (2009). https://doi.org/10.1007/s11869-009-0029-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11869-009-0029-z