Abstract
Background
Proton pump inhibitors (PPI) are widely used among general practitioners (GP) and hospital doctors alike as a first-line agent for the management of various approved conditions. However, PPIs do have an established side-effect profile that can be over looked when prescribing these agents outside of their Food Drug Administration (FDA) indications.
Aims
The aim of this audit is to establish that PPIs are often prescribed without any clear documented indication as to why, particularly in the elderly population, despite multiple previous studies conducted which showed an over-use of these medicines.
Methods
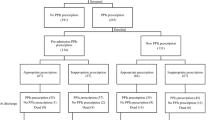
We conducted a retrospective observational study of the patients admitted to an acute hospital in Ireland in February 2018. A cohort of patient charts were pulled from medical records and reviewed. Medical notes, GP letters, discharge summaries and prescriptions were reviewed in order to establish the primary indication for PPI prescription.
Results
One hundred seventy-four (n = 174) inpatient records were randomly assessed during the audit. Of these patients, 85 of them were taking PPIs regularly. 54.7% (n = 46) were prescribed a PPI without any documented indication. 46.4% (n = 39) of these patients were > 75 years of age. 54.7% (n = 46) of patients were prescribed esomeprazole. The commonest indication for prescribing PPIs was to reduce the risk of gastric ulceration associated with NSAID use, which was 68.4% (n = 26) of those who were prescribed a PPI in accordance with guidelines.
Conclusion
Irrational prescribing of PPIs continues both in hospital and in general practise. It is imperative that the side-effects of these medicines are weighed against the benefit and cost effectiveness, especially in the elderly population where polypharmacy remains a substantial concern.
Similar content being viewed by others
References
Sachs G, Shin JM, Howden CW (2006) Review article: The clinical pharmacology of proton pump inhibitors. Alimentary Pharmacol Ther 23:2–8. https://doi.org/10.1111/j.1365-2036.2006.02943
Dean, Laura (2010). Comparing proton pump inhibitors. PubMed Health. Retrieved 16 July 2016
Rossi S, editor. Australian medicines handbook 2006. Adelaide: Australian Medicines Handbook; 2006. ISBN 0-9757919-2-34
Muhammad Haroon, Faiza Yasin, Syed K M Gardezi, Fahd Adeeb, and Frank Walker. Inappropriate use of proton pump inhibitors among medical inpatients: a questionnaire-based observational study. JRSM Short Rep 2013 Aug; 4(8)
Chia CTW, Lim WP, Vu CKF (2014) Inappropriate use of proton pump inhibitors in a local setting. Singap Med J 55(7):363–366
Linsky A, Gupta K, Lawler EV, Fonda JR, Hermos JA (2010) Proton pump inhibitors and risk for recurrent Clostridium difficile infection. Arch Intern Med 170:772–778
Howell MD, Novack V, Grgurich P et al (2010) Iatrogenic gastric acid suppression and the risk of nosocomial Clostridium difficile infection. Arch Intern Med 170:784–790
Benjamin Lazarus, MBBS, Yuan Chen, MS, Francis P. Wilson, MD, MS,3 Yingying Sang, MS,1 Alex R. Chang, MD, MS,4 Josef Coresh, MD, PhD,1,5 and Morgan E. Grams, MD, PhD1,5 Proton pump inhibitor use and risk of chronic kidney disease, JAMA Intern Med 2016 Feb 1; 176(2): 238–246
Corleto VD, Festa S, Di Giulio E, Annibale B (2014) Proton pump inhibitor therapy and potential long-term harm. Curr Opin Endocrinol Diabetes Obes 21(1):3–8. https://doi.org/10.1097/MED.0000000000000031
B MG, Bennett K, Tilson L, Barry M (2005) Cost effective prescribing of proton pump inhibitors (PPI's) in the GMS Scheme. Ir Med J 98(3):78–80
The gain in quality-adjusted life months by switching to esomeprazole in those with continued reflux symptoms in primary care: EncomPASS--a cluster-randomized trial. Moayyedi P, Armstrong D, Hunt RH, Lei Y, Bukoski M, White RJ Am J Gastroenterol. 2010 Nov; 105(11):2341–6
Bhatnagar P, Wickramasinghe K, Wilkins E, et al, Trends in the epidemiology of cardiovascular disease in the UK heart published online first: 22 August 2016. doi: 10.1136/heartjnl-2016-309573
El-Serag HB, Sweet S, Winchester CC, Dent J (2014) Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 63(6):871–880
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval was sought and granted by the institutional ethics committee at Our Lady’s Hospital, Navan.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Ali, O., Poole, R., Okon, M. et al. Irrational use of proton pump inhibitors in general practise. Ir J Med Sci 188, 541–544 (2019). https://doi.org/10.1007/s11845-018-1891-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-018-1891-1