Abstract
Objective
The aim of this study was to evaluate the effects of different doses of dexmedetomidine (Dex) compounded propofol and fentanyl on intraoperative somatosensory evoked potential (SEP) and motor evoked potential (MEP) monitoring on senile patients.
Methods
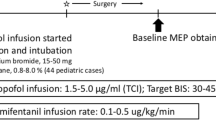
Forty-five patients undergoing elective spinal surgery were randomly divided into three groups: group C, group D1 (Dex, 0.3 μg kg−1 h−1), and group D2 (Dex, 0.8 μg kg−1 h−1). Anesthesia administration: midazolam, propofol, fentanyl, and cisatracurium. Anesthesia maintenance: propofol and fentanyl. No muscle relaxant was used throughout the operation. When muscle relaxation was T 4/T 1 > 75 %, SEPs and MEPs were monitored for the baseline. In group D1, Dex (0.3 μg/kg, loading dose) was administered, followed by a 0.3 μg kg−1 h−1 infusion of said drug until the end of surgery. In group D2, Dex (0.8 μg/kg, loading dose) was injected, followed by a 0.8 μg kg−1 h−1 infusion of said drug.
Results
Compared with group C, no significant difference was observed in the amplitude and latency of SEP (P15–N20) waves in groups D1 and D2 (P > 0.05). In groups C and D1, the MEP waveform did not disappear at every stage. In group D2, three patients lost the MEP waveform after the Dex loading dose, while four patients lost it during the Dex infusion stage. A significant difference was observed between groups C and D1. The median time to recover the MEP waveform was 47 min.
Conclusions
Dex did not affect SEPs of senile patients, but inhibited MEPs when larger doses were administered.

Similar content being viewed by others
References
Schwartz DM, Auerbach JD, Dormans JP et al (2007) Neurophysiological detection of impending spinal cord injury during scoliosis surgery. J Bone Joint Surg Am 89:2440–2449
Bronson WH, Forsh D, Qureshi SA et al (2012) Evolving compartment syndrome detected by loss of somatosensory- and motor-evoked potential signals during cervical spine surgery. Orthopedics 35:1453–1456
Shida Y, Shida C, Hiratsuka N et al (2012) High-frequency stimulation restored motor-evoked potentials to the baseline level in the upper extremities but not in the lower extremities under sevoflurane anesthesia in spine surgery. J Neurosurg Anesthesiol 24:113–120
Tamkus AA, Rice KS, Kim HL (2013) Differential rates of false-positive findings in transcranial electric motor evoked potential monitoring when using inhalational anesthesia versus total intravenous anesthesia during spine surgeries. Spine J 14(8):1440–1446
Ravasio G, Gallo M, Beccaglia M et al (2012) Evaluation of a ketamine-propofol drug combination with or without dexmedetomidine for intravenous anesthesiain cats undergoing ovariectomy. J Am Vet Med Assoc 241:1307–1313
Tobias JD, Goble TJ, Bates G et al (2008) Effects of dexmedetomidine on intraoperative motor and somatosensory evoked potential monitoring during spinal surgery in adolescents. Paediatr Anaesth 18:1082–1088
American Clinical Neurophysiology Society (2006) Guideline 9A: guidelines on evoked potentials. Am J Electroneurodiagnostic Technol 46:240–253
American Clinical Neurophysiology Society (2006) Guideline 9D: guidelines on short-latency somatosensory evoked potentials. Am J Electroneurodiagnostic Technol 46:287–300
American Clinical Neurophysiology Society (2006) Guideline 10: guidelines for writing clinical evoked potential reports. Am J Electroneurodiagnostic Technol 46:301–305
Rouche O, Wolak-Thierry A, Destoop Q et al (2013) Evaluation of the depth of sedation in an intensive care unit based on the photo motor reflex variations measured by video pupillometry. Ann Intensive Care 3:5
Monk TG, Weldon BC (2011) Does depth of anesthesia monitoring improve postoperative outcomes? Curr Opin Anaesthesiol 24:665–669
Gürses E, Sungurtekin H, Tomatir E et al (2004) Assessing propofol induct- ion of anesthesia dose using bispectral index analysis. Anesth Analg 98:128–131
Schmidt GN, Bischoff P, Standl T et al (2005) SNAP index and bispectral index during different state of propofol/remifentanil anaesthesia. Anaesthesia 60:228–230
Sloan TB, Heyer EJ (2002) Anesthesia for intraoperative neurophysiologic monitoring of the spinal cord. J Clin Neurophysiol 19:430–443
Kim SM, Yang H, Park SB et al (2012) Pattern-specific changes and discordant prognostic values of individual leg-muscle motor evoked potentials during spinal surgery. Clin Neurophysiol 123:1465–1470
Stone LS, Wilcox GL (2004) Alpha-2-adrenergic and opioid receptor additivity in rat locus coeruleus neurons. Neurosci Lett 361:265–268
Thornton C, Lucas MA, Newton DE et al (1999) Effects of dexmedetomidine on isoflurane requirements in healthy volunteers. 2: auditory and somatosensory evoked responses. Br J Anaesth 83:381–386
Kajiyama S, Nakagawa I, Hidaka S et al (2009) Effect of dexmedetomidine on intraoperative somatosensory evoked potential monitoring. Masui 58:966–970
Bala E, Sessler DI, Nair DR et al (2008) Motor and somatosensory evoked potentials are well maintained in patients given dexmedetomidine during spine surgery. Anesthesiology 109:417–425
Mahmoud M, Sadhasivam S, Salisbury S et al (2010) Susceptibility of transcranial electric motor-evoked potentials to varying targeted blood levels of dexmedetomidine during spine surgery. Anesthesiology 112:1364–1373
Conflict of interest
All authors have no conflict of interest regarding this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, Z., Lin, S. & Shao, W. Effects on somatosensory and motor evoked potentials of senile patients using different doses of dexmedetomidine during spine surgery. Ir J Med Sci 184, 813–818 (2015). https://doi.org/10.1007/s11845-014-1178-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-014-1178-0