Abstract
Background
Hip reconstructive surgery in cerebral palsy (CP) patients necessitates either femoral varus derotational osteotomy (VDRO) or pelvic osteotomy, or both. The purpose of this study is to review the results of a moderate varisation [planned neck shaft angle (NSA) of 130°] in combination with pelvic osteotomy for a consecutive series of patients.
Methods
Patients with CP who had been treated at our institution for hip dysplasia, subluxation or dislocation with VDRO in combination with pelvic osteotomy between 2005 and 2010 were reviewed.
Results
Forty patients with a mean follow-up of 5.4 years were included. The mean age at the time of operation was 8.9 years. The majority were non-ambulant children [GMFCS I–III: n = 11 (27.5 %); GMFCS IV–V: n = 29 (72.5 %)]. In total, 57 hips were treated with both femoral and pelvic osteotomy. The mean pre-operative NSA angle of 152.3° was reduced to 132.6° post-operatively. Additional adductor tenotomy was performed in nine hips (16 %) at initial operation. Reimers’ migration percentage (MP) was improved from 63.6 % pre-operatively to 2.7 % post-operatively and showed a mean of 9.7 % at the final review. The results were good in 96.5 % (n = 55) with centred, stable hips (MP <33 %), fair in one with a subluxated hip (MP 42 %) and poor in one requiring revision pelvic osteotomy for ventral instability.
Conclusions
This approach maintains good hip abduction and reduces soft-tissue surgery. Moderate varisation in VDRO in combination with pelvic osteotomy leads to good mid-term results with stable, pain-free hips, even in patients with severe spastic quadriplegia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spastic hip subluxation or dislocation is a frequent problem in children with cerebral palsy (CP). It is present among all functional levels but its frequency correlates clearly with the severity of the disease. Only 7 % of independent ambulators but up to 60–90 % of non-walking patients with severe spastic quadriplegia are affected [1].
Possible clinical problems associated with spasticity and hip instability include restriction of the ability to stand and walk, sitting imbalance, diminished hip motion, prevention of further motor progression, difficulty with perineal care and pain [1–3]. Unilateral dislocation may cause pelvic obliquity and attribute to scoliosis [4, 5].
For the treating surgeon, several surgical procedures are available to restore hip stability. Most commonly, combinations of soft-tissue balancing measures, femoral varus derotational osteotomy (VDRO) and pelvic osteotomies are used. It is known that the effect of the corrective femoral osteotomy alone on hip centration may not be sufficient, especially in severely subluxated or dislocated joints in patients with higher GMFCS levels [6]. The overall results are better when all existing deformities of the pelvis and the femur are corrected [2, 3, 7–12]. To achieve this goal, multiple surgical procedures are often performed. However, there remains controversy about the amount of surgery that is required to stabilise the hip [13, 14]. Even with multiple surgical procedures, re-dislocations must be expected in 6–7 % of cases [3].
It has been shown that the neck shaft angle (NSA) increases over time after a VDRO. Therefore, some authors suggest that children with higher GMFCS levels may require a higher amount of varisation with extensive soft-tissue release to maintain hip stability, accepting the possible higher risk of avascular necrosis (AVN) [15, 16]. Regarding the amount of VDRO, no consensus exists on how much correction of the proximal femur should be executed. One of the rare recommendations by Miller et al. [15] suggests a correction to a post-operative NSA down to 100° in non-walking patients and 120° in walking patients, mostly in conjunction with an extensive release of the adductors.
At our centre, we perform a combination of a pelvic osteotomy and a moderate VDRO with a planned post-operative NSA of 130° in a similar manner across all GMFCS levels. We believe that this will avoid a release of the adductors in most cases and still lead to stable, pain-free hips. The purpose of this paper is to review our results, to evaluate the frequency of complications, the necessity of soft-tissue releases and to report the radiologic and clinical outcome regarding hip stability.
Patients and methods
Following approval from the ethical committee, we retrospectively reviewed the X-rays and data sheets of all paediatric patients with CP who had been treated in our institution between 2005 and 2010 for hip dysplasia, subluxation or dislocation with a combined pelvic osteotomy and VDRO. Included were all patients who had a minimum follow-up of 2 years clinically and radiographically. Patients with prior bony or soft-tissue operations at the level of the hip were excluded, as well as patients with neurological disorders other than infantile CP. Antispasmodic therapeutics such as baclofen, phenol or botox injections were not taken into consideration.
Technical description
Prior to surgical intervention, computed tomography (CT) scans with 3D reconstructions were performed to visualise the direction of migration, as well as the sphericity and the bony deformity. For the pelvic osteotomy, a Smith–Peterson approach was used. The type of osteotomy was adjusted to the predominant direction of instability: Dega osteotomy for a more posterior, Pemberton osteotomy for a more anterior instability or for a multi-directional instability. In all cases, VDRO was performed through a subvastus approach. It included a varisation, derotation and shortening. The amount of correction was adjusted to the individual situation: intra-operatively correct rotated a.p. X-rays of the proximal femur were obtained and the amount of femoral varisation was defined with a goal of an NSA of around 130° after varisation (Fig. 1). The amount of femoral shortening depended on the height of bone graft needed for inter-position on the pelvic osteotomy side. An additional 5 mm was taken to reduce tension for an easier and more gentle reduction of the hip joint. By reducing pressure on the hip joint and, thereby, on the femoral head, the risk of AVN can be decreased. Fixation was achieved with either an AO blade plate or as described by Rutz and Brunner with an LCP paediatric hip plate (Synthes, Grenchen, Switzerland) [17]. In all cases, an intra-pelvine lengthening of the iliopsoas tendon was performed. An additional adductor tenotomy was only done if intra-operative hip abduction was less than 20° after pelvic osteotomy and VDRO. If necessary, an abductor release was performed in the case of a fixed abduction contracture, mostly after reduction of an anterior hip dislocation. Post-operatively, hip spica cast was applied for at least 2 weeks, primarily for analgetic reasons, in some cases prolonged for 4–6 weeks, depending on bone quality and activity level. Walking patients older than 10 years at operation were not immobilised in a hip spica cast post-operatively.
Example of intra-operative measurement of the neck shaft angle (NSA). For correct measurements and corrected anteversion, the growth plate of the greater trochanter must be fully visible (white arrow). The pre-operative NSA was measured on an image intensifier and correction was adjusted to the measured value
Analysis
Gender, GMFCS level, age at surgery and details of the operation were recorded in a spreadsheet. In patients with bilateral surgery, each hip was reviewed independently, except for age analysis. Pre-, post-operative and the latest follow-up radiographs were analysed for NSA as well as migration percentage (MP) by a consultant orthopaedic surgeon (KR). According to Reimers, a hip was regarded as centred with an MP <33 %, subluxated with an MP of at least 33 % and dislocated with an MP of 100 % [18]. With regards to this, we classified the hips as good (MP <33 %), fair (MP between 33 and 100 %) and poor (MP 100 %). Further, complications were recorded and the presence of osteonecrosis was evaluated.
Statistical methods
All analyses were performed using SPSS 22.0 (Armonk, NY, USA). Geometric means and relative standard deviations were calculated for continuous variables. The Mann–Whitney U was used for baseline measurements. One-way analysis of variance (ANOVA) with post hoc testing was used to examine differences in the NSA and MP pre-, post-operative and last follow-up measurements (level of significance 0.05). Cross-tabulation and the Chi-square test was used for the analysis of adductor release surgery among the two groups (walkers and non-walkers).
Results
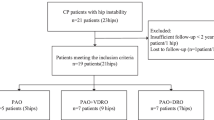
Eighty-three paediatric patients were treated operatively for neurologic hip dysplasia at our institution between 2005 and 2010. Out of 62 patients with cerebral palsy, 22 did not meet our inclusion criteria.
Forty patients (20 males and 20 females) were included in our study. Twenty-nine patients (72.5 %) were non-walkers (GMFCS IV or V) and 11 patients (27.5 %) were walkers (GMFCS I, II or III) (Table 1). The average patient age at surgery was 8.9 years (range 2.6–14.8 years), 9.3 years among walkers (range 2.6–13.3 years) and 8.8 years among non-walkers (range 4.3–14.7). The average duration of follow-up was 65.4 months (range 24–123 months). The average age at final follow-up was 14.4 years (range 9.1–20.4 years). Mann–Whitney U testing did not show any difference between groups (walkers/non-walkers) in regards to baseline measurements.
According to Reimers, nine hips were centred, 35 subluxated and 13 dislocated at the time of operation. For all nine centred hips (nine patients), dysplastic acetabular roof changes were documented. Six of these nine patients were walkers. The other three centred hips were operated in conjunction with a combined procedure of the contralateral hip which showed a subluxation or dislocation. In total, 57 pelvic osteotomies in combination with VDRO were performed. Seventeen patients (42.5 %) were treated with a bilateral pelvic and femoral osteotomy, and 23 patients (57.5 %) had a combined pelvic osteotomy and VDRO only on one side. Thirty-four Dega osteotomies were performed in hips with a more posterior instability. In four hips with a planned Dega osteotomy for posterior instability, the inner table of the ilium was perforated while levering down the acetabular roof, resulting in a more Pemberton type osteotomy. Altogether, 19 Pemberton osteotomies were performed: seven hips showed an isolated anterior and 12 hips a multi-directional instability. The mean pre-operative NSA was 152.3° (range 142°–160°), as measured in standardised positioning on fluoroscopy intra-operatively. The average planned varisation was 16.9° (range 10°–30°), resulting in an average planned post-operative NSA of 135.3° (range 126°–147°). An average external rotation of 20.9° (range 5°–30°) and shortening of 18.0 mm (range 0–35 mm) was executed. For osteotomy fixation, an AO blade plate was used in 38 hips (66.7 %) and an LCP paediatric hip plate in 19 hips (33.3 %). At the time of index surgery, additional soft-tissue release was performed in 13 hips (22.8 %): nine adductor tenotomies and in four hips, a release of the abductors (two patients with bilateral anterior hip dislocation).
The mean measured post-operative NSA was 132.6° (range 115°–146°). At the latest follow-up, the mean NSA was 137.2° (range 116°–159°) (Fig. 2). Pre-operatively, we found in non-walkers a slightly higher NSA than in walkers (not significant). The post-operative NSA in non-walkers was significantly lower than in walkers (131.5° vs. 136.3°, p < 0.011). Interestingly, non-walkers showed less elevation of the NSA (131.5°–135.4°) compared to walkers (136.3°–143.8°) at final follow-up (Table 2). Reimers’ MP could be improved from a mean of 63.6 % pre-operatively to 2.7 % post-operatively. At the latest follow-up, the mean MP was 9.7 % (Table 2). We did not see any statistical difference between walkers and non-walkers regarding the MP.
During follow-up, another soft-tissue release was performed in seven hips between 6 and 57 months after the initial procedure: four hips had a tenotomy of the adductors and an abductor release was performed in three hips. Three of these seven hips already had a soft-tissue release during the first surgery. In total, 17 out of 57 hips (29.8 %) had a soft-tissue release other than iliopsoas lengthening during the initial procedure and/or the post-operative course. We did not find a statistical difference in the total amount of adductor releases in walkers and non-walkers. The final results were good, with stable, centred hips (MP <33 %) in 96.5 % of the hips (n = 55). A fair result was recorded in one hip with a recurrent subluxation (MP 42 %). One hip was classified as poor despite an MP of 0 % at the latest follow-up because of a necessary revision due to painful anterior hip instability 9 months after initial operation. Two patients needed early operative revisions: in one case, a re-osteosynthesis had to be performed for varus malunion due to implant failure in poor bone quality. One patient suffered from post-operative soft-tissue infection that needed debridement and antibiotic therapy.
The outpatient records revealed that none of the patients suffered from hip pain at the latest follow-up.
Discussion
The concept of hip reconstruction in children with CP is a widely accepted treatment for spastic hip sub- and dislocation. Although an effective treatment, the combination of femoral varus derotation and pelvic osteotomy was found to have a complication rate of up to 30 % [13] and recurrence rates of sub- and dislocated hips are reported in 5–10 % at long-term follow-up [3, 19–21].
According to Rutz et al. [22], pre-operative MP was the most influential risk factor affecting the post-operative outcome, suggesting hip reconstruction at an early stage. In our study, 35 subluxated and 13 dislocated hips were treated with hip reconstruction, having a low complication rate concerning re-dislocation. We also agree to, instead, perform a hip reconstruction including both femoral varus derotation and pelvic osteotomy at an early stage to reduce the re-dislocation rate.
A review of the current literature shows that there is no consensus or clear recommendation on how much the NSA should be corrected in varus to achieve and maintain stable hips with the lowest complication rates (Table 3). One of the rare recommendations suggests a correction to the post-operative NSA to 100° in non-walking patients and 120° in walking patients, mostly in conjunction with an extensive release of the adductors [15]. Rutz et al. aimed at a post-operative NSA of 120–125°, with recurrent hip dislocations in 2 out of 168 hips. The extent of soft-tissue releases was not recorded [22]. In our study, we combined moderate varisation with a post-operative NSA of 132.6° with restrained release of the adductors and had a low complication rate concerning instability, in walkers and non-walkers as well. Recently, Bayusentono and colleagues [23] recommended adequate varisation at the time of the primary surgery, although they did not find significant loss of correction of the NSA when analysing more than 800 radiographs over a period of 12 years. They found a statistically significant increase of the MP of 2.0 % per year in GMFCS level IV and 3.5 % in level V, which corresponds to our increase of 4.0 % in walkers and 7.7 % in non-walkers during a mean follow-up of more than 5 years. Jóźwiak et al. [16] indicate, in another long-term analysis, that the loss of correction is progressive. Therefore, the authors stated to use a more extensive soft-tissue release and a more radical VDRO.
According to the literature, even in combined VDRO and pelvic osteotomy, releases of the adductors are carried out in up to 80 % of patients [15, 23–27]. It is known that soft-tissue corrections have a less predictable outcome than bony procedures, e.g. an extensive adductor release may fail due to scarring. We, therefore, only perform adductor release if abduction does not reach at least 20° at the end of surgery when the shortening of the femur has already lead to some relative lengthening of the muscles, even though our results are comparable to other series, in which a greater amount of varisation was performed and adductor release was carried out in 70–100 % [15, 21, 28, 29]. Miller et al., for example, performed an adductor release at the beginning of the surgery if the abduction did not exceed 45° [15] and McNerney et al. performed adductor lengthening to obtain abduction of 60° [19].
One of the possible complications of proximal femoral varisation is AVN of the femoral head. There has been discussion as to whether excessive varisation may lead to AVN [24]. A study comparing two different techniques for femoral varisation (end-to-side and end-to-end), which resulted in a post-operative angle of around 100° in both cases, reported an 5.5–6 % AVN rate [30]. We did not find any signs of AVN in our collective during the whole radiologic follow-up.
For 96.5 % of stable hips with an MP <33 % after an average of 5.4 years, our results are comparable to other studies (Table 3). Our mid-term results were able to show that even a moderate VDRO in combination with a pelvic osteotomy is a safe way to generate stable, pain-free hips. Outcomes were good in 96.5 % of patients and we performed adductor releases in only 13 hips (22.8 %).
There are important drawbacks to our analysis. Foremost, only around 50 % of patients reached skeletal maturity at the time of the latest follow-up. Our mean follow-up was 5.4 years; therefore, long-term results need to verify the effectiveness of this treatment. Secondly, the valgus position of the proximal femur is often overestimated on a.p. radiographs due to oblique projection caused by high femoral anteversion. The measurements of the NSA were only taken on a standardised and correctly rotated a.p. view according to Laplaza and Root intra-operatively [31]. X-rays taken post-operatively and during the latest follow-up often showed some rotation, which has a well-known impact on the measurement of the NSA. The measured NSA will, rather, be higher on a not correctly rotated X-ray and the loss of correction of the NSA at last follow-up (4.6° on average in our study) is rather over- than underestimated. Routinely, radiographic follow-up included pelvic a.p. X-rays only. In case of clinical suspicion for an anterior progressive subluxation, we do indeed perform a CT scan with 3D reconstruction. Still, anterior progressive subluxation might be missed or not be detected at an early stage.
We were able to show that our approach of a moderate VDRO in combination with a pelvic osteotomy has good mid-term results with stable and pain-free hips. Using this technique even in patients with severe spastic quadriplegia is safe and the amount of soft-tissue surgery can be limited.
References
Pritchett JW (1983) The untreated unstable hip in severe cerebral palsy. Clin Orthop Relat Res 173:169–172
Bagg MR, Farber J, Miller F (1993) Long-term follow-up of hip subluxation in cerebral palsy patients. J Pediatr Orthop 13:32–36
Brunner R, Baumann JU (1994) Clinical benefit of reconstruction of dislocated or subluxated hip joints in patients with spastic cerebral palsy. J Pediatr Orthop 14:290–294
Cooperman DR, Bartucci E, Dietrick E, Millar EA (1987) Hip dislocation in spastic cerebral palsy: long-term consequences. J Pediatr Orthop 7:268–276
Heidt C, Hollander K, Wawrzuta J et al (2015) The radiological assessment of pelvic obliquity in cerebral palsy and the impact on hip development. Bone Joint J 97-B:1435–1440. doi:10.1302/0301-620X.97B10.35390
Brunner R, Baumann JU (1997) Long-term effects of intertrochanteric varus-derotation osteotomy on femur and acetabulum in spastic cerebral palsy: an 11- to 18-year follow-up study. J Pediatr Orthop 17:585–591
Carstens C, Niethard FU, Schwinning M (1992) Surgical treatment of hip dislocation in patients with infantile cerebral palsy. Z Orthop Ihre Grenzgeb 130:419–425. doi:10.1055/s-2008-1039645
Jerosch J, Senst S, Hoffstetter I (1995) Combined realignment procedure (femoral and acetabular) of the hip joint in ambulatory patients with cerebral palsy and secondary hip dislocation. Acta Orthop Belg 61:92–99
Molloy MK (1986) The unstable paralytic hip: treatment by combined pelvic and femoral osteotomy and transiliac psoas transfer. J Pediatr Orthop 6:533–538
Mubarak SJ, Valencia FG, Wenger DR (1992) One-stage correction of the spastic dislocated hip. Use of pericapsular acetabuloplasty to improve coverage. J Bone Joint Surg Am 74:1347–1357
Song HR, Carroll NC (1998) Femoral varus derotation osteotomy with or without acetabuloplasty for unstable hips in cerebral palsy. J Pediatr Orthop 18:62–68
Zhang S, Wilson NC, Mackey AH, Stott NS (2014) Radiological outcome of reconstructive hip surgery in children with gross motor function classification system IV and V cerebral palsy. J Pediatr Orthop B 23:430–434. doi:10.1097/BPB.0000000000000075
Bouwhuis CB, van der Heijden-Maessen HC, Boldingh EJK, Bos CFA, Lankhorst GJ (2015) Effectiveness of preventive and corrective surgical intervention on hip disorders in severe cerebral palsy: a systematic review. Disabil Rehabil 37:97–105. doi:10.3109/09638288.2014.908961
Stott NS, Piedrahita L; AACPDM (2004) Effects of surgical adductor releases for hip subluxation in cerebral palsy: an AACPDM evidence report. Dev Med Child Neurol 46:628–645
Miller F, Girardi H, Lipton G, Ponzio R, Klaumann M, Dabney KW (1997) Reconstruction of the dysplastic spastic hip with peri-ilial pelvic and femoral osteotomy followed by immediate mobilization. J Pediatr Orthop 17:592–602
Jóźwiak M, Marciniak W, Piontek T, Pietrzak S (2000) Dega’s transiliac osteotomy in the treatment of spastic hip subluxation and dislocation in cerebral palsy. J Pediatr Orthop B 9:257–264
Rutz E, Brunner R (2010) The pediatric LCP hip plate for fixation of proximal femoral osteotomy in cerebral palsy and severe osteoporosis. J Pediatr Orthop 30:726–731
Reimers J (1980) The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl 184:1–100
McNerney NP, Mubarak SJ, Wenger DR (2000) One-stage correction of the dysplastic hip in cerebral palsy with the San Diego acetabuloplasty: results and complications in 104 hips. J Pediatr Orthop 20:93–103
Sankar WN, Spiegel DA, Gregg JR, Sennett BJ (2006) Long-term follow-up after one-stage reconstruction of dislocated hips in patients with cerebral palsy. J Pediatr Orthop 26:1–7. doi:10.1097/01.bpo.0000190842.77036.d0
Mallet C, Ilharreborde B, Presedo A, Khairouni A, Mazda K, Penneçot GF (2014) One-stage hip reconstruction in children with cerebral palsy: long-term results at skeletal maturity. J Child Orthop 8:221–228. doi:10.1007/s11832-014-0589-9
Rutz E, Vavken P, Camathias C, Haase C, Jünemann S, Brunner R (2015) Long-term results and outcome predictors in one-stage hip reconstruction in children with cerebral palsy. J Bone Joint Surg 97:500–506. doi:10.2106/JBJS.N.00676
Bayusentono S, Choi Y, Chung CY, Kwon SS, Lee KM, Park MS (2014) Recurrence of hip instability after reconstructive surgery in patients with cerebral palsy. J Bone Joint Surg 96:1527–1534. doi:10.2106/JBJS.M.01000
Hoffer MM, Stein GA, Koffman M, Prietto M (1985) Femoral varus-derotation osteotomy in spastic cerebral palsy. J Bone Joint Surg Am 67:1229–1235
Al-Ghadir M, Masquijo JJ, Guerra LA, Willis B (2009) Combined femoral and pelvic osteotomies versus femoral osteotomy alone in the treatment of hip dysplasia in children with cerebral palsy. J Pediatr Orthop 29:779–783. doi:10.1097/BPO.0b013e3181b76968
Khouri N, Khalife R, Desailly E, Thevenin-Lemoine C, Damsin JP (2010) Proximal femoral osteotomy in neurologic pediatric hips using the locking compression plate. J Pediatr Orthop 30:825–831. doi:10.1097/BPO.0b013e31820156f2
Huh K, Rethlefsen SA, Wren TAL, Kay RM (2011) Surgical management of hip subluxation and dislocation in children with cerebral palsy: isolated VDRO or combined surgery? J Pediatr Orthop 31:858–863. doi:10.1097/BPO.0b013e31822e0261
Dhawale AA, Karatas AF, Holmes L, Rogers KJ, Dabney KW, Miller F (2013) Long-term outcome of reconstruction of the hip in young children with cerebral palsy. Bone Joint J 95-B:259–265. doi:10.1302/0301-620X.95B2.30374
Debnath UK, Guha AR, Karlakki S, Varghese J, Evans GA (2006) Combined femoral and Chiari osteotomies for reconstruction of the painful subluxation or dislocation of the hip in cerebral palsy. A long-term outcome study. J Bone Joint Surg Br 88:1373–1378. doi:10.1302/0301-620X.88B10.17742
Davids JR, Gibson TW, Pugh LI, Hardin JW (2013) Proximal femoral geometry before and after varus rotational osteotomy in children with cerebral palsy and neuromuscular hip dysplasia. J Pediatr Orthop 33:182–189. doi:10.1097/BPO.0b013e318274541a
Laplaza FJ, Root L (1994) Femoral anteversion and neck-shaft angles in hip instability in cerebral palsy. J Pediatr Orthop 14:719–723
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest or funding to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Reidy, K., Heidt, C., Dierauer, S. et al. A balanced approach for stable hips in children with cerebral palsy: a combination of moderate VDRO and pelvic osteotomy. J Child Orthop 10, 281–288 (2016). https://doi.org/10.1007/s11832-016-0753-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-016-0753-5