Abstract
Purpose
In children with cerebral palsy (CP), braces are used to counteract progressive joint and muscle contracture and improve function. We examined the effects of positional ankle–foot braces on contracture of the medial gastrocnemius (MG) and gait in children with CP while referencing to typically developing children.
Methods
Seventeen independently ambulant children with CP and calf muscle contracture (age 10.4 ± 3.0y) and 17 untreated typically developing peers (age 9.5 ± 2.6y) participated. Children with CP were analysed before and 16 ± 4 weeks after ankle–foot bracing. MG muscle belly length and thickness, tendon and fascicle length, as well as their extensibility were captured by 2D ultrasound and 3D motion capturing during passive, manually applied stretches. In addition, 3D gait analysis was conducted.
Results
Prior to bracing, the MG muscle–tendon unit in children with CP was 22 % less extensible. At matched amounts of muscle–tendon unit stretch, the muscle belly and fascicles in CP were 7 % and 14 % shorter while the tendon was 11 % longer. Spastic fascicles displayed 32 % less extensibility than controls. Brace wear increased passive dorsiflexion primarily with the knees flexed. During gait, children walked faster and foot lift in swing improved. MG muscle belly and tendon length showed little change, but fascicles further shortened (−11 %) and muscle thickness (−8 %) decreased.
Conclusions
Use of ankle–foot braces improves function but may lead to a loss of sarcomeres in series, which could explain the shortened fascicles. To potentially induce gastrocnemius muscle growth, braces may also need to extend the knee or complementary training may be necessary to offset the immobilizing effects of braces.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Symptomology of spastic Cerebral Palsy (CP) includes, but is not limited to, muscular weakness, overactivity and contracture [1]. Muscular contractures are thought to some degree to reflect muscle tissue that fails to keep up with bone growth [2]. Plantarflexors are typically seriously affected. Apart from altered neural control, they are intrinsically very stiff [3], resulting in equinus, the most common musculoskeletal impairment in CP [4]. Equinus gait compromises balance and is fatiguing, since it requires more activity of the triceps surae [5]. During childhood of children with CP, the loss in passive dorsiflexion is progressive [6]. Thus, muscle contracture of the triceps surae also seems to deteriorate. On a long-term painful bony foot deformities can result. Temporary immobilization of the stretched calf using casts or braces with or without botulinum toxin injections is a popular treatment [7, 8]. Braces are commonly applied in non-rigid deformities. By holding joints near their end-range, progressive contracture should be counteracted and spastic muscles are assumed to untighten and grow at a rate more equal to that of the bone. Eventually, the gait pattern should also improve. Yet, it is unclear how bracing actually affects the muscle morphometrics in spastic equinus deformity.
Muscle morphometrics in CP
Ultrasound scans provide a non-invasive means to gain information about a muscle’s architecture. It has already been shown that plantarflexor morphometrics in CP are altered with respect to typically developing peers (TD) [9–14]. In case of the medial gastrocnemius (MG), in one of the spastic leg muscles displaying largest volumetric atrophy [15], there is evidence for reduced muscle belly length (L MB), cross-sectional area and muscle belly thickness (MT) [9]. However, achilles tendon length (L TEND) appears to be longer [10] while MG fascicle (bundle of skeletal muscle fibres) length (L FASC) seems shorter than in TD [11, 12]. Concerning the latter, L FASC, some inconsistencies have been reported [13, 14]. These discrepancies may be partly explained by difficulties in standardizing the musculoskeletal conditions, e.g., the degree of muscle stretch, during the assessment. On a microscopic level, spastic muscle fibres were also found to contain very long sarcomeres, which was interpreted as an inability to add sarcomeres in series with growth [16, 17].
Potential response to bracing
Casts and orthotics are currently favourable for contracture management [18]. They should keep the plantarflexor’s muscle–tendon units (MTU) in a stretched position. This is assumed to increase L MB over time with a concomittant reduction in pathological equinus posture. Manual stretching of spastic MG can indeed transiently increase its L MB, L FASC, as well as L TEND [19], but the long-term effectiveness of manual stretch remains doubtful [18]. Cyclic stretches by an external, machine-driven device in combination with active training stimulated the MG fascicles to grow longer and become less stiff [20], positively demonstrating the MG’s adaptive potential. By contrast, most braces induce static, low load stretch over prolonged periods and also immobilise the muscle. Knowledge about the morphometric effects of chronic muscle stretch is primarily derived from healthy animals. When muscle from adult animal is immobilised in a lengthened position, sarcomeres have been shown to be added in series [21]. Muscle fibres in CP may thus grow longer in response to bracing. Yet, the fibres’ cross-section could also atrophy because of the immobilising effect [22]. In juvenile, developing animals, experiments point out that primarily the tendon, and not the muscle fibres, lengthens in response to stretched immobilisation [21, 23, 24]. Stimulated tendon growths could in fact reduce the stretch effects on muscle fibres and eventually induce sarcomere loss [23]. Such a scenario could theoretically decrease the MG muscle belly thickness [MT]. Because of cross-sectional atrophy and the pinnated fibre arrangement, the L MB could also decrease. In fact, it has been doubted that stretch-immobilization can promote muscle growth in children with CP [25].
The main aim of this study was therefore to longitudinally re-evaluate MG morphometrics in children with CP after a period of ankle–foot bracing. To define the status quo prior to bracing, L MB, MT, L FASC and fascicle angle (FA), as well as L TEND, in children with CP was contrasted with TD using ultrasound during passive, manually applied stretches. The total extensibility (~strain) of the muscle, fascicle and tendon was compared as well. We hypothesised that children with CP and equinus have shorter and thinner MG muscle bellies, shorter L FASC, but longer L TEND than TD, and that extensibility of the MTU and its components is reduced. After ankle–foot bracing, we expected that passive dorsiflexion would improve, L MB, L FASC and L TEND of the spastic MG would be lengthened and extensibility of the MTU and its components would increase. Our second aim was to compare the functional effects of bracing using 3D gait analysis. We expected dorsiflexion to improve during stance and swing, positively affecting foot positioning at ground contact. Walking speed and step length should thereby be increased.
Methods
Participants
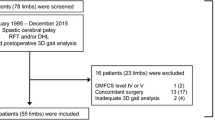
To be included, children with CP had to be classified as GMFCS I or II and display non-rigid equinus. Non-rigid equinus was defined as tone on the modified Ashworth Scale (MAS) <4 [26] and a lack of passive range of motion (PRoM) smaller than −10° dorsiflexion (with flexed or extended knees). Further exclusion criteria were a lack of passive PRoM greater than −10° of knee flexion from neutral, crouch gait, leg length discrepancies more than 2 cm, any previous surgery to the leg, botulinum toxin injections within 1 year or bracing within 3 months. We thereby consecutively included 17 (9/8 male and female; 9/8 unilaterally and bilaterally involved, 7/10 GMFCS I and II) children with CP (age range 5y 11mo–15y 6mo) from our outpatient department. As a reference group, 17 TD were included (6/11 male and female, age range 6y 0mo–15y 4mo). Only the (more) involved side was analysed in children with CP based on passive dorsiflexion. For TD, one leg was randomly chosen. Institutional ethics approval was granted and all subjects and their parents gave informed written consent.
Bracing
An articulated ankle–foot orthotic brace was individually manufactured out of glass and carbon-fibre–reinforced plastics (Fig. 1). The lower leg shell is an S-type calf-construction with condylar support. It is fixed below the tibial tuberosity with a Velcro strap. The foot shell is a circular foot support. Both parts are linked by a constraint metal ankle hinge aligned in maximum passive dorsiflexion, while keeping the knee extended without perceiving intolerable discomfort. The subtalar joint was locked by a circular frame, the heel was fixed with a removable heel cap.
Plantarflexion movement was blocked, and the dorsiflexion RoM was 5–10°. The brace was reviewed every 4–6 weeks and the metal ankle hinge was realigned if possible. If plantigrade position could be achieved and if tolerated, gas springs (~2–3 Nm) were integrated to provide a constant dorsiflexion push during night-wear (seven of 17 children). This resistance could be voluntary attenuated upon mild plantarflexor contraction and all 17 children were intended to wear this brace during sleep. If passive dorsiflexion was less than −5° from plantigrade, they were additionally prescribed daytime use to extend the duration of brace wear. Twelve of 17 children met the criteria for day-time use. Three of those were not compliant with day wear, so that a total of nine (of 17) wore the brace during both day and night. Eight of 17 wore the brace only at night and foot orthotics intended to prevent foot deformities due to mid-foot or subtalar instability during the day.
Set-up and data collection
All children with CP were analysed before and after bracing. Measurements were performed in the movement laboratory on the day of their outpatient appointments. TD were analysed on a single occasion. Apart from ultrasound scans, all participants were clinically manually examined by the same evaluator and underwent an instrumented 3D gait analysis (3DGA). PRoM for knee extension, popliteal angle (opposite hip flexed) and dorsiflexion with the knee flexed were measured using ruler-based goniometry. Plantarflexor tone was graded on modified Ashworth Scale (MAS) [26]. Passive dorsiflexion with the knee extended was instrumentally measured using motion capture data during MG ultrasound scans.
For 3DGA, a Vicon Nexus system (Vicon, Oxford, UK) with 8 MX-Cameras was used to capture barefoot gait at self-selected speed along a 12 m walkway. Markers were placed according to a modified Plug-In gait Model [27]. Marker data were sampled at 200 Hz and force plate at 1000 Hz via two force plates (AMTI, Watertown, USA). Gait analysis was repeated until five clean strikes on the force plates from each foot could be obtained.
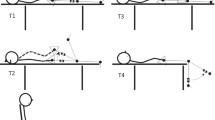
For the ultrasound scans, children were comfortably seated (hip semi-flexed) in a chair (Fig. 2). Retro-reflective markers of the 3D motion capture system remained on the leg (Fig. 2) to track knee alignment and ankle motion during the scan. A 7.5 MHz, 8 cm in width, linear array probe (Sonoline Adara; Siemens, Munich, Germany) was attached with a carbon cast that was equipped with a cluster of four markers. The probe was attached at two locations: over the muscle–tendon junction (MTJ) and over the mid-belly (halfway between popliteal crease and MTJ). The image plane was aligned with the fascicles according to a standardised protocol [28]. The leg was passively lifted and the knee extended as feasible. The same examiner manually moved the ankle slowly and continuously from flexion to extension and back. Prior to data collection, the ankle was preconditioned with three cycles. Then, three to five dorsiflexion stretches were captured while the children could view the ultrasound screen and were encouraged to relax. If muscle contraction was manually sensed as sudden resistance, or whenever contraction was visually apparent, trials were repeated.
Experimental setup: Left side Child positioning with custom-made carbon cast for probe fixation and markers of the motion capture system. Right side Superimposed ultrasound scans of the medial gastrocnemius a muscle–tendon junction (MTJ), and b its midbelly portion with representation of morphometric assessment. L FASC fascicle length, FA fascicle angle, MT muscle thickness
Data analysis
To compare spatio-temporal gait, velocity and step length were extracted and normalised as described by Hof [29], to account for growth. Peak values for ankle dorsiflexion during stance and swing and knee extension during stance were also analysed. The foot landing pattern was characterised by the foot-to-floor angle at ground contact. To quantify ankle kinetics, the peak moments during the first and second half of a stance were selected, as well as the peak power during push-off.
For the ultrasound scans, the position of the markers and the ultrasound movies were continuously captured using Vicon Nexus software with a sampling rate of 200 and 25 Hz, respectively. Subsequent analysis was done in MatLab software (MathWorks, Natick, USA). The MTJ in the ultrasound movies was manually located framewise (Fig. 2). Concerning the fascicles, three to five different mid-belly fascicles were separately localised (straight line between upper and deeper aponeurosis along hyperechoic [bright] collagenous tissue) and an automated tracking algorithm was used to continuously track their elongation during stretch [30]. MT was measured at minimum and maximum stretch only. MT was defined as the distance between the upper and deeper aponeurosis, perpendicular to the deep aponeurosis [10], located halfway between popliteal crease and MTJ. FA was calculated as: α = arcsin(MT/L FASC). The distal L TEND was defined as a straight-line from the heel marker to the MTJ. Since the entire Gastrocnemius MTU could not be tracked directly, L MTU was calculated using previously established equations relying on motion capture data concerning tibia length, knee and ankle angles, as well as on individual anthropometrics [31]. L MB was calculated as L MB = L MTU–L TEND [10]. L FASC was represented by the average of all fascicles. For each trial, MTU stretches (from minimum to maximum length) were separated. To represent the average L FASC, L MB and L TEND lengthening across the L MTU stretch for each individual, data of each stretch was split into ten equally spaced steps. Finally, the averages at these query points were taken before a third-order polynomial was fitted. For L MTU, L MB, L FASC and L TEND, minimum and maximum values were extracted. Besides, L MB, L FASC and L TEND were analysed at similar degrees of MTU stretch. Since there was no common overlap in L MTU between all participants, the midrange L MTU (halfway between minimum and maximum stretch) was first calculated for each individual with CP before bracing. To standardise comparisons, the average midrange L MTU from children with CP was used for TD. To compare morphometrics before and after bracing, midrange L MTU could be exactly matched individually. All parameters were normalised to shank length, defined as from the malleolus to the knee marker. Their extensibility was calculated as % change between minimum and maximum length.
Statistics
Shapiro–Wilk tests were used to test normality. At baseline, children with CP were compared with TD. Statistical group differences were evaluated with independent t tests. To compare children with CP before and after bracing, paired t tests were performed. Mean differences and 95 % confidence intervals were calculated. Alpha-level was set at 0.05 (two–sided tests). Standardised effect sizes were expressed as Cohen’s d. Threshold values were 0.2, 0.5 and 0.8 for small, medium and large effects. Unless indicated differently, values are presented as mean (±1 SD).
Results
Participant characteristics and clinical exam
Values for TD and CP and the test statistics are summarised in Table 1. There were no significant differences in age, height, shank length or mass (p > 0.279). Children with CP demonstrated significantly shorter popliteal angles (p < 0.001). Average passive dorsiflexion in CP with knees flexed [8° (11°)] and extended [2° (10°)] was considerably reduced with respect to [TD 29° (8°)] and [15° (5°)], all p < 0.01. At Follow-up, on average 16 (4) weeks (range 12–24 weeks) apart, children with CP grew significantly and gained in mass, height and shank length. During clinical examination passive dorsiflexion improved with the knees in flexion [6° (11°), p = 0.048] and extension [4° (8°), p = 0.076], while significance was only noted with flexed knees.
Morphometrics
In children with CP, mean knee flexion angle during scans was 9° (5°) in CP vs. 5° (4°) in TD (p = 0.015). Thus, similar L MTU were reached at different ankle angles due to altered knee alignments (Fig. 3). The midrange L MTU from CP (109.4 % shank length) corresponded to 23° (8°) and 25° (6°) plantarflexion in CP and TD.
Normalised muscle morphometrics during stretch. Data are group mean (1 SEM). *Significant differences between typically developing children (TD) and children with spastic cerebral palsy (CP) with p < 0.05 (**p < 0.01), and †significant differences between pre and post bracing in CP with p < 0.05 tested at minimum (Min), matched midrange (Mid) and maximum (Max) muscle–tendon unit length
Average L MTU–L FASC, L MTU–L TEND and L MTU–L MB relationships are plotted in Fig. 3. Detailed statistics can be found in Table 2. Prior to bracing, the total MTU extensibility in CP with respect to controls was reduced by 22 % (p = 0.002). As illustrated in Fig. 4, this was accompanied by less fascicle (−32 %) and tendon (−34 %) extensibility (both p ≤ 0.014). L MB and L FASC were significantly shorter throughout the stretch (all p ≤ 0.035). L TEND was significantly longer at minimum and midrange L MTU stretch (both p ≤ 0.039). At midrange, L MB and L FASC were 7 % (p = 0.016) and 14 % (p = 0.032) shorter, while L TEND was 11 % (p = 0.013) longer. MT was thinner, most pronounced (12 %) during the minimum MTU stretch (p = 0.027), and FA appeared to be comparable between TD and CP children.
Extensibility of the muscle belly, fascicle and tendon. Data are group mean (1 SD). * Significant differences between typically developing children (TD) and children with spastic cerebral palsy (CP) with p < 0.05 (**p < 0.01). †Significant differences between pre and post bracing in CP with p < 0.05
After bracing, the L MTU, L MB and L TEND did not significantly change (all p ≥ 0.272), but L FASC was significantly shorter throughout the stretch (all p ≤ 0.035). At matched midrange L MTU stretch, 11 % of L FASC was lost with respect to baseline. Simultaneously, MT decreased by 8 %, reaching significance at maximum MTU stretch (p = 0.018), while FA showed minor change. No significant changes in fascicle and muscle extensibility were noted (p > 0.104), whereas tendon extensibility increased by 20 % (p = 0.017).
3D gait analysis
Results are shown in Table 3. Before bracing, children with CP walked 16 % slower while taking 13 % shorter steps than TD and landed with a significantly steeper foot contact (all p ≤ 0.001). Average constraints in knee extension (−3°) and dorsiflexion (−4°) in stance did not reach significance (p ≥ 0.102). Obstructions in dorsiflexion were more pronounced during swing (−5°, p = 0.004). Ankle moments in early stance were pathologically increased, whereas ankle moments and power used for propulsion were considerably diminished (all p ≤ 0.002). After bracing, walking speed significantly increased by 8 % (p = 0.014), while children tended to take longer steps (3 %, p = 0.068). Children landed with a significantly better foot-to-floor angle (p = 0.006) and the average pattern changed towards heel-toe gait. Dorsiflexion gains in stance failed to reach significance (+2°, p = 0.073), but showed significant increases in swing (+2°, p = 0.045). The pathologically increased ankle moment during early stance developed towards reference values (p < 0.001). While propulsive ankle moments were reduced (p = 0.013), ankle power was not significantly changed (p = 0.550).
Discussion
This study set out to provide information about gastrocnemius muscle morphometrics in children with CP before and after a period of ankle foot bracing while referencing to untreated typically developing (TD) peers. Our assumption was that the spastic medial gastrocnemius (MG) would change towards TD and lengthen after a period of ankle–foot bracing. However, no significant gains of muscle belly (L MB) or tendon (L TEND) length occurred and fascicle length (L FASC) further shortened while muscle bulk decreased. Nonetheless, on a joint level, significant increases in passive dorsiflexion were noted. This primarily affected dorsiflexion with knees flexed, but the majority of the children also gained dorsiflexion when assessed with extended knees. During gait, children walked faster, and in particular, dorsiflexion during swing, as well as the foot landing pattern improved.
Muscle morphometrics prior to bracing
Before bracing, shortening of the spastic MG L MB and L FASC was pronounced in CP and maximum values during stretch only approached minimum values of TD. This displays considerable atrophy among relatively high functioning, independently ambulant children and youth (GMFCS I and II) with CP. As described before, muscle thickness (MT) was less [9] and fascicle angle (FA) appeared to be similar [13, 14]. Shorter L FASC and L MB also agree with recent investigations [11, 12]. Besides, our data confirm that MG fascicles are less extensible than usual [32]. Therefore, it appears reasonable to assume that spastic MG fibres may lack sarcomeres in series or that they might contain longer, already drawn-out sarcomeres, as had been shown for forearm or hamstring muscle [16, 17]. Potentially, more connective tissue could also impede the actual extensibility of the fibres [17]. Whether these alterations are caused by changed muscle growth or result as a consequence of decreased loading and reduced physical activity remains a subject of controversy [33]. In contrast to L MB and L FASC, at midrange stretch, L TEND was longer than usual [10]. Even though L TEND at similar degrees of muscle–tendon unit (MTU) stretch was longer, its total extensibility seemed to be compromised. In summary, if clinicians or therapists want to improve MG muscle pathology in children with CP, growth of muscle belly in length and thickness, as well as longer L FASC, appear to be desirable goals. Longer L FASC with more sarcomeres in series could in principle promote function by increasing the muscle’s contractile velocity and enable a muscle to exert force over a larger joint RoM [34].
Muscle morphometrics after bracing
Conversely, after bracing, an additional 11 % in L FASC was lost at matched amounts of MTU stretch and MT decreased by 8 %. This is the first study to provide information about spastic calf morphometrics after brace wear. Previous investigations on the longitudinal change of calf muscle morphometrics were also done on invasive treatments with worse outcome: despite improving passive dorsiflexion, surgical gastrocnemius recessions induced shortening of L MB [35] and 32 % shortening of L FASC [36]. Botulinum toxin injections caused reductions in MT of ~12 % [37]. While we observed shorter L FASC, the L MB modifications seemed negligible. Due to its pinnated fibre arrangement, loss in L FASC may not be reflected by loss in L MB, if, as observed, the MT reduces too. Although we did not instrumentally assess the force-producing capability of the MG, these architectural deteriorations suggest that the muscle would have gotten weaker.
Potential causes for morphometric changes
A potential cause for shorter L FASC, and thus progressive muscle contracture, could be that muscle tissue indeed failed to keep up with bone growth [2]. For normalization, L FASC was set in relation to the shank length [11]. In TD children, MG L FASC usually grows in proportion with the tibia [38]. During the current intervention, the shank of children with CP grew by 1.8 %, while unscaled L FASC dropped by 0.3 cm. Hence, these atrophic changes do not solely expose a lack of scaling to bone growth.
Another reason for shorter L FASC could be adaptations of the tendon. Although no significant changes in fascicle and muscle extensibility were noted, the extensibility of the tendon increased. Still, we did not observe changes in L TEND defined as a straight line from the heel marker to the MTJ. However, in absence of instrumented measures for the applied tension during passive stretch, this measure ignores slack. Consequently, we generally underestimated L TEND at small degrees of MTU stretch and overestimated its extensibility. Slack is usually surpassed shortly beyond neutral ankle alignment in TD [32]. In our data, only 2–3 % of tendon extensibility in TD children would be noted above that point, which confirms previous reports about intrinsic tendon tissue strain [39]. Moreover, during maximum MTU stretch, when all slack is taken up, no changes in L TEND of children with CP were noted, which could suggest that no major changes in L TEND occurred. Assuming that the tendon could have initially gotten more compliant during bracing, such as observed in growing animals [23, 24], the spastic fascicles were unstrained, which can trigger loss of sarcomeres [21, 22] and would fit the reductions in L FASC. Although intrinsic tendon properties are cumbersome to measure, more detailed information is necessary to clarify this.
Worth mentioning, the MG tendon also integrates the run-out from the deep MG aponeurosis and the achilles tendon to which both gastrocnemius and soleus merge. With the soleus fascicles also attaching distal to the MG’s muscle–tendon junction (MTJ), the increase in MG tendon extensibility could reflect a more compliant soleus as well. This also explains the significant increase of passive dorsiflexion with the knee held in flexion. Most ultrasound research in CP is currently done on gastrocnemius morphometrics, probably due to its superficial position. Clearly, more information about the soleus architecture in equinus needs be gathered.
The current outcome could also be attributed to the bracing regime. Overall, the MG is highly susceptible to disuse atrophy [40]. Since ankle motion in the brace was also largely restricted, a possible reason for the loss in L FASC and the decreased MT could be decreased muscle ecxcursion, which is important in regulating sarcomere number in growing animals [41]. Besides, as all children likely slept with bent knees, the ankle–foot brace may have not provided sufficient stretch on the bi-articular gastrocnemius. Surely, a knee-ankle–foot brace would be logic to target gastrocnemius contracture. Sees and Miller [42] recently emphasised this, elsewise suspecting contracture of the gastrocnemius to worsen. Our results reinforce this. As a final point, considering that prior to bracing, average dorsiflexion with knees extended in the current study group was 2°, use of augmented force into further dorsiflexion seemed critical. Such an extensive bracing treatment is very demanding and may cause insufficient compliance. That may be one reason why below-knee casting or nighttime ankle–foot orthotics are often being used [7, 8].
Functional benefits of bracing
Next to improving passive dorsiflexion with flexed knees, this ‘positional’ bracing also prevented deterioration in passive dorsiflexion with the knee in extension in 76 % of the children (13 of 17). The average dorsiflexion gain of 4° with extended knees marginally failed to reach significance. In the past, below-knee serial casts have also been shown to only increase passive dorsiflexion with flexed knees [8]. Based on the progressive loss of passive dorsiflexion during CP childhood [6], these results appear to be a beneficial outcome for children with CP! More importantly, from a functional perspective, the children walked faster and their ankle kinematics improved primarily in swing. Positioning the foot better for landing can be vital to avoid tripping and to prevent mid-foot break deformities. Reduced ankle moments during early stance may display less pathological dynamic joint stiffness after bracing. However, the reduced moments for push-off may be a side effect, but are in accordance with reduced muscle thickness.
We think that these functional gains outweigh the atrophic effects on muscle morphometrics. Restoring dorsiflexion and normalizing muscle morphometrics may not necessarily occur in concert. By concurrently improving morphometrics, a larger or potentially more sustainable change in function may be achieved. Coordinative and neural aspects may of course also modulate the direct relations between morphometrics and function. These aspects should be content of future interventions. Most likely this would include activities such as calf strength training [43] or instrumented cyclic stretching [20].
Considerations for ultrasound scans
Ultrasound scans are frequently used to study muscle architecture in CP. To perform valid comparisons between TD and CP, morphometrics should be assessed at similar muscle states. Some studies extracted MG parameters at resting or neutral ankle position without detailed info on knee alignment or at PRoM limits only [13, 14, 37]. Recently, a common ankle angle was suggested [12]. Still, even at similar ankle alignment, our data shows that the MTU can be considerably shorter in CP. Albeit referencing to L MTU, we found no common overlap. Possibly, we could have done so when allowing for semi-flexed knees [12], but the MG would then be slightly off-tension. By using a calculation of the entire MTU path, we accounted for different knee angles during testing, but the issue of standardization may depend on patient positioning. MG scans are mostly done when lying prone [10, 11, 14, 20, 38], but also when lying supine [19] or when sitting [12]. The latter probably poses most difficulties to achieve straight knees in case of short hamstrings. With the current setup, it seemed best choice to compare TD at the average midrange L MTU of the children with CP.
Limitations
First, we investigated a convenience sample and can only speculate about untreated natural progression of contracture. The treatment duration was somewhat variable depending on the childrens’ outpatient attendance, and not every child received full-time bracing. Longer treatment duration explained 15 % of the loss in L FASC assessed by simple linear regression (R 2). Besides, effects on L FASC were not different between the bracing protocols (p = 0.580). In the future, the separate impact of daytime and nighttime orthotics should be quantified. Additionally, the applied tension during stretch was not instrumentally standardised. Nevertheless, it seems very unlikely that shorter L FASC after bracing could be attributed to consistently reduced manually applied tension, since L FASC was shorter during the entire MTU stretch.
Conclusions
To the best of our knowledge, this is the first study about calf morphometrics in CP after a non-invasive orthotic treatment. Prior to bracing, the children with CP had shorter and thinner MG muscle bellies, and shorter fascicles but longer distal tendons than controls. Positional ankle–foot braces significantly improved passive dorsiflexion with the knees flexed and improved the gait pattern of the children, but failed to improve MG morphometrics. Further shortened fascicles and thinner muscle bellies are likely due to the fact that bracing potentially decreased the MG excursion or kept the bi-articular muscle off-tension. Theoretically, braces may need to extend the knee if MG morphometric pathology is to be targeted. Promoting dorsiflexion and normalizing muscle morphometrics seems difficult to be accomplished in concert using traditional orthopaedic means such as surgery, botulinum toxin injections or brace wear in isolation. Consequently, there is a need for concomitant treatments that promote muscle growth.
Abbreviations
- CP:
-
Cerebral palsy
- MG:
-
Medial gastrocnemius
- TD:
-
Typically developing peers
- MTU:
-
Muscle-tendon unit
- MAS:
-
Modified Ashworth scale
- MTJ:
-
Muscle-tendon junction
- FA:
-
Fascicle angle
- L MTU :
-
Muscle-tendon unit length
- L FASC :
-
Fascicle length
- L MB :
-
Muscle belly length
- L TEND :
-
Tendon length
- GMFCS:
-
Gross motor function classification system
- PRoM:
-
Passive range of motion
- 3DGA:
-
3D gait analysis
References
Gracies JM (2005) Pathophysiology of spastic paresis. I. Paresis and soft tissue changes. Muscle Nerve 31(5):535–551
Novacheck TF, Gage JR (2007) Orthopedic management of spasticity in cerebral palsy. Childs Nerv Syst 23(9):1015–1031
de Gooijer‐van Groep KL, de Vlugt E, de Groot JH, van der Heijden-Maessen HC, Wielheesen DH, van Wijlen-Hempel RM, Arendzen JH, Meskers CG (2013) Differentiation between non-neural and neural contributors to ankle joint stiffness in cerebral palsy. J Neuroeng Rehabil 10:81
Goldstein M, Harper DC (2001) Management of cerebral palsy: equinus gait. Dev Med Child Neurol 43(8):563–574
Neptune RR, Burnfield JM, Mulroy SJ (2007) The neuromuscular demands of toe walking: a forward dynamics simulation analysis. J Biomech 40(6):1293–1300
Hägglund G, Wagner P (2011) Spasticity of the gastrosoleus muscle is related to the development of reduced passive dorsiflexion of the ankle in children with cerebral palsy: a registry analysis of 2,796 examinations in 355 children. Acta Orthop 82(6):744–748
Lee SJ, Sung IY, Jang DH, Yi JH, Lee JH, Ryu JS (2011) The effect and complication of botulinum toxin type a injection with serial casting for the treatment of spastic equinus foot. Ann Rehabil Med 35(3):344–353
McNee AE, Will E, Lin JP, Eve LC, Gough M, Morrissey MC, Shortland AP (2007) The effect of serial casting on gait in children with cerebral palsy: preliminary results from a crossover trial. Gait Posture 25(3):463–468
Barret R, Lichtwark G (2010) Gross muscle morphology and structure in spastic cerebral palsy: a systematic review. Dev Med Child Neurol 52(9):794–804
Wren TA, Cheatwood AP, Rethlefsen SA, Hara R, Perez FJ, Kay RM (2010) Achilles tendon length and medial gastrocnemius architecture in children with cerebral palsy and equinus gait. J Pediatr Orthop 30(5):479–484
Mohagheghi AA, Khan T, Meadows TH, Giannikas K, Baltzopoulos V, Maganaris CN (2008) In vivo gastrocnemius muscle fascicle length in children with and without diplegic cerebral palsy. Dev Med Child Neurol 50(1):44–50
Matthiasdottir S, Hahn M, Yaraskavitch M, Herzog W (2014) Muscle and fascicle excursion in children with cerebral palsy. Clin Biomech 29(4):458–462
Malaiya R, McNee AE, Fry NR, Eve LC, Gough M, Shortland AP (2007) The morphology of the medial gastrocnemius in typically developing children and children with spastic hemiplegic cerebral palsy. J Electromyogr Kinesiol 17(6):657–663
Shortland AP, Harris CA, Gough M, Robinson RO (2002) Architecture of the medial gastrocnemius in children with spastic diplegia. Dev Med Child Neurol 44(3):158–163
Noble JJ, Fry NR, Lewis AP, Keevil SF, Gough M, Shortland AP (2014) Lower limb muscle volumes in bilateral spastic cerebral palsy. Brain Dev 36(4):294–300
Lieber RL, Fridén J (2002) Spasticity causes a fundamental rearrangement of muscle-joint interaction. Muscle Nerve 25(2):265–270
Smith LR, Lee KS, Ward SR, Chambers HG, Lieber RL (2011) Hamstring contractures in children with spastic cerebral palsy result from a stiffer extracellular matrix and increased in vivo sarcomere length. J Physiol 589(10):2625–2639
Novak I, McIntyre S, Morgan C, Campbell L, Dark L, Morton N, Stumbles E, Wilson SA, Goldsmith S (2013) A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev Med Child Neurol 55(10):885–910
Theis N, Korff T, Kairon H, Mohagheghi AA (2013) Does acute passive stretching increase muscle length in children with cerebral palsy? Clin Biomech 28(9–10):1061–1067
Zhao H, Wu YN, Hwang M, Ren Y, Gao F, Gaebler-Spira D, Zhang LQ (2011) Changes of calf muscle-tendon biomechanical properties induced by passive-stretching and active-movement training in children with cerebral palsy. J Appl Physiol 111(2):435–442
Williams PE, Goldspink G (1978) Changes in sarcomere length and physiological properties in immobilized muscle. J Anat 127(3):459–468
Spector SA, Simard CP, Fournier M, Sternlicht E, Edgerton VR (1982) Architectural alterations of rat hind-limb skeletal muscles immobilized at different lengths. Exp Neurol 76(1):94–110
Tardieu C, Tabary JC, Tabary C, Huet de la Tour E (1977) Comparison of the sarcomere number adaptation in young and adult animals. Influence of tendon adaptation J Physiol (Paris) 73(8):1045–1055
Blanchard O, Cohen-Solal L, Tardieu C, Allain JC, Tabary C, Le Lous M (1985) Tendon adaptation to different long term stresses and collagen reticulation in soleus muscle. Connect Tissue Res 13(3):261–267
Gough M (2007) Serial casting in cerebral palsy: panacea, placebo, or peril? Dev Med Child Neurol 9:725
Bohannon R, Smith M (1987) Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 67(2):206–207
Stief F, Böhm H, Michel K, Schwirtz A, Döderlein L (2013) Reliability and accuracy in three-dimensional gait analysis: a comparison of two lower body protocols. J Appl Biomech 29(1):105–111
Bénard MR, Becher JG, Harlaar J, Huijing PA, Jaspers RT (2009) Anatomical information is needed in ultrasound imaging of muscle to avoid potentially substantial errors in measurement of muscle geometry. Muscle Nerve 39(5):652–665
Hof AL (1996) Scaling gait data to body size. Gait Posture 4:222–223
Gillett JG, Barrett RS, Lichtwark GA (2013) Reliability and accuracy of an automated tracking algorithm to measure controlled passive and active muscle fascicle length changes from ultrasound. Comput Methods Biomech Biomed Engin 16(6):678–687
Orendurff MS, Aiona MD, Dorociak RD, Pierce RA (2002) Length and force of the gastrocnemius and soleus during gait following tendo Achilles lengthenings in children with equinus. Gait Posture 15(2):130–135
Barber L, Barrett R, Lichtwark G (2011) Passive muscle mechanical properties of the medial gastrocnemius in young adults with spastic cerebral palsy. J Biomech 44(13):2496–2500
Gough M, Shortland AP (2012) Could muscle deformity in children with spastic cerebral palsy be related to an impairment of muscle growth and altered adaptation? Dev Med Child Neurol 54(6):495–499
Butterfield TA (2010) Eccentric exercise in vivo: strain-induced muscle damage and adaptation in a stable system. Exerc Sport Sci Rev 38(2):51–60
Fry NR, Gough M, McNee AE, Shortland AP (2007) Changes in the volume and length of the medial gastrocnemius after surgical recession in children with spastic diplegic cerebral palsy. J Pediatr Orthop 27(7):769–774
Shortland AP, Fry NR, Eve LC, Gough M (2004) Changes to medial gastrocnemius architecture after surgical intervention in spastic diplegia. Dev Med Child Neurol 46(10):667–673
Park ES, Sim E, Rha DW, Jung S (2014) Architectural changes of the gastrocnemius muscle after botulinum toxin type A injection in children with cerebral palsy. Yonsei Med J 55(5):1406–1412
Bénard MR, Harlaar J, Becher JG, Huijing PA, Jasper RT (2011) Effects of growth on geometry of gastrocnemius muscle in children: a three-dimensional ultrasound analysis. J Anat 219(3):388–402
Kawakami Y, Kanehisa H, Fukunaga T (2008) The relationship between passive ankle plantar flexion joint torque and gastrocnemius muscle and achilles tendon stiffness: implications for flexibility. J Orthop Sports Phys Ther 38(5):269–276
de Boer MD, Seynnes OR, di Prampero PE, Pisot R, Mekjavić IB, Biolo G, Narici MV (2008) Effect of 5 weeks horizontal bed rest on human muscle thickness and architecture of weight bearing and non-weight bearing muscles. Eur J Appl Physiol 104(2):401–407
Koh TJ, Herzog W (1998) Excursion is important in regulating sarcomere number in the growing rabbit tibialis anterior. J Physiol 508(1):267–280
Sees J, Miller F (2013) Overview of foot deformity management in children with cerebral palsy. J Child Orthop 7:373–377
McNee AE, Gough M, Morrissey MC, Shortland AP (2009) Increases in muscle volume after plantarflexor strength training in children with spastic cerebral palsy. Dev Med Child Neurol 51(6):429–435
Conflict of interest
All authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hösl, M., Böhm, H., Arampatzis, A. et al. Effects of ankle–foot braces on medial gastrocnemius morphometrics and gait in children with cerebral palsy. J Child Orthop 9, 209–219 (2015). https://doi.org/10.1007/s11832-015-0664-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-015-0664-x