Abstract
Purpose
Different treatment modalities have been utilized to treat unicameral bone cyst (UBC), but evidence has not been fully described to support one treatment over another and the optimal treatment is controversial. The aim of this quantitative systematic review was to assess the effectiveness of different UBC treatment modalities.
Methods
We utilized Pubmed to isolate retrospective studies on patients with UBC who received any kind of treatment. The included studies needed to have a minimum sample size of 15 patients, and have provided data on radiographic healing outcome.
Results
Sixty-two articles were selected for the meta-analysis from a total of 463 articles. The cumulative sample size was 3,211 patients with 3,217 UBC, and male to female ratio was 2.2:1. The summary or pool estimate of methylprednisolone acetate (MPA) injection resulted in a healing rate of (77.4 %) that was comparable to bone marrow injection (77.9 %). A higher healing rate was observed with MPA injection when inner wall disruption was performed. The pool estimate of bone marrow with demineralized bone matrix injection was high (98.7 %). UBC healing rate after surgical curettage was comparable whether autograft or allograft was utilized (90 %). UBC treatment with flexible intramedullary nails without curettage provided almost 100% healing rate, while continuous decompression with cannulated screws provided 89 % healing rate. Conservative treatment indicated a healing rate of 64.2, 95 % CI (26.7–101.8).
Conclusions
Active treatment for UBC provided variable healing rates and the outcomes were favorable relative to conservative treatment. Due to the heterogeneity of the studies and reporting bias, the interpretation of these findings should be handled with caution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
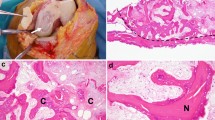
Unicameral bone cyst (UBC) is a benign lesion that mostly affects children and adolescents, and represents about 3 % of primary tumors in the first two decades of life [1–3]. UBC is also known as solitary or simple bone cyst and radiographically is seen as mildly expansile, lytic thin-walled bone lesion without periosteal reaction. The typical location is in the metaphysis adjacent to the growth plate of the tubular bones, mostly the humerus and femur [3]. Based on the distance between the cyst and the growth plate, UBC is classified as active when the distance is less than 5 mm, and latent when the distance is larger than 5 mm [4]. Other locations of UBC may include the pelvis, ribs, vertebrae and the tarsal bones, especially calcaneus. Several theories have been postulated to explain the origin of UBC, including trauma and inflammation; however, none has been conclusive [5].
The purpose of treatment is to restore bone strength, cortical thickness and obliteration of the cyst; and based on these criteria, healing of UBC was classified by Neer [3] and Capanna [6]. Complete filling of the cyst with restoration of cortical thickness was described as healed cyst. When small radiolucent areas persist with good bone strength, the cyst was described as partially healed. When the UBC had continuous bone lucency and thin or broken cortex and did not respond to the treatment, the cyst was considered persistent. Cyst recurrence was defined when a cavity and expansile remodelling and thinning of the cortex develop after full obliteration.
Various treatment modalities have been utilized to treat UBC, including surgical and nonsurgical interventions with variable reported healing rates. UBC has frequently been examined in the literature, yet no clearcut evidence supports one modality over another. The aim of this current study was to review the literature and examine the published articles referenced in Pubmed about the healing outcome of UBC management with every treatment modality. A qualitative systematic review was performed to screen all the articles and to select eligible articles for a meta-analysis on UBC treatment outcome. We postulated that treatment of UBC leads to better rates of cyst healing.
Materials and methods
Search techniques and terms:
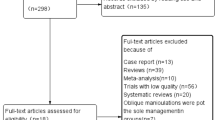
The studies were identified from Pubmed until 2012 using the following search terms: unicameral bone cyst, simple bone cyst and solitary bone cyst. The articles were searched by a single investigator (MK), but were reviewed by two investigators (MK, AK) independently and data were extracted during the review. The articles selected were reviewed and screened for pertinent information based on specific criteria (Fig. 1).
Eligibility criteria
The extracted articles were examined based on: (a) non-experimental retrospective studies on unicameral bone cyst in any anatomical location and any kind of treatment, (b) studies conducted in any geographic location, (c) studies with abstracts published in English, (d) studies that examined consecutive patients with sample size equal or greater than 15 patients, (e) studies with follow up more than 6 months, and (f) studies that demonstrated the radiographic outcome of treatment that can be classified into (healed, partially healed, persistence or recurrence).
Studies with sample size smaller than 15 were excluded in order to avoid sparse data bias; implying negative finding as a result of small sample size and limited statistical power. Case reports were excluded, as they did not examine consecutive patients. When more than one study was conducted in the same institution, the articles were examined for a possibility of duplicate report on the same patient sample, and data were retrieved from the most complete or recent study.
Study quality assessment
The included studies were assessed for study design, sampling techniques and data on patients’ characteristics and radiographic healing status. We determined the objectivity of each study, whether the aims or the purposes were clearly stated, and whether the studies presented factual results. We also examined for adequate statistical analysis and how the outcomes were determined. Studies were assessed for confounding factors that might have influenced the outcome and for any bias, including selection, information and misclassification biases. This quality assessment provided comparable measures to the preferred reporting for systematic reviews and meta-analysis (PRISMA statement) [7].
Study variables
Each study was identified by the first author’s last name and the year of publication. Study populations were stratified by sex, age at treatment, cyst location, cyst activity (active or latent), follow-up time and radiographic healing classified by Neer [3] and Capanna [6] criteria. The cohort of each study was categorized into two groups based on the final healing status of UBC: success—good outcome included healed and partially healed UBCs, and failure—poor outcome included persistence and recurrent UBCs.
Treatment groups
All treatment modalities were included in this study (conservative and surgical intervention). Studies that utilized injection as a method of treatment were categorized in one treatment group and subgroups were identified based on the material utilized for injection, including; methylprednisolone acetate (MPA) injection, bone marrow injection, combined MPA with bone marrow, combined bone marrow with demineralized bone matrix (DBM), and combined bone marrow with MPA and DBM. The technique of injection procedure was reviewed in each article to identify whether inner wall disruption was performed or not, and based on this criterion, every injection subgroup was subcategorized into injection with and without inner wall disruption. Studies on surgical treatment were examined and subgroups were identified, including: curettage only, curettage with bone graft (autograft versus allograft), curettage with bone substitution (calcium sulphate pellets, calcium phosphate pellets, Hydroxyapetite, ceramic substitute), curettage with myoplasty, cyst excision, flexible intramedullary nailing (IM nail) and continuous decompression with cannulated screws.
Comparative studies
Retrospective comparative studies that presented outcome of different treatment modalities were selected for further evaluation by combining the patients of each treatment group. Comparative assessment performed included: MPA vs. bone marrow injection, MPA injection with vs. without inner wall disruption, curettage with autograft vs. curettage with allograft, MPA injection vs. curettage with autograft, MPA injection vs. curettage with allograft.
Anatomical location
We identified the studies that provided a list of UBC cases demonstrating age, sex, cyst location treatment modality and radiographic healing outcome. The UBC cases were categorized based on the anatomic location for further assessment.
Sample size and power estimation
Four hundred and sixty-three articles published between 1942 and 2012 were identified for the qualitative systematic review. The number of studies included in the quantitative systematic review (meta-analysis or quantitative evidence synthesis) was represented by K = 62. The combination of study sizes (UBC) that constituted this meta-analysis was represented by n = 3,217 cysts. To estimate the power of this meta-analysis, we used 95 % confidence interval (5 % error), effect size of 20 % (0.2), and a random effect meta-analytic technique (DerSimonian and Laird). With these parameters, and with the combined sample sizes from the individual studies (n) for each treatment group, we obtained sufficient power (>80 %) to detect a difference between success (good) and failure (poor) outcomes in terms of UBC healing.
Statistical analysis
Frequency and percentages were employed to summarize nominal variables, while mean and standard deviation were used to describe the continuous variables, including age and follow-up.
We tested the hypotheses to determine the effectiveness of different treatment modalities. Both the fixed method of Peto and Mantel–Haenszel, and the random effect method of Dersimonian-Laird meta-analytic techniques were utilized. The fixed effect method was applicable to the summary point estimate when the studies that constituted the meta-analysis were assessed to be homogenous (implying heterogeneity test I with a significance level >0.05). Unless the homogeneity test was performed, the fixed method was inapplicable. The random effect method was utilized when the homogeneity assumption was not met.
The significance level was <0.05 and all tests were two-tailed. All analyses were performed using STATA 12.0 (StataCorp LP, College Station, TX).
Results
The results of this meta-analysis consisted of two parts, descriptive and inferential. Four hundred and sixty-three articles were identified for the qualitative systematic review. Sixty-two articles were eligible for the quantitative systematic review [3, 6, 8–67]. The rest of the articles were excluded, including: 97 articles that were not in English or French [68–164], one randomized clinical trial [165], one prospective study [166], seven case series [167–173], 174 case reports [2, 174–346], 10 basic science articles [5, 347–355], 26 articles that did not discuss UBC treatment [1, 356–380], 17 articles that did not represent clear data on healing [381–397], 18 review articles [4, 398–414], one article that was a reprint [415], three commentary articles [416–418], 36 articles with a sample size smaller than 15 [419–454], and ten articles with possibility of shared cohort [455–464] (Fig. 1).
The 62 studies of the meta-analysis generated 3,211 patients with 3,217 UBCs. There were 1,709 boys and 765 girls. While some studies did not provide enough data on gender and the proportions did not add up to 100 %, the estimated male to female ratio was 2.2:1. The clinical presentation was with a pathologic fracture in 1,107 UBCs, pain in 204 cysts, and incidental finding in 133 UBCs (the clinical presentation was not specified in all studies). Seven hundred and twenty-four UBC were classified as active and 535 cysts were latent. The overall average age at treatment was 10.9 ± 2.9 years, and the average follow up was 6.1 ± 4.2 years (not all the studies provided data on age at surgery and follow-up).
The most common location of UBC was in the humerus (59.2 %), followed by the femur (25.9 %). The calcaneus was affected in 6 %, the tibia in 4 %, the fibula in 1.5 %, the radius in 1.1 %, the pelvis in 0.9 %, and the other locations were affected in 1.4 % (Table 1).
Based on radiographic healing classification, 2,448 UBCs (76.1 %) were classified as healed or partially healed (success), while 769 cysts (23.9 %) were classified as persistent or recurrent (failure).
Treatment
Primarily three treatment modalities were assessed; injection, surgery and conservative treatment (observational management) (Table 2). Overall injection was utilized in 1,370 cysts. Of the injection cases, 1,128 cysts were treated with MPA, while 114 cysts were injected with bone marrow. Surgical treatment included several surgical techniques as presented in Table 2. Curettage as a separate treatment was done in 31 UBCs. Curettage with allograft was performed in 353 UBCs, while 128 cysts were treated with curettage and autograft. Flexible IM nail was used in 205 UBCs and cannulated screws for continuous decompression were utilized in 61 UBCs. Conservative treatment implying observational management was utilized in 149 cysts.
Comparative studies
We examined the studies that compared the healing outcome of MPA injection with bone marrow injection [19, 26, 38, 39]. Of 206 patients in this protocol, a higher rate of success was observed in bone marrow injection compared to MPA injection (Fig. 2). Only one study examined MPA injection outcome with and without inner wall disruption [47] and the outcome success was comparable. Five studies examined the difference in outcome of curettage with allograft compared to autograft [3, 9, 14, 25, 27], and the success rate was comparable (Fig. 3). Five articles compared the outcome of MPA injection relative to surgical curettage with autograft [14, 19, 25, 27, 47] (Fig. 4), and five articles also examined the outcome of MPA injection compared to surgical curettage with allograft [14, 25, 27, 29, 37] (Fig. 5).
Outcome of treatment based on the anatomic location
The outcome of treatment based on UBC anatomic location was also examined, including (humerus, femur, calcaneus, fibula, tibia and radius). Some studies did not present healing status for each anatomic location of the cyst; therefore, the numbers and percentages did not add up to 100 % of the total number of UBC of the meta-analysis. Tables 3, 4, 5, and 6 present the findings on healing outcome stratified by sex, activity level and treatment modalities. A few studies examined the fibula, radius, tibia and pelvic locations.
Quantitative results (Pool estimates)
Table 7 illustrates the percentages and 95 % CI of each treatment modality representing the successful outcome (healed and partially healed UBC). The combination of studies in almost all the categories of the meta-analysis indicated satisfactory healing of UBC after each specific treatment. The summary or pool estimate of overall injection category was 81.3, 95 % CI (77.9–84.8), implying a statistically significant 81 % success rate for overall injection (p < 0.05). MPA injection resulted in a healing rate of 77.4, 95 % CI (72.7–82.2) (Fig. 6). The effect of inner wall disruption with MPA injection was examined and higher healing rate was observed when the disruption was performed. The pool estimate of bone marrow injection was comparable to MPA injection, 77.9, 95 % CI (65.9–89.9) (Fig. 7). Only one study reported on the outcome of bone marrow injection with inner wall disruption and success rate was 78.6 % [39]; therefore, no pool estimate was performed for bone marrow injection with inner wall disruption. The pool estimate of bone marrow with DBM injection was high, 98.7, 95 % CI (95.7–101.7) relative to injection with either MPA or bone marrow.
Surgical curettage was examined according to the utilization of bone graft or bone substitute, and the pool estimates of all the subcategories were comparable. Other surgical managements were also assessed, including cyst excision, continuous decompression with IM nail or cannulated screws, and cyst wall trepanation (Table 3). The pool estimate of conservative treatment was 64.2, 95 % CI (26.7–101.8) (Fig. 8).
Discussion
The effect of various treatment modalities on UBC management has been repeatedly examined in the literature, but the natural history of UBC and the optimal treatment remain unclear. The conventional knowledge about UBC is that it is a self-limited benign bone lesion [370]; however, the healing rate without treatment (observational management) is undetermined and most of the studies in this review demonstrated better results with active treatment. With the purpose to better understand the role of each treatment modality of UBC, we aimed in this quantitative systematic review to synthesize the literature and assess the natural history of UBC, as well as evaluate the various treatment methods.
The main purpose of meta-analysis is to improve the power by combining homogeneous studies and arriving at a summary effect or pool estimate. We performed both systematic review and meta-analysis to examine the effect of several treatment modalities on UBC. Specifically, we tested the hypothesis regarding the effectiveness of different treatment modalities on UBC healing. Our meta-analysis has some relevant findings: overall active treatment improves UBC healing, regardless of anatomic site and the type of treatment compared to observational management. In this meta-analysis, observational treatment leads to a healing rate of 64 %. However, due to the variability of the studies, the rate of healing after conservative treatment can be as low as 27 % and as high as 100 %. The healing rate after conservative treatment varied in different anatomic location. Higher failure rate of conservative treatment was found in calcaneal and humeral UBCs compared to femoral UBCs (although the number of femoral UBCs was small, 11 out of 211 cysts were treated conservatively).
The indication to treat UBC is to prevent a pathologic fracture and to manage symptoms, especially pain. Historically, surgical curettage and cyst excision with bone graft were the optimal choices to treat UBCs. Based on this meta-analysis, UBC healing rate after surgical curettage was comparable (90 %) whether autograft or allograft was utilized. The utilization of MPA in the treatment of UBC was first described by Scaglietti [454]. The role of MPA is to reduce the production of cyst fluid from the inner wall cyst, which enhances bone healing [352]. On the other hand, bone marrow injection was proposed to accelerate healing, given the osteogenic potential of red marrow [465, 466]. In this meta-analysis, the healing rate of UBC was comparable after injection with bone marrow or MPA (77 %). The healing rate after MPA or bone marrow injection was higher (almost double) in our meta-analysis compared to the results demonstrated by Wright et al. [165] in a randomized (prospective) clinical trial. This might be a result of failure to report unsuccessful outcomes in studies of retrospective design (reporting bias). Both the randomized study by Wright et al. [165] and our meta-analysis demonstrated comparable healing rate after MPA injection and bone marrow injection.
The utilization of IM nails or cannulated screws for the treatment of UBC was also described, and the rationale was that theoretically, UBCs develop from venous blockage and increase of fluid pressure inside the cyst [5]. In this meta-analysis, we found that treatment with IM nails without curettage provided almost 100 % healing rate of UBC in long bones. IM nails were described as an efficient acute treatment for UBCs that present with a fracture [11, 16, 67]. Cyst wall drilling and trepanation also provided a healing rate of almost 100 %; however, this healing rate was estimated based on only two studies [9, 49].
Although this meta-analysis may be interpreted as a comparison between different treatment modalities such as MPA and bone marrow injection, this is incorrect. Studies that tested hypothesis with respect of comparative effectiveness of treatment were not available; therefore, we were unable to use formal meta-analysis method to examine the differences in outcomes of treatment with different treatment modalities. Future studies designed to compare different modalities of treatment are recommended, and will provide the opportunity for these questions to be addressed.
Our systematic review is limited in the sense that different studies presented with different sampling designs and different study protocols. For example, data were not available on MPA dosage that was utilized for treatment. Also, the variability of surgical techniques and type of bone graft (autograft or allograft) has a tendency of introducing a confounding that may lead to bias in our outcomes estimation and interpretation. In addition, we were unable to examine the need for further intervention and recurrence rate in each treatment modality, as data were not clearly specified in the reviewed articles. Also UBC activity as described by the distance from the growth plate may be an important factor that may affect on cyst healing after different treatment modalities. Some of the studies provided data on cyst activity, but only a few of these provided data on the outcome of treatment stratified by cyst activity. The other limitations are the heterogeneity of the patients in terms of UBC anatomic locations, cyst size, sex variability, and duration of treatment and follow-up. We could have performed subgroup meta-analysis in terms of the impact of sex or anatomic site of the UBC on the outcome implying cyst healing. However, since many studies did not provide relevant data, performing such subgroup analysis could have ended up in biased results regarding such effects. Considering this inability to perform the observed subgroup analyses, we recommend future studies to provide complete data on patients’ sex and specific anatomic location.
Heterogeneity remains an important factor to be considered in the conduct and interpretation of meta-analysis. There is no meta-analytic study without some influence of heterogeneity. Several studies used in our meta-analysis showed significant heterogeneity; however, our meta-analysis is not completely driven by this variability. A meta-analytic finding could be reliable and valid despite heterogeneity when appropriate analysis is used in the summary estimate. We applied the random effect meta-analysis given the heterogeneity of studies included in this meta-analysis. Consequently, by adjusting for the differences between studies with the random effect method approach, we have produced relatively standard and valid meta-analytic results on the effect of treatments on the outcomes of UBC. Whereas qualitative systematic review is not intended to quantify results of reviewed literature, we attempted to summarize proportions with regard to UBC healing, and caution is recommended in the interpretation of the results of our systematic review.
We are unaware of previous meta-analysis in this direction to either support or negate our findings. Clinicians will be interested in assessing the possibility of the results of this meta-analysis in developing guidelines regarding the treatment of UBC. Our meta-analysis of published literature on UBC treatment indicates improved healing rates among treated patients relative to the observational management. Healing rate was found to be comparable in studies that utilized bone marrow injection or MPA, and higher rate of healing was found when DBM was added. Surgical curettage resulted in healing rate of 90 % with the utilization of autograft, allograft or any bone substitution material. Healing rate was also high with the utilization of IM nails.
References
Boseker EH, Bickel WH, Dahlin DC (1968) A clinicopathologic study of simple unicameral bone cysts. Surg Gynecol Obstet 127(3):550–560
Cohen J (1970) Etiology of simple bone cyst. J Bone Jt Surg Am 52(7):1493–1497
Neer CS, Francis KC, Marcove RC, Terz J, Carbonara PN (1966) Treatment of unicameral bone cyst. A follow-up study of one hundred seventy-five cases. J Bone Jt Surg Am 48(4):731–745
Jaffe H, Lichtenstein L (1942) Solitary unicameral bone cyst-with emphasis on the roentgen picture the pathologic appearance and the pathogenesis. Arch Surg 44:1004–1025
Cohen J (1960) Simple bone cysts. Studies of cyst fluid in six cases with a theory of pathogenesis. J Bone Jt Surg Am 42-A:609–616
Capanna R, Dal MA, Gitelis S, Campanacci M (1982) The natural history of unicameral bone cyst after steroid injection. Clin Orthop Relat Res 166:204–211
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Sponer P, Urban K, Urbanova E, Karpas K, Mathew PG (2009) Behaviour of nonresorbable bioactive glass-ceramic implanted into long bone defects: comparison with cancellous allografts. Arch Orthop Trauma Surg 129(10):1353–1360
Baker DM (1970) Benign unicameral bone cyst. A study of forty-five cases with long-term follow up. Clin Orthop Relat Res 71:140–151
Bensahel H, Aigrain Y, Desgrippes Y (1982) Evaluation of the treatment of the unicameral bone cyst in children. J Chir (Paris) 119(5):319–323
Roposch A, Saraph V, Linhart WE (2000) Flexible intramedullary nailing for the treatment of unicameral bone cysts in long bones. J Bone Jt Surg Am 82-A(10):1447–1453
Bovill DF, Skinner HB (1989) Unicameral bone cysts. A comparison of treatment options. Orthop Rev 18(4):420–427
Chuo CY, Fu YC, Chien SH, Lin GT, Wang GJ (2003) Management strategy for unicameral bone cyst. Kaohsiung J Med Sci 19(6):289–295
Oppenheim WL, Galleno H (1984) Operative treatment versus steroid injection in the management of unicameral bone cysts. J Pediatr Orthop 4(1):1–7
Kanellopoulos AD, Yiannakopoulos CK, Soucacos PN (2005) Percutaneous reaming of simple bone cysts in children followed by injection of demineralized bone matrix and autologous bone marrow. J Pediatr Orthop 25(5):671–675
Journeau P, Ciotlos D (2003) Treatment of solitary bone cysts by intra-medullary nailing or steroid injection in children. Rev Chir Orthop Reparatrice Appar Mot 89(4):333–337
Gakuu LN (1997) Solitary unicameral bone cyst. East Afr Med J 74(1):31–32
Graham JJ (1952) Solitary unicameral bone cyst; a follow-up study of thirty-one cases with proven pathological diagnoses. Bull Hosp Jt Dis 13(1):106–130
Kokavec M, Fristakova M, Polan P, Bialik GM (2010) Surgical options for the treatment of simple bone cyst in children and adolescents. Isr Med Assoc J 12(2):87–90
Pogorelic Z, Furlan D, Biocic M, Mestrovic J, Juric I, Todoric D (2010) Titanium intramedullary nailing for treatment of simple bone cysts of the long bones in children. Scott Med J 55(3):35–38
Rougraff BT, Kling TJ (2002) Treatment of active unicameral bone cysts with percutaneous injection of demineralized bone matrix and autogenous bone marrow. J Bone Jt Surg Am 84-A(6):921–929
de Palma L, Santucci A (1987) Treatment of bone cysts with methylprednisolone acetate. A 9 to 11 year follow-up. Int Orthop 11(1):23–28
Hou HY, Wu K, Wang CT, Chang SM, Lin WH, Yang RS (2010) Treatment of unicameral bone cyst: a comparative study of selected techniques. J Bone Jt Surg Am 92(4):855–862
Peltier LF, Jones RH (2004) Treatment of unicameral bone cysts by curettage and packing with plaster-of-Paris pellets. 1978. Clin Orthop Relat Res 422:145–147
Farber JM, Stanton RP (1990) Treatment options in unicameral bone cysts. Orthopedics 13(1):25–32
Cho HS, Oh JH, Kim HS, Kang HG, Lee SH (2007) Unicameral bone cysts: a comparison of injection of steroid and grafting with autologous bone marrow. J Bone Jt Surg Br 89(2):222–226
Pentimalli G, Tudisco C, Scola E, Farsetti P, Ippolito E (1987) Unicameral bone cysts—comparison between surgical and steroid injection treatment. Arch Orthop Trauma Surg 106(4):251–256
Campanacci M, Capanna R, Picci P (1986) Unicameral and aneurysmal bone cysts. Clin Orthop Relat Res 204:25–36
Brecelj J, Suhodolcan L (2007) Continuous decompression of unicameral bone cyst with cannulated screws: a comparative study. J Pediatr Orthop B 16(5):367–372
Masquijo JJ, Baroni E, Miscione H (2008) Continuous decompression with intramedullary nailing for the treatment of unicameral bone cysts. J Child Orthop 2(4):279–283
De SN, Andreacchio A (2006) Elastic stable intramedullary nailing is the best treatment of unicameral bone cysts of the long bones in children? Prospective long-term follow-up study. J Pediatr Orthop 26(4):520–525
Glanzmann MC, Campos L (2007) Flexible intramedullary nailing for unicameral cysts in children’s long bones : level of evidence: lV, case series. J Child Orthop 1(2):97–100
Di BC, Dozza B, Frisoni T, Cevolani L, Donati D (2010) Injection of demineralized bone matrix with bone marrow concentrate improves healing in unicameral bone cyst. Clin Orthop Relat Res 468(11):3047–3055
Teoh KH, Watts AC, Chee YH, Reid R, Porter DE (2010) Predictive factors for recurrence of simple bone cyst of the proximal humerus. J Orthop Surg (Hong Kong) 18(2):215–219
Spence KF Jr, Bright RW, Fitzgerald SP, Sell KW (1976) Solitary unicameral bone cyst: treatment with freeze-dried crushed cortical-bone allograft. A review of one hundred and forty-four cases. J Bone Jt Surg Am 58(5):636–641
Fahey JJ, O’Brien ET (1973) Subtotal resection and grafting in selected cases of solitary unicameral bone cyst. J Bone Jt Surg Am 55(1):59–68
Sung AD, Anderson ME, Zurakowski D, Hornicek FJ, Gebhardt MC (2008) Unicameral bone cyst: a retrospective study of three surgical treatments. Clin Orthop Relat Res 466(10):2519–2526
Canavese F, Wright JG, Cole WG, Hopyan S (2011) Unicameral bone cysts: comparison of percutaneous curettage, steroid, and autologous bone marrow injections. J Pediatr Orthop 31(1):50–55
Chang CH, Stanton RP, Glutting J (2002) Unicameral bone cysts treated by injection of bone marrow or methylprednisolone. J Bone Jt Surg Br 84(3):407–412
Zamzam MM, Abak AA, Bakarman KA, Al-Jassir FF, Khoshhal KI, Zamzami MM (2009) Efficacy of aspiration and autogenous bone marrow injection in the treatment of simple bone cysts. Int Orthop 33(5):1353–1358
Scaglietti O, Marchetti PG, Bartolozzi P (1982) Final results obtained in the treatment of bone cysts with methylprednisolone acetate (depo-medrol) and a discussion of results achieved in other bone lesions. Clin Orthop Relat Res 165:33–42
Altermatt S, Schwobel M, Pochon JP (1992) Operative treatment of solitary bone cysts with tricalcium phosphate ceramic. A 1 to 7 year follow-up. Eur J Pediatr Surg 2(3):180–182
James AG, Coley BL, Higinbotham NL (1948) Solitary, unicameral, bone cyst. Arch Surg 57(1):137–147
Norman-Taylor FH, Hashemi-Nejad A, Gillingham BL, Stevens D, Cole WG (2002) Risk of refracture through unicameral bone cysts of the proximal femur. J Pediatr Orthop 22(2):249–254
Docquier PL, Delloye C (2004) Autologous bone marrow injection in the management of simple bone cysts in children. Acta Orthop Belg 70(3):204–213
Hagberg S, Mansfeld L (1967) The solitary bone cyst. A follow-up study of 24 cases. Acta Chir Scand 133(1):25–29
Mylle J, Burssens A, Fabry G (1992) Simple bone cysts. A review of 59 cases with special reference to their treatment. Arch Orthop Trauma Surg 111(6):297–300
Inoue O, Ibaraki K, Shimabukuro H, Shingaki Y (1993) Packing with high-porosity hydroxyapatite cubes alone for the treatment of simple bone cyst. Clin Orthop Relat Res 293:287–292
Shinozaki T, Arita S, Watanabe H, Chigira M (1996) Simple bone cysts treated by multiple drill-holes. 23 cysts followed 2–10 years. Acta Orthop Scand 67(3):288–290
Carrata A, Garbagna P, Mapelli S, Zucchi V (1983) The treatment of simple bone cysts by topical infiltrations of methylprednisolone acetate: technique and results. Eur J Radiol 3(1):3–8
Hunt KJ, Bergeson A, Coffin CM, Randall RL (2009) Percutaneous curettage and bone grafting for humeral simple bone cysts. Orthopedics 32(2):89
Gray DH (1971) Simple bone cysts: results of a pilot survey. Aust N Z J Surg 41(2):169–173
Schreuder HW, Conrad EU III, Bruckner JD, Howlett AT, Sorensen LS (1997) Treatment of simple bone cysts in children with curettage and cryosurgery. J Pediatr Orthop 17(6):814–820
McKay DW, Nason SS (1977) Treatment of unicameral bone cysts by subtotal resection without grafts. J Bone Jt Surg Am 59(4):515–519
Hashemi-Nejad A, Cole WG (1997) Incomplete healing of simple bone cysts after steroid injections. J Bone Jt Surg Br 79(5):727–730
Park IH, Micic ID, Jeon IH (2008) A study of 23 unicameral bone cysts of the calcaneus: open chip allogeneic bone graft versus percutaneous injection of bone powder with autogenous bone marrow. Foot Ankle Int 29(2):164–170
Yildirim C, Akmaz I, Sahin O, Keklikci K (2011) Simple calcaneal bone cysts: a pilot study comparing open versus endoscopic curettage and grafting. J Bone Jt Surg Br 93(12):1626–1631
Smith RW, Smith CF (1974) Solitary unicameral bone cyst of the calcaneus. A review of twenty cases. J Bone Jt Surg Am 56(1):49–56
Polat O, Saglik Y, Adiguzel HE, Arikan M, Yildiz HY (2009) Our clinical experience on calcaneal bone cysts: 36 cysts in 33 patients. Arch Orthop Trauma Surg 129(11):1489–1494
Bumci I, Vlahovic T (2002) Significance of opening the medullar canal in surgical treatment of simple bone cyst. J Pediatr Orthop 22(1):125–129
Tsuchiya H, Abdel-Wanis ME, Uehara K, Tomita K, Takagi Y, Yasutake H (2002) Cannulation of simple bone cysts. J Bone Jt Surg Br 84(2):245–248
Meyer JM, Burdet A (1979) Essential bone cyst and its therapy. Schweiz Med Wochenschr 109(19):714–719
Mik G, Arkader A, Manteghi A, Dormans JP (2009) Results of a minimally invasive technique for treatment of unicameral bone cysts. Clin Orthop Relat Res 467(11):2949–2954
Glowacki M, Ignys-O’Byrne A, Ignys I, Mankowski P, Melzer P (2010) Evaluation of volume and solitary bone cyst remodeling using conventional radiological examination. Skeletal Radiol 39(3):251–259
Immenkamp M, Ehrenbrink H, Knoche U (1982) Subperiosteal segmental resection and insertion of a fibula graft in the treatment of solitary bone cysts of the humerus. Arch Orthop Trauma Surg 100(2):107–114
Gennari JM, Merrot T, Legre B, Bergoin M (1996) The choice of treatment for simple bone cysts of the upper third of the femur in children. Eur J Pediatr Surg 6(2):95–99
Knorr P, Schmittenbecher PP, Dietz HG (2003) Elastic stable intramedullary nailing for the treatment of complicated juvenile bone cysts of the humerus. Eur J Pediatr Surg 13(1):44–49
Lischi DM (1984) Solitary cysts of the calcaneus with inclusion. Radiol Med 70(12):995–996
Zidkova H (1984) Solitary benign bone lesions. Cesk Radiol 38(4):276–290
Chigira M, Watanabe H, Arita S, Udagawa E (1983) Simple bone cyst–pathophysiology and treatment. Nihon Seikeigeka Gakkai Zasshi 57(8):759–766
Vrbicky B (1982) Solitary cyst of the calcaneous (author’s transl). Acta Chir Orthop Traumatol Cech 49(2):174–176
Sturz H, Hagena FW (1980) Solitary bone cysts with expansion throughout the complete humerus (author’s transl). Z Orthop Ihre Grenzgeb 118(6):923–926
Glowacki M, Struszynski J, Krasny I (2000) Solitary cyst of the calcaneus contemporary diagnostic possibilities: the results and treatment. Chir Narzadow Ruchu Ortop Pol 65(2):117–121
Sturz H, Witt AN (1979) Solitary bone cysts of the ulna (author’s transl). Arch Orthop Trauma Surg 94(2):105–108
Maranzana G (1979) Solitary osseous cyst in early childhood. Chir Organi Mov 65(1):75–80
Iwasaki H, Okamura Y, Hirano Y, Tagawa T, Murata M, Sato I (1979) Three cases of solitary bone cyst (author’s transl). Kyoto Daigaku Kokukagaku Kiyo 19:79–85
Korzh AA, Pankov EI, Kul’man LV (1978) Reliable and arguable points in the problem of the solitary bone cyst. Ortop Travmatol Protez 4:75–80
De Palma L (1978) Use of methylprednisolone acetate in the treatment of solitary bone cysts. Arch Putti Chir Organi Mov 29:341–351
Hauer G, Wilhelm K, Feldmeier C (1978) Solitary cyst of the distal radius. Handchirurgie 10(1):13–14
Korzh AA, Kul’man L, Matskevich ND, Pankov EI (1977) Therapeutic tactics in solitary bone cysts in children. Ortop Travmatol Protez 12:32–38
Koch W, Luy M, Solitary bone cysts (1977) A possible clinical contribution to their pathogenesis. Dtsch Zahnarztl Z 32(8):629–630
Kovacs A, Szabo G, Tatrai J, Toth E (1976) Simple bone cyst. Fogorv Sz 69(11):341–344
Aszodi K (1976) Data on the pathogenesis of solitary juvenile bone cysts (author’s transl). Arch Orthop Unfallchir 86(2):157–168
Dick W (1976) Solitary bone cysts in the foot. Chirurg 47(2):93–97
Melanotte PL, Pavanini G, Turra S (1975) Solitary bone cysts. Clin Ortop 26:70–86
Ozga A, Borkowski Z (1975) Results of treatment of solitary bone cysts. Chir Narzadow Ruchu Ortop Pol 40(2):261–267
Olechnowicz A, Tokarowski A, Zappa M (1974) Treatment of solitary bone cysts. Chir Narzadow Ruchu Ortop Pol 39(3):349–355
Goldschmidt H (1973) Healing and healing picture of the juvenile, solitary bone cyst. Helv Chir Acta 40(1):163–170
Carnevali G, Lattuada A (1973) Radiological signs of malignancy of solitary lesions of the skeleton. Minerva Med 64(54):2808–2827
Toth S, Gyarfas F, Perenyi A (1972) Solitary bone cysts. Monatsschr Unfallheilkd Versicher Versorg Verkehrsmed 75(7):326–330
Pagani A (1971) Solitary bone cysts. Minerva Med 62(89):4425–4427
Harada M, Nino M, Tanaka S (1970) Case of solitary bone cyst occurring in the carpale (the capitate bone). Seikei Geka 21(4):294–297
Stefanescu N (1968) Clinico-radiological observations on solitary primary bone cysts based on 5 cases. Rev Med Chir Soc Med Nat Iasi 72(2):447–450
Ito S (1968) Clinical and radiological studies of solitary bone cysts and benign giant cell tumors. Nihon Seikeigeka Gakkai Zasshi 42(3):153–167
Pollono F, Cavalli F (1967) On a case of solitary osseous cyst of the olecranon. Minerva Ortop 18(10):680–682
Kischinhevsky W (1967) Solitary bone cyst. Arq Bras Med 54(4):357–359
Jansen C (1967) On an atypical solitary bone cyst. Z Orthop Ihre Grenzgeb 103(1):109–111
Bednarek J, Hibner K (1967) Solitary bone cyst of the clavicle treated by excision and simultaneous bone grafting. Chir Narzadow Ruchu Ortop Pol 32(2):281–284
Brancadoro P (1966) n 3 cases of solitary osseous cyst of the tarsus. Nunt Radiol 32(10):1131–1141
Marchese GS, Grassi E, Tos L (1965) Solitary bone cysts. Minerva Chir 20(18):773–780
Gottschalk E (1965) Clinical observations on a solitary bone cyst. Zentralbl Chir 90(26):994–1002
Fukuma H (1965) A study of the solitary bone cyst. Igaku Kenkyu 35(3):91–128
Petraccia A, Volmaro N (1964) Simple bone cyst in an unusual site, comments on a case. Prensa Med Argent 31(51):299–303
Palkoska F (1964) On the treatment of solitary juvenile bone cysts and giant cell tumors. Zentralbl Chir 12(89):1909–1916
Romano A, Zaffaroni A (1964) Findings on recurrences of juvenile solitary bone cysts. Chir Ital 16:275–288
Salzer M, Salzer-Kuntschik M (1964) Giant cell tumor and solitary cyst of bone. Wien Klin Wochenschr 1(76):316–318
Itami Y, Kamatsu K, Yamashita E (1964) Radiography and histology of the solitary bone cyst. Rinsho Geka 19:640–645
Dubrov I, Buachidze OS, Fedotov PD (1964) Solitary bone cysts. Ortop Travmatol Protez 25:19–23
Monesi B, Florio L (1964) Recurrence in operated solitary bone cysts. Arch Putti Chir Organi Mov 19:175–189
Lievre CA, Calcagni V (1963) On a solitary bone cyst of the wing of the ilium. Minerva Ortop 14:615–617
Rai I, Kitano M (1963) Cases of solitary bone cyst in siblings. Nihon Seikeigeka Gakkai Zasshi 37:623–627
Calxagni V (1963) On juvenile solitary osseous cysts of the calcaneus. Minerva Ortop 14:556–560
Maeda F (1963) Studies on the solitary bone cyst with special reference to its pathogenesis. Nihon Seikeigeka Gakkai Zasshi 37:529–547
Malcapi C, Turrini PG (1963) Solitary osseous cysts of the calcaneus. Minerva Ortop 14:445–451
Krebs H (1963) The solitary juvenile bone cyst. Bruns Beitr Klin Chir 206:335–350
Skwarcz A (1963) Results of surgical treatment for solitary cyst of the long bones. Chir Narzadow Ruchu Ortop Pol 28:955–961
Lanzillo F (1956) Clinical aspects of solitary bone cysts. Riforma Med 70(2):39–42
Havranek P, Pesl T, Bartonicek J (2005) Pathologic proximal femoral fractures in children in an unicameral bone cyst. Acta Chir Orthop Traumatol Cech 72(5):282–286
Gal P, Ondrus S, Skvaril J, Straka M, Jochymek J, Planka L (2009) Synthetic biocompatible degradable material for juvenile bone cyst treatment. Acta Chir Orthop Traumatol Cech 76(6):495–500
Yu GX, Wei MM (2009) Proximal humeral interlocking antatomic plate for the treatment of proximal humeral fracture and bone cyst. Zhongguo Gu Shang 22(10):793
Makris V, Papavasiliou KA, Bobos M, Hytiroglou P, Kirkos JM, Kapetanos GA (2009) Simultaneous existence of unicameral bone cysts involving the femur and ischium. Acta Orthop Traumatol Turc 43(2):185–189
Hardes J, Schultheiss M, Gosheger G, Schulte M (2009) The juvenile bone cyst: treatment with continuous decompression using cannulated screws. Orthopade 38(3):256–262
Planka L, Ondrus S, Skvaril J, Stary D, Gal P (2008) The use of biodegradable materials in the management of bone cysts in children. Rozhl Chir 87(11):585–589
Tang HC, Wang ZH, Xiang M (2008) Allogeneic bone graft for the treatment of children’s bone cyst. Zhongguo Gu Shang 21(12):928–929
Teng HW, Zhang JS, Fang GJ (2008) Solitary bone cyst in both calcaneuses: a case report. Zhongguo Gu Shang 21(4):312
Liu H, Sun J, Wang Y, Yang X, Zhu E (2008) Repairing bone defects of benign bone neoplasm by grafting of bioactive glass combined with autologous bone marrow. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 22(11):1349–1353
Delling G, Sopta J (2008) Solitary bone cysts of the pelvis. A frequently misinterpreted entity. Pathologe 29(3):221–230
Sibinski M, Drobniewski M, Adamczyk E, Synder M (2007) Calcaneal solitary bone cysts in children. Chir Narzadow Ruchu Ortop Pol 72(3):211–213
Deng G, Ling Q, Li T (2007) Treatment of bone cyst by transplantation of autologous bone marrow combined with allograft bone. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 21(8):801–803
Guo S, Feng W, Jia Y (2007) Lyophilized small-segment allogeneic bone in repairing bone defect due to benign bone tumor and tumor-like lesions after resection and curettage. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 21(8):789–792
Wang E, Zhao Q, Zhang L (2006) Assessment of therapeutic results for simple bone cyst with percutaneous injection of autogenous bone marrow. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 20(9):925–927
Sulko J (2005) Solitary calcaneal bone cyst in children. Chir Narzadow Ruchu Ortop Pol 70(4):261–264
Yilmaz G, Aksoy MC, Alanay A, Yazici M, Alpaslan AM (2005) Treatment of simple bone cysts with methylprednisolone acetate in children. Acta Orthop Traumatol Turc 39(5):411–415
Kraus R, Schnettler R (2006) Distraction osteogenesis for adjusting humeral length difference due to premature closure of the proximal growth plate in a simple bone cyst. Chirurg 77(4):376–380
Zhang Y, Wang Y, Cheng J (2005) A long-term follow-up of treatment of adult unicameral bone cysts with allograft of lyophilized cancellous bone. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 198:600–602
Topuriia ZM, Bekauri LA, Makaridze DS (2005) Immunohistochemical characteristics of solitary bone cyst. Georgian Med News 118:56–58
Lewandowski B, Kulig T (2004) Simple bone cyst. Pol Merkur Lekarski 17(97):70–72
Huch K, Werner M, Puhl W, Delling G (2004) Calcaneal cyst: a classical simple bone cyst? Z Orthop Ihre Grenzgeb 142(5):625–630
Pogoda P, Priemel M, Catala-Lehnen P, Gebauer M, Rupprecht M, Adam G, Rueger JM, Amling M (2004) Simple bone cysts of the calcaneus. Differential diagnosis and therapy. Unfallchirurg 107(8):680–688
Cuenca EJ, Herrera RA, Gil AJ, Martinez Martin AA, Bregante BJ (2002) Simple bone cysts in childhood. Retrospective study of 15 cases and review of literature. Cir Pediatr 15(2):68–72
Kondoch A, Ewerbeck V, Bernd L (2002) Calcifying solitary bone cyst of the sacrum–A rare type of bone cyst and its unknown localisation, differential diagnosis and management. Z Orthop Ihre Grenzgeb 140(2):214–217
Beek FJ, Pruijs JE (2001) Diagnostic image (42). Solitary bone cyst of the left calcaneus. Ned Tijdschr Geneeskd 145(24):1155
Zietek P, Krolewski J, Bohatyrewicz A (1999) Aneurysmal bone cyst and solitary cyst of bone. Chir Narzadow Ruchu Ortop Pol 64(6):663–669
Seip GU, Thiele H (1999) Solitary juvenile cyst of the heel bone. Two case reports and review of the literature. Unfallchirurg 102(7):576–579
Glowacki M, Marciniak W, Krasny I, Szulc A (1998) The evaluation of selected risk factors of solitary bone cyst recurrence after its curretage and bone graft filling. Chir Narzadow Ruchu Ortop Pol 63(3):259–266
Glowacki M, Marciniak W (1997) Solitary bone cyst: etiology, diagnosis, therapy, clinical and radiologic evaluation of treatment results. Chir Narzadow Ruchu Ortop Pol 62(5):437–444
Wallenbock E, Pollanz H (1996) Solitary calcaneal cyst. Langenbecks Arch Chir 381(6):300–302
Amling M, Werner M, Posl M, Ritzel H, Welkerling H, Wening JV, Maas R, Winkler K, Heise U, Delling G (1996) Solitary bone cysts. Morphologic variation, site, incidence and differential diagnosis. Pathologe 17(1):63–67
Werner M, Heintz A, Delling G (1996) DNA cytometry of solitary and aneurysmal bone cysts and low malignancy and high malignancy central osteosarcomas. Current significance within the scope of morphologic diagnosis of intraosseous cystic and osteoblastic lesions. Pathologe 17(1):44–49
Mandys V, Mazanek J (1995) Solitary “traumatic” mandibular cyst. Cesk Patol 31(3):92–93
D’Angelo R, Mangoni Di Stefano ML, Arienzo A, Fazioli F, De Rosa V (1995) Unicameral cysts of the hindfoot. Diagnostic aspects and therapeutic implications. Radiol Med 89(3):335–338
Ludwig A, Merten HA (1995) Solitary bone cysts. The pathogenesis, clinical picture and therapy of solitary bone cysts. Schweiz Monatsschr Zahnmed 105(1):63–70
Maiat VV (1992) Zonography in solitary bone cysts. Khirurgiia (Mosk) 7–8:56–58
Sim E, Haid C (1990) Unicameral cyst of the calcaneus: surgical indications, biomechanical calculations and results of follow-up studies. Z Orthop Ihre Grenzgeb 128(6):623–631
Dietlein M, Zanella FE, de Feaux LW (1990) A unicameral aneurysmal bone cyst of the cervical spine. The differential diagnosis of a lateral cervical cyst. Rofo 152(6):732–733
Konera W, Okonski M, Gregosiewicz A (1990) Outcome of treating solitary osseous cyst with acetate methylprednisolone injections. Chir Narzadow Ruchu Ortop Pol 55(3):237–240
Sarria CA, Olivan GG, Fleta ZJ, Bello Nicolau ML, Jimenez VA, Bueno SM (1989) Solitary bone cyst in childhood: form of presentation and course in 13 cases. An Esp Pediatr 30(3):171–174
Berezhnoi AP, Nechvolodova OL, Vilenskii EV, Skipenko TT (1988) The outcome of the conservative treatment of solitary and aneurysmal bone cysts in children. Ortop Travmatol Protez 2:5–8
Pedersen NW, Schmidt SA (1986) Solitary bone cyst. Ugeskr Laeger 148(20):1195–1197
Sokolov TP (1986) Our experience treating a solitary bone cyst with mineralocorticoid preparations. Ortop Travmatol Protez 3:48–49
Schwenzer N, Ehrenfeld M, Roos R (1985) The so-called solitary bone cyst. Dtsch Zahnarztl Z 40(6):573–575
Fischer-Brandies E, Dielert E (1985) The diagnosis and therapy of solitary bone cysts. Dtsch Zahnarztl Z 40(6):570–572
Brandt M, Lehmann W (1985) Frequency and recurrence of solitary bone cysts. Dtsch Zahnarztl Z 40(6):566–569
Sleboda B (1985) Solitary cyst of the ilium. Chir Narzadow Ruchu Ortop Pol 50(6):513–515
Wright JG, Yandow S, Donaldson S, Marley L (2008) A randomized clinical trial comparing intralesional bone marrow and steroid injections for simple bone cysts. J Bone Jt Surg Am 90(4):722–730
Bielecki T, Cieslik-Bielecka A, Zelawski M, Mikusek W (2012) A side-effect induced by the combination of a demineralized freeze-dried bone allograft and leucocyte and platelet-rich plasma during treatment for large bone cysts: a 4-year follow-up clinical study. Transfus Apher Sci 47(2):133–138
Creyssel J (1955) Remote prognosis and treatment of solitary cysts of bone. Lyon Chir 50(1):98–103
Miles JE, Degenshein GA (1956) Solitary bone cysts. Am J Surg 91(2):170–177
Dotter WE (1959) Solitary unicameral bone cysts. Surg Clin North Am 39(3):857–864
Creyssel J (1954) Remote prognosis and treatment of solitary bone cysts. Acta Orthop Belg 20(5):463–476
Creyssel J, Barry P (1953) Postoperative recurrences in solitary non-parasitic cysts of bones. Lyon Chir 48(3):322–335
Tonino AJ, Linclau LA (1974) The solitary bone cyst. Arch Chir Neerl 26(2):131–138
Bodart A, Lesure J (1954) Surgical treatment of a solitary cyst in bones. Rev Med Nancy 1(79):905–910
Heublein GW, Baird CL (1948) Solitary unicameral bone cyst of right ilium; a case report. Am J Roentgenol Radium Ther 59(5):699–704
MacDonald KM, Swanstrom MM, McCarthy JJ, Nemeth BA, Guliani TA, Noonan KJ (2010) Exaggerated inflammatory response after use of recombinant bone morphogenetic protein in recurrent unicameral bone cysts. J Pediatr Orthop 30(2):199–205
Jerbi OS, Hafsa C, Ben GH, Hamza HA, Sassi N, Gannouni A (2008) Osteoid osteoma of the talus and simple bone cyst of the homolateral calcaneus. A rare association. Rev Chir Orthop Reparatrice Appar Mot 94(1):96–99
Goto T, Nemoto T, Okuma T, Kobayashi H, Funata N (2008) Mirror-image solitary bone cyst of the humerus in a pair of mirror-image monozygotic twins. Arch Orthop Trauma Surg 128(12):1403–1406
Gallagher TA, Lim-Dunham JE, Vade A (2007) CT findings of a unicameral calcaneal bone cyst containing a fluid-fluid level. Comput Med Imaging Graph 31(2):111–113
Lu AP, Hame SL (2005) Autologous osteochondral transplantation for simple cyst in the patella. Arthroscopy 21(8):1008
Wada R, Lambert RG (2005) Deposition of intraosseous fat in a degenerating simple bone cyst. Skeletal Radiol 34(7):415–418
Hanna SJ, Dasic D, Floyd A (2004) Simple bone cysts of the calcaneus: a report of five cases and a review of the literature. Foot Ankle Int 25(9):680–684
Coskun B, Akpek S, Dogulu F, Uluoglu O, Eken G (2004) Simple bone cyst in spinous process of the c4 vertebra. Am J Neuroradiol 25(7):1291–1293
Ogata T, Matsuda Y, Hino M, Kawatani Y, Sogabe H, Yamamoto H (2004) A simple bone cyst located in the pedicle of the lumbar vertebra. J Spinal Disord Tech 17(4):339–342
Baughman R, Johnson P, Abramson H (2003) Testing your diagnostic skills. Case no. 2. Traumatic (simple) bone cyst. Todays FDA 15(10):20–22
Amrani A, Dandane MA, el Alami Z, Miri A (2002) An unusual localization of solitary bone cyst in a child: the lumbar spine. Acta Orthop Belg 68(5):551–554
Cohen N, Keret D, Ezra E, Lokiec F (2002) Unusual simple bone cyst of the distal radius in a toddler. Isr Med Assoc J 4(2):137–139
Abdel-Wanis ME, Tsuchiya H, Minato H, Morinaga T, Yamamoto N, Tomita K (2001) Bilateral symmetrical cysts in the upper tibiae in a skeletally mature patient: might they be simple bone cysts? J Orthop Sci 6(6):595–600
Fujimoto T, Nakamura T, Ikeda T, Koyanagi E, Takagi K (2002) Solitary bone cyst in L-2. Case illustration. J Neurosurg 97(1 Suppl):151
Chang H, Park JB, Lee EJ (2001) Simple bone cyst of lamina of lumbar spine: a case report. Spine (Phila Pa 1976) 26(22):E531–E534
Komiya S, Inoue A (2000) Development of a solitary bone cyst–a report of a case suggesting its pathogenesis. Arch Orthop Trauma Surg 120(7–8):455–457
Bonnel F, Canovas F, Faure P (1999) Treatment of a simple bone cyst of the calcaneus by endoscopic curettage with cancellous bone injection. Acta Orthop Belg 65(4):528–531
Kitoh H, Nogami H (1999) A simple bone cyst containing secretory cells in its lining membrane in a patient with polyostotic fibrous dysplasia. Pediatr Radiol 29(6):481–483
Maas EJ, Craig JG, Swisher PK, Amin MB, Marcus N (1998) Fluid-fluid levels in a simple bone cyst on magnetic resonance imaging. Australas Radiol 42(3):267–270
Ehara S, Nishida J, Shiraishi H, Honda M, Abe M, Satoh T (1997) Eccentric simple bone cysts of the femoral neck in adults. Clin Imaging 21(4):233–236
Park CK, Cho KK, Lee SW, Jeon JS, Kang JK, Choi CR (1997) Simple bone cyst of the axis. Childs Nerv Syst 13(3):171–174
Margolis M, McLennan MK (1994) Radiology rounds. Simple bone cyst. Can Fam Physician 40:1535 1539–1541
Watanabe H, Arita S, Chigira M (1994) Aetiology of a simple bone cyst. A case report. Int Orthop 18(1):16–19
Seckler MM, Kenan S, Desimone D, Abdelwahab IF, Lewis MM (1993) Simple bone cysts: true recurrence after complete obliteration. Bull Hosp Jt Dis 53(4):50–53
Zamarin RI, Bosacco DN (1992) Answer please. Simple (unicameral) bone cysts. Orthopedics 15(8):989 993–89, 994
Hoeffel JC (1992) Simple bone cysts of the pelvis in adolescents. A report of four cases. J Bone Jt Surg Am 74(6):951–952
Abdelwahab IF, Hermann G, Norton KI, Kenan S, Lewis MM, Klein MJ (1991) Simple bone cysts of the pelvis in adolescents. A report of four cases. J Bone Jt Surg Am 73(7):1090–1094
Andrews JR, Tedder JL, Godbout BP (1991) Simple bone cyst of the distal tibia: a case for ankle arthroscopy. Arthroscopy 7(4):381–384
Jasan M, House JH, Brand JC (1990) Bilateral unicameral bone cysts in the hamate bones. J Hand Surg Am 15(6):888–890
Kragel PJ, Williams J, Garvin DF, Goral AB (1989) Solitary bone cyst of the radius containing Liesegang’s rings. Am J Clin Pathol 92(6):831–833
Sener RN (1989) Persistent femoral neck cysts in healed Legg-Perthes’ disease: a clue to the etiology of simple bone cyst? Pediatr Radiol 19(6–7):496–497
Nakamura T, Takagi K, Kitagawa T, Harada M (1988) Microdensity of solitary bone cyst after steroid injection. J Pediatr Orthop 8(5):566–568
Baruch A, Haas A, Lifschitz-Mercer B, Zeligowsky A (1987) Simple bone cyst of the metacarpal. J Hand Surg Am 12(6):1103–1106
Chigira M, Takehi Y, Nagase M, Arita S, Shimizu T, Shinozaki T (1987) A case of multiple simple bone cysts. With special reference to their etiology and treatment. Arch Orthop Trauma Surg 106(6):390–393
Cudia G, Gordeeff A, Panzoni E (1987) Solitary bone cyst. A case of dual mandibular and humeral location. Rev Stomatol Chir Maxillofac 88(1):31–35
Steinberg GG (1985) Ewing’s sarcoma arising in a unicameral bone cyst. J Pediatr Orthop 5(1):97–100
Kozlowski K, Masel J (1982) Simple bone cysts (report of two unusual cases). Australas Radiol 26(3):269–272
Blumberg ML (1981) CT of iliac unicameral bone cysts. AJR Am J Roentgenol 136(6):1231–1232
Mirra JM, Bernard GW, Bullough PG, Johnston W, Mink G (1978) Cementum-like bone production in solitary bone cysts. (so-called “cementoma” of long bones). Report of three cases. Electron microscopic observations supporting a synovial origin to the simple bone cyst. Clin Orthop Relat Res 135:295–307
Porat S, Lowe J, Rousso M (1978) Solitary bone cyst in the infant radius. A case report. Clin Orthop Relat Res 135:132–136
Lloyd ES, Press HC Jr (1978) Solitary bone lesion in a young adult. J Natl Med Assoc 70(9):681–682
Khermosh O, Weissman SL (1977) Coxa vara, avascular necrosis and osteochondritis dissecans complicating solitary bone cysts of the proximal femur. Clin Orthop Relat Res 126:143–146
Watanabe R (1977) Solitary bone cyst of the rib. Nihon Geka Hokan 46(1):68–71
Dawson EG, Mirra JM, Yuhl ET, Lasser K (1976) Solitary bone cyst of the cervical spine. Clin Orthop Relat Res 119:141–143
Nelson JP, Foster RJ (1976) Solitary bone cyst with epiphyseal involvement: a case report. Clin Orthop Relat Res 118:147–150
Gwinn JL, Lee FA (1976) Radiological case of the month: solitary bone cyst. Am J Dis Child 130(6):655–656
Samuelson KM, Momberger GL, Coleman SS (1975) Solitary bone cyst of the ilium. Report of two cases and a review of the literature. Rocky Mt Med J 72(10):443–445
Ogden JA, Griswold DM (1972) Solitary cyst of the talus. J Bone Jt Surg Am 54(6):1309–1310
Melrose RJ, Abrams AM, Nedleman G (1971) Multiple osseous dysplasia with concomitant simple bone cyst. J South Calif Dent Assoc 39(5):386–389
Fincher RL (1971) Radiographic diagnosis of a bone cyst of the humerus with pathological fracture. J Ark Med Soc 67(9):298
Tanghe W, Verstreken J, Mulier JC (1970) Solitary cyst of the ramus ossis pubis. Report of a case. Acta Orthop Belg 36(3):346–349
Broder HM (1968) Possible precursor of unicameral bone cysts. J Bone Jt Surg Am 50(3):503–507
Sato A, Watanabe R, Nishijima H (1966) A rare case of a solitary bone cyst of the patella. Nihon Geka Hokan 35(1):173–175
Idelberger K (1964) A solitary cyst of the 4th lumbar vertebra, operated on by abdominal approach in a 48 year old man. Rev Chir Orthop Reparatrice Appar Mot 50:385–387
Devan WT (1964) Solitary bone cyst with pathological fracture complicating otherwise normal pregnancy: report of a case and discussion of fractures in etiology, pathogenesis and treatment. Am Surg 30:109–114
Clark L (1962) The influence of trauma on unicameral bone cysts. Clin Orthop 22:209–214
Ufranc OE, Jones WN, Harris WH (1961) Humeral fractures through unicameral bone cysts. JAMA 28(178):410–413
Beller ML (1952) Solitary bone cyst in the humeral mid-shaft at age five years. Bull Hosp Jt Dis 13(1):212–216
McCort JJ (1951) Weekly clinicopathological exercises: unicameral bone cyst of ischium. N Engl J Med 245(10):379–81
Kliger M (1951) Solitary bone cyst of humerous, report of case and review of some current literature. Arch Pediatr 68(11):518–525
Wu KK (1993) A surgically treated unicameral (solitary) bone cyst of the talus with a 15-year follow-up. J Foot Ankle Surg 32(2):242–244
Brogdon BG, Cottrell WC, Nimityongskul P, Takhtani D (2006) A bullet-sired bone cyst. Skeletal Radiol 35(12):959–963
Akman S, Gur B, Seckin F, Ozturk I (2002) A case of bilateral unicameral bone cyst of the calcaneus and surgical outcome. Acta Orthop Traumatol Turc 36(3):265–267
Schwartz D (2009) An 11-year-old boy with ankle trauma: unicameral bone cyst of the calcaneus. Pediatr Ann 38(3):132–134
Giddings CE, Bray D, Stapleton S, Daya H (2005) Aneurysmal bone cyst of the spine. J Laryngol Otol 119(6):495–497
Sarierler M, Cullu E, Yurekli Y, Birincioglu S (2004) Bone cement treatment for aneurysmal bone cyst in a dog. J Vet Med Sci 66(9):1137–1142
Burr BA, Resnick D, Syklawer R, Haghighi P (1993) Fluid-fluid levels in a unicameral bone cyst: CT and MR findings. J Comput Assist Tomogr 17(1):134–136
Ruggieri P, Biagini R, Picci P (1987) Case report 437: solitary (unicameral, simple) bone cyst of the scapula. Skeletal Radiol 16(6):493–497
Chaudhary D, Bhatia N, Ahmed A, Chopra RK, Malik AC, Singh AK, Rao KS (2000) Unicameral bone cyst of the patella. Orthopedics 23(12):1285–1286
Vayego SA, De Conti OJ, Varella-Garcia M (1996) Complex cytogenetic rearrangement in a case of unicameral bone cyst. Cancer Genet Cytogenet 86(1):46–49
Marsh JI, Munk PL, Muller NL (1992) CT of a unicameral bone cyst in a rib. Br J Radiol 65(769):74–75
Weisel A, Hecht HL (1980) Development of a unicameral bone cyst. Case report. J Bone Jt Surg Am 62(4):664–666
Haims AH, Desai P, Present D, Beltran J (1997) Epiphyseal extension of a unicameral bone cyst. Skeletal Radiol 26(1):51–54
Lagier R, Kramar C, Baud CA (1987) Femoral unicameral bone cyst in a medieval child. Radiological and pathological study. Pediatr Radiol 17(6):498–500
Cebesoy O (2007) Intraosseous ganglion of the talus treated with the talonavicular joint approach without exposing the ankle joint. J Am Podiatr Med Assoc 97(5):424–427
Schopler SA, Lawrence JF, Johnson MK (1986) Lengthening of the humerus for upper extremity limb length discrepancy. J Pediatr Orthop 6(4):477–480
Sadler AH, Rosenhain F (1964) Occurrence of two unicameral bone cysts in the same patient. J Bone Jt Surg Am 46:1557–1560
Madiefsky L, Wasiak GA (1986) Outpatient surgery of a unicameral bone cyst of the calcaneus. J Foot Surg 25(1):73–77
Tynan JR, Schachar NS, Marshall GB, Gray RR (2005) Pathologic fracture through a unicameral bone cyst of the pelvis: CT-guided percutaneous curettage, biopsy, and bone matrix injection. J Vasc Interv Radiol 16(2 Pt 1):293–296
Madhavan P, Ogilvie C (1998) Premature closure of upper humeral physis after fracture through simple bone cyst. J Pediatr Orthop B 7(1):83–85
Shindell R, Connolly JF, Lippiello L (1987) Prostaglandin levels in a unicameral bone cyst treated by corticosteroid injection. J Pediatr Orthop 7(2):210–212
Stearns HC III (1986) Radiologic review: unicameral bone cyst with humeral fracture. Orthop Nurs 5(4):43–45
Tyler W, Frassica FJ, McCarthy EF (2002) Recurrence of a unicameral bone cyst after nineteen years. Orthopedics 25(4):435–436
Bowen RE, Morrissy RT (2004) Recurrence of a unicameral bone cyst in the proximal part of the fibula after en bloc resection. A case report. J Bone Jt Surg Am 86(1):154–158
Lee CC, Wei JD, How SW (2000) Simple bone cyst in cervical vertebral spinous process and laminae: report of a case. J Formos Med Assoc 99(1):54–58
Violas P, Salmeron F, Chapuis M, de Sales GJ, Bracq H, Cahuzac JP (2004) Simple bone cysts of the proximal humerus complicated with growth arrest. Acta Orthop Belg 70(2):166–170
Thomas LB, Steffensen T, Walling AK, Gilbert-Barness E (2008) Simple (unicameral) bone cyst of the calcaneus: a pathologic variant revisited. Fetal Pediatr Pathol 27(3):141–147
Nager GT (1986) Solitary (unicameral) cysts involving the temporal bone. Laryngoscope 96(6):666–674
Tausend ME, Marcus M (1959) Solitary unicameral bone cyst in a seven-week-old infant. N Engl J Med 260(3):129–131
Frankel SL, Chioros PG, Sidlow CJ (1988) Steroid injection of a unicameral bone cyst of the calcaneus: literature review and two case reports. J Foot Surg 27(1):60–65
Alvarez RG, Arnold JM (2007) Technical tip: arthroscopic assistance in minimally invasive curettage and bone grafting of a calcaneal unicameral bone cyst. Foot Ankle Int 28(11):1198–1199
McGlynn FJ, Mickelson MR, El-Khoury GY (1981) The fallen fragment sign in unicameral bone cyst. Clin Orthop Relat Res 156:157–159
Tsuchihara T, Arino H, Nemoto K, Amako M, Isaki H, Fujikawa K (2008) The growth rate of the humerus: long-term follow-up of treatment of solitary bone cyst of the proximal humerus using cannulated screws: a case report. J Pediatr Orthop B 17(3):145–147
Jordanov MI (2009) The “rising bubble” sign: a new aid in the diagnosis of unicameral bone cysts. Skeletal Radiol 38(6):597–600
Taxin RN, Feldman R (1975) The tumbling bullet sign in a post-traumatic bone cyst. Am J Roentgenol Radium Ther Nucl Med 123(1):140–143
Richkind KE, Mortimer E, Mowery-Rushton P, Fraire A (2002) Translocation (16;20)(p11.2;q13). sole cytogenetic abnormality in a unicameral bone cyst. Cancer Genet Cytogenet 137(2):153–155
Johnston CE, Fletcher RR (1986) Traumatic transformation of unicameral bone cyst into aneurysmal bone cyst. Orthopedics 9(10):1441–1447
Yildirim C, Mahirogullari M, Kuskucu M, Akmaz I, Keklikci K (2010) Treatment of a unicameral bone cyst of calcaneus with endoscopic curettage and percutaneous filling with corticocancellous allograft. J Foot Ankle Surg 49(1):93–97
Moed BR, LaMont RL (1982) Unicameral bone cyst complicated by growth retardation. J Bone Jt Surg Am 64(9):1379–1381
Prietto C, Orofino CF, Waugh TR (1977) Unicameral bone cyst in the scapula. Clin Orthop Relat Res 125:183–184
Bone LB, Johnston CE, Bucholz RW (1986) Unicameral bone cyst. Orthopedics 9(8):1155–1161
Yoho RM, Mandracchia VJ, Syvrud JN (1996) Unicameral bone cyst. An unusual complication. J Am Podiatr Med Assoc 86(5):236–238
Shulman HS, Wilson SR, Harvie JN, Cruickshank B (1977) Unicameral bone cyst in a rib of a child. Am J Roentgenol 128(6):1058–1060
Grumbine NA, Clark GD (1986) Unicameral bone cyst in the calcaneus with pathologic fracture. A literature review and case report. J Am Podiatr Med Assoc 76(2):96–99
Keret D, Kumar SJ (1987) Unicameral bone cysts in the humerus and femur in the same child. J Pediatr Orthop 7(6):712–715
Hresko MT, Miele JF, Goldberg MJ (1988) Unicameral bone cyst in the scapula of an adolescent. Clin Orthop Relat Res 236:141–144
Ehrlich MG, Chaglassian JH (1974) Unicameral bone cyst in the scapula. Clin Orthop Relat Res 103:80–81
Tsirikos AI, Bowen JR (2002) Unicameral bone cyst in the spinous process of a thoracic vertebra. J Spinal Disord Tech 15(5):440–443
Head SA (1984) Unicameral bone cyst located in metacarpal bone: report of a case. J Am Osteopath Assoc 84(4):372–373
Snell BE, Adesina A, Wolfla CE (2001) Unicameral bone cyst of a cervical vertebral body and lateral mass with associated pathological fracture in a child. Case report and review of the literature. J Neurosurg 95(2 Suppl):243–245
Brodsky AE, Khalil M, VanDeventer L (1986) Unicameral bone cyst of a lumbar vertebra. A case report. J Bone Jt Surg Am 68(8):1283–1285
Hazmy CH (2004) Unicameral bone cyst of the calcaneum. Med J Malaysia 59 Suppl F:63–64
Epstein J, Wertheimer SJ (1984) Unicameral bone cyst of the calcaneus. Literature review and case studies. J Am Podiatry Assoc 74(2):76–79
O’Laughlin SJ (2012) Unicameral bone cyst of the calcaneus. J Orthop Sports Phys Ther 42(1):43
Perlman MD, Maiocco JL, Rybczynski JM (1989) Unicameral bone cyst of the first metatarsal. J Foot Surg 28(1):38–41
Randelli P, Arrigoni P, Cabitza P, Denti M (2009) Unicameral bone cyst of the humeral head: arthroscopic curettage and bone grafting. Orthopedics 32(1):54
Wray CC (1986) Unicameral bone cyst of the ilium. J R Coll Surg Edinb 31(4):233–236
Wu KK (1990) Unicameral bone cyst of the medial malleolus of the ankle. J Foot Surg 29(2):183–187
Janjua KJ (1999) Unicameral bone cyst of the patella. Am J Knee Surg 12(2):111–113
Saglik Y, Ucar DH, Yildiz HY, Dogan M (1995) Unicameral bone cyst of the patella. A case report. Int Orthop 19(5):280–281
Wientroub S, Salama R, Baratz M, Papo I, Weissman SL (1979) Unicameral bone cyst of the patella. Clin Orthop Relat Res 140:159–161
Martin SJ, Schiller JE (1987) Unicameral bone cyst of the second metatarsal with pathologic fracture. J Am Podiatr Med Assoc 77(3):143–147
Chieppa WA, Shinder M (1989) Unicameral bone cyst of the talus. J Am Podiatr Med Assoc 79(9):441–446
Gordon SL, Denton JR, McCann PD, Parisien MV (1987) Unicameral bone cyst of the talus. Clin Orthop Relat Res 215:201–205
Nasca RJ (1988) Unicameral bone cyst of the tibia complicated by genu valgum. South Med J 81(10):1301–1304
Malawer MM, Markle B (1982) Unicameral bone cyst with epiphyseal involvement: clinicoanatomic analysis. J Pediatr Orthop 2(1):71–79
Deyoe L, Woodbury DF (1985) Unicameral bone cyst with fracture. Orthopedics 8(4):529–531
Singh S, Dhammi IK, Arora A, Kumar S (2003) Unusually large solitary unicameral bone cyst: case report. J Orthop Sci 8(4):599–601
Agerholm JC, Goodfellow JW (1965) Simple cysts of the humerus treated by radical excision. J Bone Jt Surg Br 47(4):714–717
MacKenzie DB (1980) Treatment of solitary bone cysts by diaphysectomy and bone grafting. S Afr Med J 58(4):154–158
Kleiger B (1969) Unicameral bone cyst, 15 year follow-up. Bull Hosp Jt Dis 30(1):53–58
Gundes H, Sahin M, Alici T (2010) Unicameral bone cyst of the lunate in an adult: case report. J Orthop Surg Res 5:79
Hutter CG (1950) Unicameral bone cyst; report of an unusual case. J Bone Jt Surg Am 32A(2):430–432
Dormans JP, Dormans NJ (2004) Use of percutaneous intramedullary decompression and medical-grade calcium sulfate pellets for treatment of unicameral bone cysts of the calcaneus in children. Orthopedics 27(1 Suppl):s137–s139
Siegel IM (1966) Brisement force with controlled collapse in treatment of solitary unicameral bone cyst. Arch Surg 92(1):109–114
Goel AR, Kriger J, Bronfman R, Lauf E (1994) Unicameral bone cysts: treatment with methylprednisone acetate injections. J Foot Ankle Surg 33(1):6–15
Cho HS, Seo SH, Park SH, Park JH, Shin DS, Park IH (2012) Minimal invasive surgery for unicameral bone cyst using demineralized bone matrix: a case series. BMC Musculoskelet Disord 13:134
Shibata K, Tsunooka H, Sasaki S, Oono N, Niwa A, Oowa T, Kamio Y, Saito Y, Sumita H, Naito A (1992) A case report of solitary bone cyst of rib detected from pathological fracture. Kyobu Geka 45(9):817–819
Zenmyo M, Komiya S, Hamada T, Inoue A (2000) A solitary bone cyst in the spinous process of the cervical spine: a case report. Spine (Phila Pa 1976) 25(5):641–642
Nystrom L, Raw R, Buckwalter J, Morcuende JA (2008) Acute intraoperative reactions during the injection of calcium sulfate bone cement for the treatment of unicameral bone cysts: a review of four cases. Iowa Orthop J 28:81–84
Asada Y, Suzuki I, Suzuki M, Fukushima M (1991) Atypical multiple benign osteoblastomas accompanied by simple bone cysts. A case report. J Craniomaxillofac Surg 19(4):166–171
Taneda H, Azuma H (1994) Avascular necrosis of the femoral epiphysis complicating a minimally displaced fracture of solitary bone cyst of the neck of the femur in a child. A case report. Clin Orthop Relat Res 304:172–175
Stelling CB, Martin W, Fechner RE, Alford BA, Strider DV (1981) Case report 150. Solitary bone cyst with cementum-like bone production. Skeletal Radiol 6(3):213–215
Hahn PF, Rosenthal DI, Ehrlich MG (1984) Case report 286: gas within a solitary bone cyst of the proximal end of the left humerus. Skeletal Radiol 12(3):214–217
Schultz E, Greenspan A (1986) Case report 378: simple bone cyst (traumatized). Skeletal Radiol 15(5):405–407
Wu KK, Guise ER (1981) Unicameral bone cyst of the spine. A case report. J Bone Jt Surg Am 63(2):324–326
Abdelwahab IF, Lewis MM, Klein MJ, Barbera C (1989) Case report 515: simple (solitary) bone cyst of the calcaneus. Skeletal Radiol 17(8):607–610
Abdelwahab IF, Hermann G, Lewis MM, Klein MJ (1989) Case report 534: simple bone cyst of the acetabulum and ischium. Skeletal Radiol 18(2):157–159
Gregory JM, Arkader A, Bokhari A, Dormans JP (2010) Case report: unicameral bone cysts in a young patient with acquired generalized lipodystrophy. Clin Orthop Relat Res 468(5):1440–1446
Grabias S, Mankin HJ (1974) Chondrosarcoma arising in histologically proved unicameral bone cyst. A case report. J Bone Jt Surg Am 56(7):1501–1509
Abril JC, Queiruga JA, Casas J, Albinana J (1999) Unusual finding after contrast injection of a solitary bone cyst. A case report. Acta Orthop Belg 65(2):235–238
Mason RJ, Friedman SJ, Frassica FJ (1994) Medial meniscal cyst of the knee simulating a solitary bone lesion. A case report and review of the literature. Clin Orthop Relat Res 304:190–194
Tamir E, Halperin N, Segal M, Robinson D (1998) Sclerotic hip medullary lesion evolving into a simple bone cyst–a case report. Acta Orthop Scand 69(6):647–648
Czitrom AA, Pritzker KP (1980) Simple bone cyst causing collapse of the articular surface of the femoral head and incongruity of the hip joint. A case report. J Bone Jt Surg Am 62(5):842–845
Smith SB, Shane HS (1994) Simple bone cyst of the calcaneus. A case report and literature review. J Am Podiatr Med Assoc 84(3):127–130
Ha KY, Kim YH (2003) Simple bone cyst with pathologic lumbar pedicle fracture: a case report. Spine (Phila Pa 1976) 28(7):E129–E131
Uygur F, Ulkur E, Pehlivan O, Celikoz B (2008) Soft tissue necrosis following using calcium phosphate cement in calcaneal bone cyst: case report. Arch Orthop Trauma Surg 128(12):1397–1401
Shen Q, Jia L, Li Y (1998) Solitary bone cyst in the odontoid process and body of the axis. A case report and review of literature. J Bone Jt Surg Br 80(1):30–32
Matsumoto K, Fujii S, Mochizuki T, Hukuda S (1990) Solitary bone cyst of a lumbar vertebra. A case report and review of literature. Spine (Phila Pa 1976) 15(6):605–607
Civello IM, Butti A (1978) Sutures of nonabsorbable material as the cause of disturbances in gastrectomized patients. Considerations on 19 personal cases. Chir Patol Sper 26(2):131–135
Sguazzini VC (1967) Solitary bone cyst of the clavicle (case report). Minerva Ortop 18(12):870–872
Goldsmith E (1966) Solitary bone cyst of the distal phalanx. A case report. J Am Podiatry Assoc 56(2):69–70
Gupta AK, Crawford AH (1996) Solitary bone cyst with epiphyseal involvement: confirmation with magnetic resonance imaging. A case report and review of the literature. J Bone Jt Surg Am 78(6):911–915
Rodolico R, Nicolato A, Scaglione P (1968) Solitary osseous cyst of the calcaneus. Case reports. Ann Radiol Diagn (Bologna) 41(3):183–191
Bosch B, Bialik G, Bialik V (2002) Spontaneous epiphyseal injury as a complication of a simple bone cyst of the femoral neck? Case report and review of the literature. Orthopade 31(9):930–933
Parker ME, Samsodien MG, Wood RE (1988) The untreated, shrinking simple bone cavity: case report. Ann Dent 47(2):43–45
Herring JA, Peterson HA (1987) Simple bone cyst with growth arrest. J Pediatr Orthop 7(2):231–235
Maney WA (1967) Kiel bone in the treatment of a simple bone cyst. Br J Clin Pract 21(10):519–520
Bourne MH, Beabout JW, Wold LE, Sim FH (1986) Simple bone cysts. Orthopedics 9(9):1285–1289
Catier P, Bracq H, Canciani JP, Allouis M, Babut JM (1981) The treatment of upper femoral unicameral bone cysts in children by Ender’s nailing technique. Rev Chir Orthop Reparatrice Appar Mot 67(2):147–149
Mainard D, Galois L (2006) Treatment of a solitary calcaneal cyst with endoscopic curettage and percutaneous injection of calcium phosphate cement. J Foot Ankle Surg 45(6):436–440
Nakagawa T, Kawano H, Kubota T (1994) Solitary bone cyst of the cervical spine–case report. Neurol Med Chir (Tokyo) 34(8):558–560
Vasilev V, Andreeff I, Sokolov T, Vidinov N (1987) Clinical-morphological and electron-microscopic studies of the growth plate in solitary bone cysts. Arch Orthop Trauma Surg 106(4):232–237
Sanerkin NG (1979) Old fibrin coagula and their ossification in simple bone cysts. J Bone Jt Surg Br 61-B(2):194–199
Komiya S, Tsuzuki K, Mangham DC, Sugiyama M, Inoue A (1994) Oxygen scavengers in simple bone cysts. Clin Orthop Relat Res 308:199–206
Yu J, Chang SS, Suratwala S, Chung WS, Abdelmessieh P, Lee HJ, Yang J, Lee FY (2005) Zoledronate induces apoptosis in cells from fibro-cellular membrane of unicameral bone cyst (UBC). J Orthop Res 23(5):1004–1012
Jager M, Jelinek EM, Wess KM, Scharfstadt A, Jacobson M, Kevy SV, Krauspe R (2009) Bone marrow concentrate: a novel strategy for bone defect treatment. Curr Stem Cell Res Ther 4(1):34–43
Yu CL, D’Astous J, Finnegan M (1991) Simple bone cysts. The effects of methylprednisolone on synovial cells in culture. Clin Orthop Relat Res 262:34–41
Gerasimov AM, Toporova SM, Furtseva LN, Berezhnoy AP, Vilensky EV, Alekseeva RI (1991) The role of lysosomes in the pathogenesis of unicameral bone cysts. Clin Orthop Relat Res 266:53–63
Vayego-Lourenco SA (2001) TP53 mutations in a recurrent unicameral bone cyst. Cancer Genet Cytogenet 124(2):175–176
Komiya S, Kawabata R, Zenmyo M, Hashimoto S, Inoue A (2000) Increased concentrations of nitrate and nitrite in the cyst fluid suggesting increased nitric oxide synthesis in solitary bone cysts. J Orthop Res 18(2):281–288
Zehetgruber H, Bittner B, Gruber D, Krepler P, Trieb K, Kotz R, Dominkus M (2005) Prevalence of aneurysmal and solitary bone cysts in young patients. Clin Orthop Relat Res 439:136–143
Becker WH (1952) Differential diagnosis of solitary bone cysts from giant cell tumors. Munch Med Wochenschr 94(36):1799–1804
Lee FY, Schoeb JS, Yu J, Christiansen BD, Dick HM (2005) Operative lengthening of the humerus: indications, benefits, and complications. J Pediatr Orthop 25(5):613–616
Sullivan RJ, Meyer JS, Dormans JP, Davidson RS (1999) Diagnosing aneurysmal and unicameral bone cysts with magnetic resonance imaging. Clin Orthop Relat Res 366:186–190
Levine E, Neff JR (1983) Dynamic computed tomography scanning of benign bone lesions: preliminary results. Skeletal Radiol 9(4):238–245
Pireau N, De GA, Mainard-Simard L, Lascombes P, Docquier PL (2011) Fracture risk in unicameral bone cyst. Is magnetic resonance imaging a better predictor than plain radiography? Acta Orthop Belg 77(2):230–238
Clayer M, Boatright C, Conrad E (1997) Growth disturbances associated with untreated benign bone cysts. Aust N Z J Surg 67(12):872–873
Lodwick GS (1958) Juvenile unicameral bone cyst; a roentgen reappraisal. Am J Roentgenol Radium Ther Nucl Med 80(3):495–504
Margau R, Babyn P, Cole W, Smith C, Lee F (2000) MR imaging of simple bone cysts in children: not so simple. Pediatr Radiol 30(8):551–557
Ahn JI, Park JS (1994) Pathological fractures secondary to unicameral bone cysts. Int Orthop 18(1):20–22
Caviglia H, Garrido CP, Palazzi FF, Meana NV (2005) Pediatric fractures of the humerus. Clin Orthop Relat Res 432:49–56
Lee JH, Reinus WR, Wilson AJ (1999) Quantitative analysis of the plain radiographic appearance of unicameral bone cysts. Invest Radiol 34(1):28–37
Struhl S, Edelson C, Pritzker H, Seimon LP, Dorfman HD (1989) Solitary (unicameral) bone cyst. The fallen fragment sign revisited. Skeletal Radiol 18(4):261–265
Morton KS (1964) The pathogenesis of unicameral bone cyst. Can J Surg 7:140–150
Kaelin AJ, MacEwen GD (1989) Unicameral bone cysts. Natural history and the risk of fracture. Int Orthop 13(4):275–282
Reinus WR, Wilson AJ (1995) Quantitative analysis of solitary lesions of bone. Invest Radiol 30(7):427–432
Yandow SM, Marley LD, Fillman RR, Galloway KS (2009) Precordial Doppler evaluation of simple bone cyst injection. J Pediatr Orthop 29(2):196–200
Norman A, Schiffman M (1977) Simple bone cysts: factors of age dependency. Radiology 124(3):779–782
Hammoud S, Weber K, McCarthy EF (2005) Unicameral bone cysts of the pelvis: a study of 16 cases. Iowa Orthop J 25:69–74
Brodetti A (1956) The weight bearing capacity of the femoral neck with solitary bone cyst. Acta Orthop Scand 26(2):81–98
Docquier PL, Paul L, Menten R, Cartiaux O, Francq B, Banse X (2009) Measurement of bone cyst fluid volume using k-means clustering. Magn Reson Imaging 27(10):1430–1439
Vasconcellos DA, Yandow SM, Grace AM, Moritz BM, Marley LD, Fillman RR (2007) Cyst index: a nonpredictor of simple bone cyst fracture. J Pediatr Orthop 27(3):307–310
Ortiz EJ, Isler MH, Navia JE, Canosa R (2005) Pathologic fractures in children. Clin Orthop Relat Res 432:116–126
Reynolds J (1969) The “fallen fragment sign” in the diagnosis of unicameral bone cysts. Radiology 92(5):949–953
Amling M, Werner M, Posl M, Maas R, Korn U, Delling G (1995) Calcifying solitary bone cyst: morphological aspects and differential diagnosis of sclerotic bone tumours. Virchows Arch 426(3):235–242
Yanagawa T, Watanabe H, Shinozaki T, Takagishi K (2009) Curettage of benign bone tumors without grafts gives sufficient bone strength. Acta Orthop 80(1):9–13
Shrader MW, Schwab JH, Shaughnessy WJ, Jacofsky DJ (2009) Pathologic femoral neck fractures in children. Am J Orthop (Belle Mead NJ) 38(2):83–86
Mnaymneh WA, Ghandur-Mnaymneh L, Chaglassian J (1973) Unicameral bone cyst. Appraisal of experience at the American University Hospital of Beirut. J Med Liban 26(4):459–470
Sakamoto A, Matsuda S, Yoshida T, Iwamoto Y (2010) Clinical outcome following surgical intervention for a solitary bone cyst: emphasis on treatment by curettage and steroid injection. J Orthop Sci 15(4):553–559
Haidar SG, Culliford DJ, Gent ED, Clarke NM (2011) Distance from the growth plate and its relation to the outcome of unicameral bone cyst treatment. J Child Orthop 5(2):151–156
Fillingham YA, Lenart BA, Gitelis S (2012) Function after injection of benign bone lesions with a bioceramic. Clin Orthop Relat Res 470(7):2014–2020
Glowacki M, Ignys-O’Byrne A, Ignys I, Wroblewska K (2011) Limb shortening in the course of solitary bone cyst treatment—a comparative study. Skeletal Radiol 40(2):173–179
Sturz H, Zenker H, Buckl H (1979) Total subperiosteal resection treatment of solitary bone cysts of the humerus. Arch Orthop Trauma Surg 93(3):231–239
Morton KS (1982) Unicameral bone cyst. Can J Surg 25(3):330–332
Tey IK, Mahadev A, Lim KB, Lee EH, Nathan SS (2009) Active unicameral bone cysts in the upper limb are at greater risk of fracture. J Orthop Surg (Hong Kong) 17(2):157–160
Stanton RP, Abdel-Mota’al MM (1998) Growth arrest resulting from unicameral bone cyst. J Pediatr Orthop 18(2):198–201
Garceau GJ, Gregory CF (1954) Solitary unicameral bone cyst. J Bone Joint Surg Am 36(A:2):267–280
Matthiass HH, Immenkamp M (1976) Surgical treatment of solitary bone cysts. Recent Results Cancer Res 54:231–238
Yajima H, Murata K, Kawamura K, Kawate K, Takakura Y (2008) Treatment of intraosseous ganglia and bone cysts of the carpal bones with injectable calcium phosphate bone cement. Hand Surg 13(3):167–173
Garcia Filho RJ, Dos Santos JB, Korukian M, Laredo FJ (1992) Conservative treatment of solitary bone cysts–a study of 55 patients. Rev Paul Med 110(3):131–137
Givon U, Sher-Lurie N, Schindler A, Ganel A (2004) Titanium elastic nail—a useful instrument for the treatment of simple bone cyst. J Pediatr Orthop 24(3):317–318
Chaves D (1980) Treatment of solitary cysts of the humerus. Treated by diaphyseal resection and bone grafting. Int Orthop 3(4):253–256
Biermann JS (2002) Common benign lesions of bone in children and adolescents. J Pediatr Orthop 22(2):268–273
Abdel-Wanis ME, Tsuchiya H (2002) Simple bone cyst is not a single entity: point of view based on a literature review. Med Hypotheses 58(1):87–91
Robins PR, Peterson HA (1972) Management of pathologic fractures through unicameral bone cysts. JAMA 222(1):80–81
Neer CS, Francis KC, Johnston AD, Kiernan HA Jr (1973) Current concepts on the treatment of solitary unicameral bone cyst. Clin Orthop Relat Res 97:40–51
Leclet H, Adamsbaum C (1998) Intraosseous cyst injection. Radiol Clin North Am 36(3):581–587
Wilkins RM (2000) Unicameral bone cysts. J Am Acad Orthop Surg 8(4):217–224
Capanna R, Campanacci DA, Manfrini M (1996) Unicameral and aneurysmal bone cysts. Orthop Clin North Am 27(3):605–614
Makley JT, Joyce MJ (1989) Unicameral bone cyst (simple bone cyst). Orthop Clin North Am 20(3):407–415
Kruls HJ (1979) Pathological fractures in children due to solitary bone cysts. Reconstr Surg Traumatol 17:113–118
Iorio R, Betz RR, Clancy MJ (1989) Treatment options in simple unicameral bone cysts. Orthopedics 12(6):877–878
Donaldson S, Chundamala J, Yandow S, Wright JG (2010) Treatment for unicameral bone cysts in long bones: an evidence based review. Orthop Rev (Pavia) 2(1):e13
Baig R, Eady JL (2006) Unicameral (simple) bone cysts. South Med J 99(9):966–976
Dormans JP, Pill SG (2002) Fractures through bone cysts: unicameral bone cysts, aneurysmal bone cysts, fibrous cortical defects, and nonossifying fibromas. Instr Course Lect 51:457–467
Lokiec F, Wientroub S (1998) Simple bone cyst: etiology, classification, pathology, and treatment modalities. J Pediatr Orthop B 7(4):262–273
Hecht AC, Gebhardt MC (1998) Diagnosis and treatment of unicameral and aneurysmal bone cysts in children. Curr Opin Pediatr 10(1):87–94
Chaney SL, Karp NE (1981) The use of freeze-dried bone allografts: a review of the literature with special emphasis on their use in treatment of solitary bone cysts. J Foot Surg 20(1):41–43
Cohen J (1977) Unicameral bone cysts. A current synthesis of reported cases. Orthop Clin North Am 8(4):715–736
Peltier LF, Jones RH (1978) Treatment of unicameral bone cysts by curettage and packing with plaster-of-Paris pellets. J Bone Jt Surg Am 60(6):820–822
Moore TM (1982) Orthopedics-important advances in clinical medicine: injection of steroid agents in solitary bone cysts. West J Med 137(5):408–409
Weinert CR (1989) Administering steroids in unicameral bone cysts. West J Med 150(6):684–685
Namazi H (2008) Practice pearl: a novel use of botulinum toxin for unicameral bone cyst ablation. Ann Surg Oncol 15(2):657–658
Savastano AA (1979) The treatment of bone cysts with intracyst injection of steroids. Injection of steroids will largely replace surgery in the treatment of benign bone cysts. R I Med J 62:93–95
Galasko CS (1974) Letter: the fate of simple bone cysts which fracture. Clin Orthop Relat Res (101):302–304
Matsumine A, Myoui A, Kusuzaki K, Araki N, Seto M, Yoshikawa H, Uchida A (2004) Calcium hydroxyapatite ceramic implants in bone tumour surgery. A long-term follow-up study. J Bone Jt Surg Br 86(5):719–725
Gebhart M, Blaimont P (1996) Contribution to the vascular origin of the unicameral bone cyst. Acta Orthop Belg 62(3):137–143
Innami K, Takao M, Miyamoto W, Abe S, Nishi H, Matsushita T (2011) Endoscopic surgery for young athletes with symptomatic unicameral bone cyst of the calcaneus. Am J Sports Med 39(3):575–581
Shindell R, Huurman WW, Lippiello L, Connolly JF (1989) Prostaglandin levels in unicameral bone cysts treated by intralesional steroid injection. J Pediatr Orthop 9(5):516–519
Fernbach SK, Blumenthal DH, Poznanski AK, Dias LS, Tachdjian MO (1981) Radiographic changes in unicameral bone cysts following direct injection of steroids: a report on 14 cases. Radiology 140(3):689–695
Lindell L (1963) Solitary unicameral bone cyst in childhood. Ann Chir Gynaecol Fenn 52:80–92
Glaser DL, Dormans JP, Stanton RP, Davidson RS (1999) Surgical management of calcaneal unicameral bone cysts. Clin Orthop Relat Res 360:231–237
Moreau G, Letts M (1994) Unicameral bone cyst of the calcaneus in children. J Pediatr Orthop 14(1):101–104
Kanellopoulos AD, Mavrogenis AF, Papagelopoulos PJ, Soucacos PN (2007) Elastic intramedullary nailing and DBM-bone marrow injection for the treatment of simple bone cysts. World J Surg Oncol 5:111
Abdel-Wanis ME, Tsuchiya H, Uehara K, Tomita K (2002) Minimal curettage, multiple drilling, and continuous decompression through a cannulated screw for treatment of calcaneal simple bone cysts in children. J Pediatr Orthop 22(4):540–543
Thawrani D, Thai CC, Welch RD, Copley L, Johnston CE (2009) Successful treatment of unicameral bone cyst by single percutaneous injection of alpha-BSM. J Pediatr Orthop 29(5):511–517
Saraph V, Zwick EB, Maizen C, Schneider F, Linhart WE (2004) Treatment of unicameral calcaneal bone cysts in children: review of literature and results using a cannulated screw for continuous decompression of the cyst. J Pediatr Orthop 24(5):568–573
Killian JT, Wilkinson L, White S, Brassard M (1998) Treatment of unicameral bone cyst with demineralized bone matrix. J Pediatr Orthop 18(5):621–624
Yandow SM, Lundeen GA, Scott SM, Coffin C (1998) Autogenic bone marrow injections as a treatment for simple bone cyst. J Pediatr Orthop 18(5):616–620
Lokiec F, Ezra E, Khermosh O, Wientroub S (1996) Simple bone cysts treated by percutaneous autologous marrow grafting. A preliminary report. J Bone Jt Surg Br 78(6):934–937
Delloye C, Docquier PL, Cornu O, Poilvache P, Peters M, Woitrin B, Rombouts JJ, De Nayer P (1998) Simple bone cysts treated with aspiration and a single bone marrow injection. A preliminary report. Int Orthop 22(2):134–138
Symeonides PP, Economou CJ, Papadimitriou J (1977) Solitary bone cyst of the calcaneus. Int Surg 62(1):24–26
Pedzisz P, Zgoda M, Kocon H, Benke G, Gorecki A (2010) Treatment of solitary bone cysts with allogenic bone graft and platelet-rich plasma. A preliminary report. Acta Orthop Belg 76(3):374–379
Rosenborg M, Karlsson A, Hirsch G, Mortensson W (1992) Contrast medium injected into juvenile bone cysts to analyze interior morphology and guide intracavity corticosteroid treatment. Acta Radiol 33(3):221–224
El-Adl G, Mostafa MF, Enan A, Ashraf M (2009) Biphasic ceramic bone substitute mixed with autogenous bone marrow in the treatment of cavitary benign bone lesions. Acta Orthop Belg 75(1):110–118
Rud B, Pedersen NW, Thomsen PB (1991) Simple bone cysts in children treated with methylprednisolone acetate. Orthopedics 14(2):185–187
Gartland JJ, Cole FL (1975) Modern concepts in the treatment of unicameral bone cysts of the proximmal humerus. Orthop Clin North Am 6(2):487–498
Robbins H (1982) The treatment of unicameral or solitary bone cysts by the injection of corticosteroids. Bull Hosp Jt Dis Orthop Inst 42(1):1–16
Komiya S, Minamitani K, Sasaguri Y, Hashimoto S, Morimatsu M, Inoue A (1993) Simple bone cyst. Treatment by trepanation and studies on bone resorptive factors in cyst fluid with a theory of its pathogenesis. Clin Orthop Relat Res 287:204–211
Santori F, Ghera S, Castelli V (1988) Treatment of solitary bone cysts with intramedullary nailing. Orthopedics 11(6):873–878
Kose N, Gokturk E, Turgut A, Gunal I, Seber S (1999) Percutaneous autologous bone marrow grafting for simple bone cysts. Bull Hosp Jt Dis 58(2):105–110
Arazi M, Senaran H, Memik R, Kapicioglu S (2005) Minimally invasive treatment of simple bone cysts with percutaneous autogenous bone marrow injection. Orthopedics 28(2):108–112
Sponer P, Urban K, Urbanova E, Karpas K, Mathew PG (2010) Behavior of bioactive glass-ceramic implanted into long bone defects: a scintigraphic study. J Pediatr Orthop B 19(1):102–107
Morii T, Mochizuki K, Satomi K (2009) Continuous decompression using a cannulated ceramic pin for simple bone cysts. J Orthop Surg (Hong Kong) 17(1):62–66
Chigira M, Maehara S, Arita S, Udagawa E (1983) The aetiology and treatment of simple bone cysts. J Bone Jt Surg Br 65(5):633–637
Vigler M, Weigl D, Schwarz M, Ben-Itzhak I, Salai M, Bar-On E (2006) Subtrochanteric femoral fractures due to simple bone cysts in children. J Pediatr Orthop B 15(6):439–442
Ovadia D, Ezra E, Segev E, Hayek S, Keret D, Wientroub S, Lokiec F (2003) Epiphyseal involvement of simple bone cysts. J Pediatr Orthop 23(2):222–229
Tang XY, Liu LJ, Peng MX, Xiang B (2006) Simple bone cysts in children treated with intracystic fibrin sealant injection. Chin Med J (Engl) 119(6):523–525
Scaglietti O, Marchetti PG, Bartolozzi P (1979) The effects of methylprednisolone acetate in the treatment of bone cysts. Results of three years follow-up. J Bone Jt Surg Br 61(2):200–204
Capanna R, Van HJ, Ruggieri P, Biagini R (1986) Epiphyseal involvement in unicameral bone cysts. Skeletal Radiol 15(6):428–432
Capanna R, Albisinni U, Caroli GC, Campanacci M (1984) Contrast examination as a prognostic factor in the treatment of solitary bone cyst by cortisone injection. Skeletal Radiol 12(2):97–102
Bensahel H, Jehanno P, Desgrippes Y, Pennecot GF (1998) Solitary bone cyst: controversies and treatment. J Pediatr Orthop B 7(4):257–261
Chigira M, Shimizu T, Arita S, Watanabe H, Heshiki A (1986) Radiological evidence of healing of a simple bone cyst after hole drilling. Arch Orthop Trauma Surg 105(3):150–153
Campanacci M, De SL, Trentani C (1977) Scaglietti’s method for conservative treatment of simple bone cysts with local injections of methylprednisolone acetate. Ital J Orthop Traumatol 3(1):27–36
Roposch A, Saraph V, Linhart WE (2004) Treatment of femoral neck and trochanteric simple bone cysts. Arch Orthop Trauma Surg 124(7):437–442
Spence KF, Sell KW, Brown RH (1969) Solitary bone cyst: treatment with freeze-dried cancellous bone allograft. A study of one hundred seventy-seven cases. J Bone Jt Surg Am 51(1):87–96
Docquier PL, Delloye C (2003) Treatment of simple bone cysts with aspiration and a single bone marrow injection. J Pediatr Orthop 23(6):766–773
Dormans JP, Sankar WN, Moroz L, Erol B (2005) Percutaneous intramedullary decompression, curettage, and grafting with medical-grade calcium sulfate pellets for unicameral bone cysts in children: a new minimally invasive technique. J Pediatr Orthop 25(6):804–811
Bensahel H (1976) Treatment of the solitary bone cyst in children. Nouv Presse Med 5(11):711–712
Salama R, Weissman SL (1978) The clinical use of combined xenografts of bone and autologous red marrow. A preliminary report. J Bone Jt Surg Br 60(1):111–115
Burwell RG (1964) Studies in the transplantation of bone. VII. The fresh composite homograft of cancellous bone, an analysis of factors leading to osteogenesis in marrow transplantations and in marrow-containing bone grafts. J Bone Jt Surg Br 46:110–140
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kadhim, M., Thacker, M., Kadhim, A. et al. Treatment of unicameral bone cyst: systematic review and meta analysis. J Child Orthop 8, 171–191 (2014). https://doi.org/10.1007/s11832-014-0566-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-014-0566-3