Abstract
Purpose
The purpose of this retrospective study was to evaluate the long-term outcome of different methods of treatment in slipped capital femoral epiphysis (SCFE), to find risk factors for poor outcome, and to assess whether prophylactic fixation is indicated.
Methods
Sixty-six patients (76 hips) treated for SCFE with a mean follow-up of 38 years (range 21–57 years) were evaluated. All except seven patients had chronic SCFE. Ten patients (15%) had bilateral affection. Three methods of treatment had been used: screw fixation (35 hips), bone-peg epiphysiodesis (30 hips), and bone-peg epiphysiodesis combined with corrective femoral osteotomy (11 hips). The long-term clinical outcome was classified as good when the patient had not undergone total hip replacement (THR), when the Harris hip score (HHS) was 85 points or above, or the patient had no pain. Good radiographic outcome was defined as no THR or osteoarthritis (OA).
Results
In 51 patients with chronic slip (mean slip angle 32°) treated with in situ fixation, the clinical outcome was good in 35 patients (69%) and there was no significant difference between screw fixation and bone-peg epiphysiodesis. Eight patients with large chronic slip (mean slip angle 53°) were treated with bone-peg epiphysiodesis and corrective femoral osteotomy, and the clinical outcome was poor in six patients. Seven patients with acute slip had larger mean slip angle (57°) and more complications than those with chronic slip, and the long-term outcome was poor in all. Two hips out of 42 (5%) had OA in the contralateral hip at follow-up.
Conclusion
In situ fixation of chronic SCFE gave satisfactory long-term outcome irrespective of the treatment method. Corrective femoral osteotomy did not improve the outcome in hips with large slip angles. Acute SCFE had poor outcome. Prophylactic fixation of the contralateral hip is barely necessary.
Similar content being viewed by others
Introduction
Slipped capital femoral epiphysis (SCFE) is the most frequent hip disorder among adolescents. There is a risk of developing osteoarthritis (OA) later in life, but symptomatic OA generally does not appear until the fourth or fifth decade of life [1–4]. Thus, long-term follow-up studies are necessary to predict outcome.
The aim of treatment in SCFE is to prevent further slip and avoid complications like chondrolysis and avascular necrosis. Percutaneous in situ fixation with a single cannulated screw has shown consistently good results [5–7] and is presently widely used. Before the era of screw and pin fixation, open bone-peg epiphysiodesis was used in Norway. In cases with more severe displacement, it was combined with corrective osteotomy of the proximal femur. Bone-peg epiphysiodesis was first described by Ferguson and Beckett Howorth in 1931 [8]. The purpose of this treatment is to achieve rapid closure of the physis and to avoid further slip. Compared with internal fixation, the advantages are the avoidance of hardware joint protrusion and no second operation for hardware removal. There is, however, a risk of further slip [9, 10]. To our knowledge, no long-term follow-up studies exist regarding this method.
The purposes of this study were to compare the long-term clinical and radiographic outcome in patients treated for SCFE by bone-peg epiphysiodesis and screw fixation, to evaluate whether femoral osteotomy in more pronounced slips improved the outcome, and to assess whether fixation of the contralateral hip is indicated.
Patients and methods
The study was approved by the Regional Ethical Committee and the Data Inspectorate. All patients gave their informed consent prior to their inclusion in the study. The patients were identified by searching through the radiographic archive in our hospital during the year 2006. We included the patients that were living in the ten counties in the South-East area of Norway with all original radiographs available and a minimum follow-up of 20 years. Seventy-nine patients met the inclusion criteria. However, 13 patients were not included because of the following reasons: seven patients had died during the follow-up time, five patients did not respond to the enquiry, and one patient did not want to participate in the study. Thus, 66 patients (76 hips) were included, representing a 92% follow-up. Twenty-four patients (36%) were female and 42 patients were male. They had been treated between 1953 and 1986. The mean age at primary surgery was 13.2 years, 12.5 years (range 10.7–14.5 years) among the female patients and 13.6 years (range 8.8–16.7 years) among the male patients.
The duration of symptoms until diagnosis was estimated from the medical records. The severity of the slip was measured on the original preoperative frog-leg radiograph and was classified according to the head-shaft angle as described by Southwick [11]. We did not subtract the head-shaft angle of the contralateral hip. If the head-shaft angle was 30° or below, the slip was classified as mild, whereas angles between 30° and 50° were termed moderate, and angles above 50° were classified as severe slips [1]. Clinically, the slip was classified as acute if the duration of symptoms was less than 3 weeks and chronic if the duration of symptoms was more than 3 weeks. If mild prodromal symptoms had been present for several months preceding an acute episode, the slip was classified as acute on chronic [12].
Three different types of treatment had been used: screw fixation (35 hips), bone-peg epiphysiodesis (30 hips), and bone-peg epiphysiodesis combined with corrective osteotomy of the proximal femur (11 hips). The choice of treatment method was mainly based on what was the routine at the time and the surgeon’s preferences. In the 1950s and 1960s, bone-peg epiphysiodesis was used, and in cases with more pronounced slip, it was combined with corrective femoral osteotomy. With time, screw fixation gradually replaced bone-peg epiphysiodesis. Before bone-peg epiphysiodesis, most patients were placed in traction for 1–3 weeks. An open approach was used, and two bone-pegs (allografts) were placed through the femoral neck, through the physis, and into the epiphysis. Routinely, the patients treated with bone-peg epiphysiodesis were treated with bedrest or traction for about 10 weeks postoperatively.
In four of the patients treated with osteotomy, the bone-peg epiphysiodesis and osteotomy were performed in the same operation. In three patients, the osteotomy was performed 1 month after the bone-peg epiphysiodesis, in two patients 4–6 months after, and in two patients 2 years after. Three osteotomies were located at the base of the femoral neck, and large metallic staples were used for fixation. The other eight osteotomies were intertrochanteric. Three of them were fixated with an angled plate, while fixation with a straight plate was used in the other five.
The treatment with screw fixation was performed with different kinds of threaded screws in 32 hips (25 spongiosa screws and seven fully threaded screws). Five hips were fixated with one single screw, 24 hips with two screws, and three hips with three screws. In three hips, a Smith–Peterson nail was used.
Chondrolysis was defined as a decrease, during the first postoperative year, in the width of the joint space greater than 50% compared with the contralateral hip, or if bilateral involvement, a joint space of less than 3 mm [13]. Avascular necrosis was considered when there was a collapse of the femoral head on the radiographs [14].
At follow-up, 50 patients (58 hips) were examined clinically and radiographically. We rated hip function with the Harris hip score (HHS) [15], which has a range from 0 points (maximum disability) to 100 points (no disability). In the present study, a HHS score of 85 points or above was classified as a good clinical result, while a score below 85 points was classified as a poor result. If patients had been operated with total hip replacement (THR), we classified the result as poor. In patients with bilateral affection, the clinical result was defined according to the hip with the worst outcome.
The 16 patients that did not appear for the follow-up examination were evaluated by telephone interview. In this group, information regarding whether the patient had been treated with THR or not was obtained, and they were asked if they had hip-related pain or discomfort, and if they had limping or were using crutches. In these patients, good clinical outcome was defined as no or negligible pain, good gait function without support, and no THR.
The patients’ weight and height were measured and the body mass index (BMI) calculated.
As a measure of health-related quality of life, we used the EQ-5D (EuroQol) [16, 17]. The EQ-5D index score is a standardized instrument for use as a measure of health outcome and has five dimensions (mobility, personal hygiene, usual activities, pain/discomfort, and anxiety/depression). The EQ-5D visual analog scale ranges from 0 (worst possible health) to 100 (best possible health).
With the patient supine, radiographs of the pelvis and both hips, including lateral view, were taken at the follow-up examination. The film-focus distance was 115 cm. Osteoarthritis was defined according to Jacobsen and Sonne-Holm [18], with a minimum joint space width of less than 2 mm in the upper weight-bearing part of the joint as the criterion for OA. The result was classified as good if there was no OA. If there was OA or the hip had been operated with THR, the result was poor.
Statistics
SPSS was used for the statistics analysis. Categorical data were analyzed with the Chi-square test. Continuous data were analyzed using the t-test. Differences were considered to be significant when the P-value was below 0.05.
Results
The mean time from primary surgery to the follow-up examination was 38 years (range 21–57 years). There were 56 patients with unilateral and ten patients (15%) with bilateral affection. Sixty-nine hips (91%) had a chronic slip, five hips had an acute on chronic slip, while two hips had an acute slip.
From the medical records, we were able to make an estimate of the duration of symptoms until diagnosis in 48 patients with chronic or acute on chronic slip. The mean duration was 5.1 months (range 1–12 months). In the group with a mild slip, it was 3.8 months (range 1–9 months), if there was a moderate slip, it was 5.2 months (range 2–12 months), while it was 6.3 months (range 2–12 months) in the group with severe slips. The mean slip angle was 36° (range 12–78°), 22° (range 12–30°) among the 37 hips with mild slip, 40° (range 32–50°) among the 23 hips with moderate slip, and 64° (range 54–78°) among the 16 hips with severe slip.
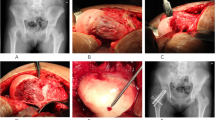
At follow-up, 14 patients (16 hips) had been treated with THR (Fig. 1) at a mean age of 48.1 years (range 41–66 years) and one patient with hip arthrodesis. Pronounced pain in addition to radiographic OA were the indications for THR. With THR or hip arthrodesis defined as failure, the cumulative survival rate according to Kaplan–Meyer survival analysis was 0.91 after 30 years, 0.77 after 40 years, and 0.55 after 50 years (Fig. 2). The hip arthrodesis was performed 1 year after the primary surgery. The time interval between primary surgery and THR was, on average, 36 years (range 23–51 years). Two of the THRs were revised 9 and 10 years after the primary replacement, respectively.
Radiographs of a male patient 12.7 years old at diagnosis treated for mild bilateral slipped capital femoral epiphysis (SCFE) of chronic type with bone-peg epiphysiodesis. a Preoperative radiograph (frog-leg view) of the right hip (slip angle 21°). b Preoperative radiograph (frog-leg view) of the left hip (slip angle 22°). c Postoperative radiograph of the pelvis. d Radiograph of the pelvis 6 years after primary treatment. e Radiograph of the pelvis at the last follow-up 48 years after primary treatment. The patient underwent total hip replacement (THR) in his left hip 10 months before the last follow-up. No osteoarthritis has occurred in his right hip
The mean HHS among the 39 patients not having THR or hip arthrodesis was 88 points (range 45–100 points). Of the 16 patients evaluated by telephone interview, four had undergone THR and one patient had severe discomfort from the hip (pain and stiffness) and was using two crutches; these were classified as having a poor clinical outcome. One patient reported occasionally slight discomfort after physical exercise and ten patients reported no discomfort at all, and these 11 patients were classified as having a good clinical outcome. Radiographs at follow-up were obtained in 39 patients (45 hips) with surviving hips (no THR or hip arthrodesis). Eight patients had developed OA and these patients had a mean HHS of 64 points (range 45–82 points).
The mean EQ-5D visual analog scale score at follow-up was 74 (range 30–100), and the mean EQ-5D index score was 0.84 (range 0.30–1.00).
At the time of follow-up, 59 patients (89%) were employed and seven had disability pension. The mean BMI was 30.0 kg/m2 (range 20.3–46.0 kg/m2), 29.5 kg/m2 among male and 30.5 kg/m2 among female patients. Nineteen patients (38%) had a BMI above 30 kg/m2 (overweight). There was a tendency to higher BMI (34.1 kg/m2) in patients with acute slips than in those with chronic slips (29.3 kg/m2; P = 0.07).
In situ fixation of chronic slips
Fifty-one patients (61 hips) with chronic SCFE were treated with in situ fixation, 28 patients (31 hips) with screw fixation and 23 patients (30 hips) with bone-peg epiphysiodesis. The mean slip angle was larger and the follow-up time shorter in patients treated with screw fixation (Table 1).
Evaluation at long-term follow-up showed no significant differences between screw fixation and bone-peg epiphysiodesis regarding clinical outcome, radiographic outcome, EQ-5D visual analog scale score and index score, and BMI (Table 1). The clinical outcome was good in 35 patients (69%) and poor in 16 patients. Of 50 hips with in situ fixation, 36 hips (72%) had a good radiographic outcome and 14 hips had poor outcome.
There were few serious complications among hips treated with in situ fixation. One hip with severe slip, treated with bone-peg epiphysiodesis, developed chondrolysis and the patient underwent THR at the age of 52 years. Separation of the physis after screw fixation occurred in one patient with severe slip, and reoperation with two nails was performed with subsequent avascular necrosis. The patient underwent THR at the age of 64 years. Complications in the screw fixation group included six hips with protrusion of a few millimeters of the screw beyond the bony outline of the femoral head. Three hips had had a mild slip and three hips a moderate slip. One of these patients (slip angle 48°) underwent THR at the age of 50 years. The others had a good clinical outcome.
Bone-peg epiphysiodesis with femoral osteotomy in chronic slips
Eight patients (eight hips) with chronic SCFE were treated with bone-peg epiphysiodesis combined with corrective femoral osteotomy. The mean slip angle (53°) was larger than in patients treated with in situ fixation (mean angle 32°). The long-term outcome was not satisfactory, since the clinical results were poor in six of eight patients and the radiographic results were poor in five of six patients (Table 2). There were serious complications in three hips. Avascular necrosis occurred in one hip with severe slip and the clinical outcome was poor because of severe pain and stiffness in the hip. Chondrolysis developed in two hips with moderate slip. One patient underwent hip arthrodesis 1 year after primary surgery and the other had poor outcome with OA and an HHS score of 82 points.
To assess whether or not hips with more marked slips benefited from corrective osteotomy, this group was compared with those hips with the same amount of chronic slipping but with in situ fixation only (Table 2). Apart from more males and older age at surgery in patients with osteotomy, no other significant differences between the groups occurred. However, there was a trend towards worse clinical and radiographic outcome in patients with osteotomy (Table 2).
Acute slips
The slip severity in the acute and acute on chronic slips was severe in five patients and moderate in two (mean slip angle 57°, range 40–70°). The mean age at surgery was 12.8 years (range 11.4–14.6 years). Four hips had been treated with screw fixation and three with bone-peg epiphysiodesis combined with corrective femoral osteotomy.
The long-term clinical outcome was poor in all seven patients and the radiographic results were poor in all except one. Three hips with screw fixation were complicated by avascular necrosis of the femoral head, leading to THR in two patients (aged 41 and 55 years, respectively) and OA with an HHS of 68 points in one. Of the other four patients, two had undergone THR (aged 37 and 48 years, respectively), one patient had OA with an HHS of 47 points, and one patient had a low HHS score (69 points) but no OA.
Bilateral slips
Ten patients (15%) had been treated for bilateral slip. The mean age at surgery of the index slip was 12.7 years in the bilateral cases and 13.3 years in the unilateral cases (P = 0.22). The initial slip in the bilateral cases was mild in eight hips, moderate in one hip, and severe in one hip. The subsequent contralateral slip was mild in nine hips and moderate in one. The mean slip angle (25°) in the bilateral cases was lower than in the unilateral cases (40°; P < 0.001). Five patients were operated on both sides within a few weeks, which was the routine at that time when there was bilateral affection at the time of diagnosis. In the remaining five patients, the subsequent contralateral slip was operated after 5, 6, 12, 13, and 21 months, respectively. No difference was found in the BMI between unilateral and bilateral SCFE (P = 0.76). The long-term results were satisfactory in both the initial and the subsequent slip, with good clinical outcome in 7 of 10 patients and good radiographic outcome results in 15 of 20 hips.
Forty-two patients with unilateral affection were examined radiographically at follow-up. When evaluating the contralateral hips, no patients underwent THR, but there were two hips (5%) with OA.
Discussion
The onset of symptoms in SCFE can be vague and subtle, and this could make the information about the onset of symptoms unreliable. The patients in our study were treated from 1953 to 1986, and the mean duration of symptoms was 5.1 months. This is in accordance with previous studies [19–21]. It seems that the delay in diagnosis has been relatively constant throughout the past decades, although Kocher et al. [22] had a shorter delay (2 months) during the period 1988–2002. As in previous studies [19–22], we found the duration of symptoms to be longer in moderate and severe slips, indicating that there is still a need to focus on reaching the diagnosis earlier to avoid an increase in slipping.
Slip severity was measured according to Southwick’s head-shaft angle [11], which is commonly used for the severity of SCFE. We did not subtract the head-shaft angle of the contralateral side, which, in unaffected hips, has been found to be 12° on average [23]. This probably means that we classified more moderate and severe slips than in studies where the head-shaft angle of the contralateral side has been subtracted. The mean slip angle in our study was 34° among chronic slips, which is in accordance with previous studies where the contralateral head-shaft angle was not subtracted, reporting mean slip angles of 29° [19] and 35° [7].
In general, the comparison of retrospective studies is difficult, because different classifications and definitions of outcome have been used. The HHS is a widely used functional score and has been validated for patients with osteoarthritis [24]. We found a clear association between HHS and long-term radiographic outcome, since none of the patients with an HHS above 82 points had developed OA. Sixteen patients did not appear for the follow-up examination and were evaluated by telephone interview. Four patients had been treated with THR and were classified as having a poor radiographic and clinical outcome. The remaining 12 patients were not omitted from the long-term clinical evaluation because they gave valuable information during telephone interview. One patient had severe pain and obviously had a poor clinical outcome. One patient had slight discomfort only after physical exercise and ten patients had no pain at all. These 11 patients were classified as having a good clinical outcome even if they were not assessed by physical examination. It is, however, indisputable that patients with no THR and no hip pain during long-term follow-up have a good clinical outcome. Including these patients gave a very satisfactory follow-up rate of 92%. This way of performing long-term studies will considerably contribute to a decrease in the number of patients “lost to follow-up”.
Regarding radiographic outcome, our definition of osteoarthritis as radiographic signs of a minimum joint space width less than 2 mm has been validated by Jacobsen and Sonne-Holm [18]. THR or hip arthrodesis is an objective end point in long-term studies. The age of the patients treated with THR (48 years) is distinctly lower than the average age of all patients receiving THR in Norway (69 years). Since none of the patients had had hip fracture or other hip disorders, it is highly probable that SCFE was the cause of OA.
In chronic slips, our results with 69% good clinical outcome and 28% OA after in situ fixation are in accordance with the few previous reports with longer than 20 years follow-up. With 41 years follow-up, Carney et al. [2] found that pinning gave better long-term outcome than other methods (symptomatic treatment, spica cast, and femoral osteotomy) with an Iowa hip rating of 90 points. Hägglund et al. [25] had a mean follow-up of 28 years and reported OA in 24% of the hips treated with pinning or nailing in situ. Hansson et al. [3] reviewed the radiographic results in chronic slips after nailing in situ, and 31% of the hips had OA at a mean follow-up of 31 years.
In the present study, screw fixation was compared with bone-peg epiphysiodesis in chronic slips. The slip angle was larger in the screw fixation group because bone-peg epiphysiodesis was combined with femoral osteotomy in more severe slips. Interestingly, the outcome after bone-peg epiphysiodesis was similar to that after screw fixation, even though the mean time of follow-up was 10 years longer in the bone-peg group. To our knowledge, no previous long-term follow-up studies exist regarding bone-peg epiphysiodesis. Adamczyk et al. [9] reported all cases of SCFE in a single institution treated by bone graft epiphysiodesis between 1950 and 2000. All patients were followed for at last 1 year, and both acute (n = 45) and chronic slips (n = 273) were included. Avascular necrosis occurred in 2% of the hips, chondrolysis in one hip, and reslippage in 7%. The authors suggested that this method is a reasonable treatment alternative. Zahrawi et al. [26] compared 28 hips treated with bone-peg epiphysiodesis and 60 hips with pinning in situ after an average follow-up of 7 years. The rate of failures and complications were higher in hips treated with bone-peg, and the authors found pinning in situ more predictable with less complications and better results. In our hospital, bone-peg epiphysiodesis was, from the late 1960s, replaced by screw fixation, because this method is technically less complicated and the patients do not need traction or bed rest postoperatively.
Will realignment procedures in more marked slips lead to better outcome? Our results were disappointing in this respect. In the few patients with femoral osteotomy in chronic slips, the results were unsatisfactory with poor clinical outcome in six of eight patients. This is in accordance with previous studies. Hägglund et al. [27] reported a high rate of OA (64%) after femoral neck osteotomy at 28 years follow-up. Jerre et al. [28] evaluated the outcome of 36 patients with moderate and severe slips treated with realignment procedures at an average follow-up of 34 years. Very poor results were found, as 22 hips (59%) had been treated with THR, hip arthrodesis, or had severe osteoarthritis. Newer osteotomy techniques [29] will probably give better results in hips with more marked slips, but no long-term studies exist to prove this.
In the only study we have found on long-term outcome in patients with acute SCFE, Carney et al. [2] reported no significant differences in the mean Iowa hip rate or radiographic grade of OA between hips with chronic slips and hips with acute slips after a mean follow-up of 41 years. This experience is in contrast to our results where the clinical and radiographic long-term outcome in acute slips were considerably worse than those in chronic slips. One reason for the worse outcome was probably the greater degree of slipping in the acute cases.
The management of the contralateral hip in unilateral SCFE is controversial. Some authors have recommended prophylactic fixation [30], whereas others have not [31]. In this study 15% of the patients were treated for bilateral slip, which is a lower rate of bilaterality compared to other studies, where the rate varied from 18 to 25% during adolescence [21, 31, 32]. In the unilateral cases with available radiographs at long-term follow-up, we found only two hips with OA in the contralateral hip, which supports our opinion that prophylactic fixation of the contralateral side is barely necessary. Jerre et al. [31] reviewed 61 patients primarily treated for unilateral SCFE with 32 years follow-up. Of the 52 contralateral hips not treated, 23% had loss of joint space, which is considerably higher than the 5% in our patients. However, they recorded pathological narrowing of the hip joint when the superior joint space was <3 mm, in contrast to 2 mm in the present study.
SCFE is known to be associated with obesity [19, 33, 34]. Manoff et al. [33] found that 81% of patients with SCFE had a BMI at diagnosis above the 95% percentile compared to 41% in the control group. Poussa et al. [34] compared annual height and weight from birth to onset of slippage in patients with SCFE and the normal population in Finland. Patients with SCFE had significantly higher BMI during growth. To our knowledge, no previous studies have estimated the BMI in patients with SCFE in long-term follow-up. Reas et al. [35] reported a mean BMI among Norwegian women of 24.6 kg/m2 and in men of 26.3 kg/m2. Compared with these results, the mean BMI in our study population (30.0 kg/m2) was higher (P < 0.005). One explanation could be that the level of physical activity is lower in this group because of poorer hip function, but it seems more likely that the higher BMI is constitutional to this condition also later in life.
To our knowledge, the EQ-5D has previously not been used in relation to SCFE. The mean EQ-5D index score among Danish individuals aged 50–59 years was 0.86 among women and 0.89 among men [36]. The mean score (0.84) was not poorer in the present study population. Eighty-nine percent of the patients in our study were employed at follow-up, which we consider to be satisfactory.
In conclusion, bone-peg epiphysiodesis gave similar good long-term outcome as screw fixation in chronic slips. Corrective femoral osteotomy did not improve the results in chronic slips with large slip angles. The outcome in acute slips was very poor. Because of the good clinical outcome and low rate of OA in the contralateral hip, we think that prophylactic fixation of this hip is barely indicated.
References
Boyer DW, Mickelson MR, Ponseti IV (1981) Slipped capital femoral epiphysis. Long-term follow-up study of one hundred and twenty-one patients. J Bone Joint Surg Am 63:85–95
Carney BT, Weinstein SL, Noble J (1991) Long-term follow-up of slipped capital femoral epiphysis. J Bone Joint Surg Am 73:667–674
Hansson G, Billing l, Högstedt B, Jerre R, Wallin J (1998) Long-term results after nailing in situ of slipped upper femoral epiphysis. A 30-year follow-up of 59 hips. J Bone Joint Surg Br 80:70–77
Murray RO (1965) The aetiology of primary osteoarthritis of the hip. Br J Radiol 38:810–824
Aronson DD, Carlson WE (1992) Slipped capital femoral epiphysis. A prospective study of fixation with a single screw. J Bone Joint Surg Am 74:810–819
Goodman WW, Johnson JT, Robertson WW Jr (1996) Single screw fixation for acute and acute-on-chronic slipped capital femoral epiphysis. Clin Orthop Relat Res 322:86–90
Ward WT, Stefko J, Wood KB, Stanitski CL (1992) Fixation with a single screw for slipped capital femoral epiphysis. J Bone Joint Surg Am 74:799–809
Ferguson AB, Beckett Howorth M (1931) Slipping of the upper femoral epiphysis. A study of seventy cases. J Am Med Assn 97:1867–1872
Adamczyk MJ, Weiner DS, Hawk D (2003) A 50-year experience with bone graft epiphysiodesis in the treatment of slipped capital femoral epiphysis. J Pediatr Orthop 23:578–583
Ward WT, Wood K (1990) Open bone graft epiphyseodesis for slipped capital femoral epiphysis. J Pediatr Orthop 10:14–20
Southwick WO (1967) Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am 49:807–835
Fahey JJ, O’Brien ET (1965) Acute slipped capital femoral epiphysis: review of the literature and report of ten cases. J Bone Joint Surg Am 47:1105–1127
Waldenstrøm H (1930) On necrosis of the joint cartilage by epiphyseolysis capitis femoris. Acta Chir Scand 67:936–946
Ficat RP (1985) Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br 67:3–9
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
EuroQol Group (1990) EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Brooks R (1996) EuroQol: the current state of play. Health Policy 37:53–72
Jacobsen S, Sonne-Holm S (2005) Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology 44:211–218
Loder RT, Starnes T, Dikos G, Aronsson DD (2006) Demographic predictors of severity of stable slipped capital femoral epiphyses. J Bone Joint Surg Am 88:97–105
Green DW, Reynolds RAK, Khan SN, Tolo V (2005) The delay in diagnosis of slipped capital femoral epiphysis: a review of 102 patients. HSS J 1:103–106
Wilson PD, Jacobs B, Schecter L (1965) Slipped capital femoral epiphysis: an end-result study. J Bone Joint Surg Am 47:1128–1145
Kocher MS, Bishop JA, Weed B, Hresko MT, Millis MB, Kim YJ, Kasser JR (2004) Delay in diagnosis of slipped capital femoral epiphysis. Pediatrics 113:e322–e325
Aronson DD, Loder RT (1992) Slipped capital femoral epiphysis in black children. J Pediatr Orthop 12:74–79
Hoeksma HL, Van den Ende CH, Ronday HK, Heering A, Breedveld FC, Dekker J (2003) Comparison of the responsiveness of the Harris Hip Score with generic measures for hip function in osteoarthritis of the hip. Ann Rheum Dis 62:935–938
Hägglund G, Hansson LI, Sandström S (1987) Slipped capital femoral epiphysis in southern Sweden. Long-term results after nailing/pinning. Clin Orthop Relat Res 217:190–200
Zahrawi FB, Stephens TL, Spencer GE (1983) Comparative study of pinning in situ and open epiphysiodesis in 105 patients with slipped capital femoral epiphyses. Clin Orthop Relat Res 177:160–168
Hägglund G, Hansson LI, Ordeberg G, Sandström S (1986) Slipped capital femoral epiphysis in southern Sweden. Long-term results after femoral neck osteotomy. Clin Orthop Relat Res 210:152–159
Jerre R, Hansson G, Wallin J, Karlsson J (1996) Long-term results after realignment operations for slipped upper femoral epiphysis. J Bone Joint Surg Br 78:745–750
Ziebarth K, Zilkens C, Spencer S, Leunig M, Ganz R, Kim Y-J (2009) Capital realignment for moderate and severe SCFE using a modified Dunn procedure. Clin Orthop Relat Res 467:704–716
Hägglund G (1996) The contralateral hip in slipped capital femoral epiphysis. J Pediatr Orthop B 5:158–161
Jerre R, Billing L, Hansson G, Wallin J (1994) The contralateral hip in patients primarily treated for unilateral slipped femoral epiphysis. Long-term follow-up of 61 hips. J Bone Joint Surg Br 76:563–567
Hägglund G, Hansson LI, Ordeberg G, Sandström S (1988) Bilaterality in slipped capital femoral epiphysis. J Bone Joint Surg Br 70:179–181
Manoff EM, Banffy MB, Winell JJ (2005) Relationship between body mass index and slipped capital femoral epiphysis. J Pediatr Orthop 25:744–746
Poussa M, Schlenzka D, Yrjönen T (2003) Body mass index and slipped capital femoral epiphysis. J Pediatr Orthop B 12:369–371
Reas DL, Nygård JF, Svensson E, Sørensen T, Sandanger I (2007) Changes in body mass index by age, gender, and socio-economic status among a cohort of Norwegian men and women (1990–2001). BMC Public Health 7:269
Sørensen J, Davidsen M, Gudex C, Møller Pedersen K, Brønnum-Hansen H (2009) Danish EQ-5D population norms. Scand J Public Health 37:467–474
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wensaas, A., Svenningsen, S. & Terjesen, T. Long-term outcome of slipped capital femoral epiphysis: a 38-year follow-up of 66 patients. J Child Orthop 5, 75–82 (2011). https://doi.org/10.1007/s11832-010-0308-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-010-0308-0