Abstract
Purpose
Little research has been done to identify possible cancer-related fatigue (CRF) subtypes and to classify cancer survivors accordingly. We aimed to identify CRF subtypes in a large population-based sample of (long term) stage I–III colorectal cancer survivors. We also identified factors associated with the CRF subtypes.
Methods
Respondents completed the Multidimensional Fatigue Inventory and other validated questionnaires on anxiety and reduced positive affect (anhedonia), sleep quality, and lifestyle factors (body mass index and physical activity). Latent class analysis was used to derive the CRF subtypes. Factors associated with the derived CRF subtypes were determined with multinomial logistic regression.
Results
Three CRF classes were identified: class 1 (no fatigue and distress, n = 644, 56%), class 2 (low fatigue, moderate distress, n = 256, 22%), and class 3 (high fatigue, moderate distress, n = 256, 22%). Multinomial logistic regression results show that survivors in class 3 were more likely to be female, were treated with radiotherapy, have comorbid diabetes mellitus, and be overweight/obese than survivors in class 1 (reference). Survivors in classes 2 and 3 were also more likely to have comorbid heart condition, report poorer sleep quality, experience anhedonia, and report more anxiety symptoms when compared with survivors in class 1.
Conclusions
Three distinct classes of CRF were identified which could be differentiated with sleep quality, anxiety, anhedonia, and lifestyle factors.
Implications for cancer survivors
The identification of CRF subtypes with distinct characteristics suggests that interventions should be targeted to the CRF subtype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer survivors commonly experience fatigue. The prevalence of cancer-related fatigue (CRF) varies widely from 15–99%, depending on the domains of fatigue assessed, time of assessment, and the questionnaire used [1]. However, for approximately 30% of survivors, CRF persists long after treatment completion [2]. CRF is defined as a subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to exertion effort and interferes with usual functioning [3].
Cancer survivors consider feeling fatigued as being more of a burden and having a greater negative impact on daily activities and health-related quality of life (HRQL) than other distressing symptoms like pain and depression [4, 5]. Despite its high prevalence and negative impact, CRF is still not well-understood. The etiology of CRF is equivocal [6], although it has been associated with cancer and its treatment [7]. CRF can be hard to treat. Current CRF treatments such as pharmacological treatments [8], exercise [9], or psychosocial [10] interventions yield small to moderate effect sizes in meta-analyses. A possible explanation for this limited treatment effect could be that the concept of CRF is not optimally delineated, and treatments are not targeted to patients’ specific fatigue experiences.
CRF has been conceptualized as a multidimensional concept, although there is discussion whether the dimensions of fatigue are expressions of one symptom (multidimensional concept) or expressions of separate symptoms such as physical or mental fatigue, collectively called fatigue (multiple symptom concept) [11]. In qualitative studies, survivors describe their CRF as physical, cognitive, or emotional sensations of tiredness [12]. According to the multiple symptom concept of fatigue, it is postulated that the dimensions of fatigue will behave differently among cancer survivors. A review found mixed results on the behaviors of physical and mental fatigue among cancer survivors and healthy controls [13]. Nevertheless, that review concluded there could be support for multiple symptom concept of fatigue as physical and mental fatigue generally had different correlates, based on the reviewed studies. A study that explored the fatigue experiences of cancer survivors and patients with advanced cancer found a weak correlation between physical and mental fatigue among cancer survivors but no correlation between these two dimensions of fatigue among patients with advanced cancer, suggesting that these fatigue dimensions could be separate phenomena among patients with advanced cancer [14]. Within the cancer survivor group, there was more heterogeneity in the relationship between physical and mental fatigue, suggestive of different patterns of fatigue within this group. However, little research has been done to classify cancer survivors according to CRF subtypes and to identify factors associated with the subtypes. In a study that focused only on physical CRF, distinct predictors and trajectories of morning and evening physical CRF were identified in on-treatment patients [15, 16]. It is intuitive that better classification of CRF can have implications for prognosis and response to treatment. For example, it is possible that a survivor with complaints of high physical and low mental CRF will benefit more from an exercise intervention. On the other hand, a survivor with more complaints of mental CRF could improve with psychosocial interventions.
In this exploratory analysis, our main study objective was to identify possible CRF subtypes in a large population-based sample of (long term) stage I–III colorectal cancer (CRC) survivors. We will also identify factors associated with the derived CRF subtypes and explore the association between the CRF subtypes and HRQL.
Methods
Setting and participants
This study is part of a longitudinal, population-based survey of all individuals living in the southern part of the Netherlands who were diagnosed with CRC between 2000 and 2009, as registered in the Netherlands Cancer Registry (NCR). The NCR compiles data of all individuals newly diagnosed with cancer in the Netherlands. The southern area covers 10 hospitals serving 2.4 million inhabitants [17]. We excluded individuals with cognitive impairment as indicated by the treating medical specialist, had died prior to start of study (according to the Central Bureau for Genealogy that collects information on all deceased Dutch citizens via the civil municipal registries and hospital records), or had unverifiable addresses. A complete overview of the sample selection can be found on our website under “data and documentation”, http://www.profilesregistry.nl/dataarchive/study_units/view/22.
Ethical approval for the study was obtained from a local certified Medical Ethics Committee of the Maxima Medical Centre Veldhoven.
Data collection
The study was started in December 2010, with yearly follow-ups. In 2013, the Multidimensional Fatigue Inventory (MFI-20) [18] was added to the standard questionnaire protocol. The analyses presented in this paper used the MFI data collected at this first assessment. Data were collected via PROFILES (Patient Reported Outcomes Following Initial treatment and Long term Evaluation of Survivorship). Details of the PROFILES data collection method have been described [19]. Briefly, eligible survivors received an invitation letter with a link to a secure website, a login name, and a password to provide informed consent and to complete questionnaires online. Individuals without internet access, or who preferred written rather than digital communication, could return a prepaid postcard requesting a pencil-and-paper version of the informed consent and questionnaire. Non-respondents were sent a reminder and questionnaire within 2 months.
Data from PROFILES studies are available for non-commercial scientific research, subject to study question, privacy and confidentiality restrictions, and registration (www.profilesregistry.nl) [19].
Study measures
MFI-20
The MFI-20 consists of five scales assessing: general fatigue (GF), physical fatigue (PF), reduced activity (RA), reduced motivation (RM), and mental fatigue (MF) [18]. It comprises 20 items and responses are ranged on a 5-point scale. Higher scores indicate more fatigue. The internal consistency of the subscales was satisfactory, with Cronbach’s alpha coefficients ranging from 0.79 to 0.93 [20].
Anxiety and depression (anhedonia)
The Hospital Anxiety and Depression Scale (HADS) comprises 14 items, 7 each assessing anxiety and depression [21]. Items were scored on a 4-point scale, ranging from 0 to 3. For the anxiety subscale, total score was 21 and a cut-off score ≥ 8 indicated clinical level of anxiety [21, 22]. To reduce possible overlap of physical symptoms of depression with fatigue, we limited items to those assessing lack of positive affect (i.e., anhedonia) [23]. This subscale consists of 4 items: I look forward with enjoyment to things, I feel cheerful, I can laugh and see the funny side of things, and I still enjoy the things I used to enjoy (range 0–12, mean + SD 2.2 ± 2.3). We defined anhedonia using a cut-off score of ≥ 6 (i.e., one SD above the mean) from the total score of the 4 items [24].
Sleep quality
Sleep quality was assessed with the Pittsburgh Sleep Quality Index (PSQI) [25]. The PSQI consists of 19 items from which 7 component scores are derived: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Although a total score of ≥ 5 indicates poor sleep [25], studies suggest that a cut-off of 8 is more appropriate for cancer survivors [26].
Functioning and HRQL
We used the 5 functioning (physical, role, emotional, cognitive, social) and the health status/overall quality of life scales of the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire version 3.0 (QLQ-C30) [27]. Items were scored on a scale from 1 (not at all) to 4 (very much) which were linearly transformed to a 1–100 scale following recommended guidelines [28]. Higher scores indicate better functioning and HRQL.
Demographics, lifestyle, and clinical data
Self-reported demographic data included marital status, weight, and height. BMI was calculated with self-reported height and weight. On the validated European Prospective Investigation into Cancer (EPIC) Physical Activity Questionnaire [29], patients reported the average time spent, during winter and summer, on walking, cycling, gardening, household activities, and sports. Hours per week spent on moderate-to-vigorous physical activity (MVPA) were derived from estimated metabolic equivalent intensity values assigned to each activity based on previously described classifications [30, 31].
Self-reported comorbid status at the time of survey was categorized according to the adapted Self-administered Comorbidity Questionnaire (SCQ) [32].
Demographic and clinical information including date of birth, date of diagnosis, cancer stage according to the tumor-node-metastasis clinical classification [33], and treatment were extracted from the NCR.
Statistical analyses
Differences in baseline characteristics of respondents, non-respondents, and survivors with non-verifiable addresses were determined using parametric tests (e.g., ANOVA) or non-parametric equivalents (e.g., chi-square). As there were no published cut-off scores of the MFI for cancer patients and to facilitate interpretation of results in daily clinical practice, we dichotomized the MFI scale scores using the 75th percentile as cut-off (Table 1) to identify the survivors who were fatigued. The cut-offs used in this study were comparable to the mean MFI scores of cancer patients (including CRC) undergoing chemotherapy [34]. We conducted latent class analysis using Latent GOLD 5.0 [35] to identify groups of survivors with similar CRF profiles. Latent class analysis is a data-driven approach that aims to obtain the smallest number of groups with similar profiles based on a categorical latent variable [36]. Using the 5 dichotomized MFI scores, we fitted models with 1 to 8 classes. The optimal number of latent classes was based on the model with the lowest Bayesian information criterion (BIC) value, indicating the best fit. Respondents were assigned to the class for which the posterior probability was highest. The factors that discriminated the identified classes were determined using multinomial logistic regression on IBM SPSS (Statistical Package for Social Sciences, Chicago, IL, USA) version 22 for Windows. Differences in the mean HRQL scores between identified CRF classes were determined with ANCOVA, correcting for sex and age at survey. Post hoc analyses were conducted using Bonferroni correction for multiple testing. All tests were two-sided and significant if p < 0.05.
Results
Participant characteristics
Of the 1465 stage I–III survivors eligible, 1183 (81%) returned a questionnaire. There were no significant differences in demographic and clinical characteristic differences between respondents and non-respondents (Table 2).
Characteristics of identified CRF classes
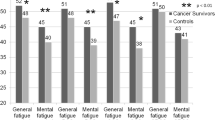
Based on the lowest BIC (Table 3), a 3-class solution was selected. Among the respondents, 27 (2%) were not classified and were excluded from subsequent multinomial logistic regression analyses. Of the 3-class model, class 1 (no fatigue and distress, n = 644, 56%) was characterized by very low scores on all MFI dimensions (Fig. 1). Class 2 (low fatigue, moderate distress, n = 256, 22%) was characterized by low scores on the three fatigue dimensions (GF, PF, MF) and moderate reduction in activities and motivation (RA, RM) dimensions. The third class (high fatigue, moderate distress, n = 256, 22%) was characterized by high general and physical fatigue, and moderate reduction in activities and motivation but low mental fatigue.
Factors associated with identified CRF classes
For the multinomial logistic regression models, class 1 (no fatigue and distress) was the reference group (Table 4). In comparison with class 1, factors associated with class 3 (high fatigue, moderate distress) were more likely to be female sex, treatment with radiotherapy, comorbid diabetes mellitus, and being overweight/obese. Survivors allocated to classes 2 (low fatigue, moderate distress) and 3 were also more likely to have comorbid heart condition, report poorer sleep quality, experience anhedonia, and report more anxiety symptoms when compared with those in class 1. When comparing factors that differentiated between classes 2 and 3, being female and reporting anhedonia symptoms were associated with significantly lower chances of being in class 3.
Differences in functioning and HRQL between the identified CRF classes
The EORTC-QLQ-C30 functioning and HRQL scores were all significantly different between the three fatigue classes. Survivors in class 1 (no fatigue and distress) scored the highest on all functioning and HRQL subscales and class 3 (high fatigue, moderate distress), the lowest (Fig. 2). Post hoc Bonferroni tests between each of the three classes were all significant at p < 0.0001 for all functioning and HRQL subscales.
EORTC functioning and HRQL subscale scores according to cancer-related fatigue latent classes. All EORTC functioning and HRQL subscales were significantly different between the 3 classes (p < 0.0001), corrected for sex and age at survey. Post-hoc Bonferroni tests between each of the 3 classes were all significant at p < 0.0001 for all functioning and HRQL subscales
Discussion
This study, using a large population-based sample of stage I-III (long term) CRC survivors, identified three classes of CRF. More than half of the survivors were classified as having no problems with fatigue or reduction in activities/motivation. For the other two fatigued classes, differences were found on severity of physical fatigue, and reduction in activity and motivation levels rather than mental fatigue. Our findings support previous research that proposed that cancer survivors could have different patterns of fatigue [14].
We found distinct characteristics in the identified CRF classes. Both classes 2 (low fatigue, moderate distress) and 3 (high fatigue, moderate distress) have poorer quality of sleep, heart problems, and anhedonia and anxiety symptoms in comparison with class 1 (no fatigue and distress). Although classes 2 and 3 are characterized by anhedonia and anxiety symptoms, the lower levels of fatigue of survivors in class 2 suggest this group is more likely to be depressed rather than fatigued. A study that investigated the diagnostic reliability of a semi-structured clinical interview for assessing fatigue in women with chronic illnesses including cancer, found that fatigue items were non-discriminatory between diagnostic groups while symptoms such as anhedonia and loss of motivation differentiated women with depression [37]. We cannot compare our results with previous research as we were not able to find published studies identifying CRF subtypes and their associated variables.
Symptoms such as poorer quality of sleep, anxiety, and depression commonly co-occur in cancer survivors [4], suggesting a common biological mechanism underlying these symptoms [38]. Increased levels of inflammation have been shown to be associated with fatigue, insomnia, and depression in breast cancer survivors [39], and fatigue and disturbed sleep among metastatic CRC patients [40]. Genetic associations between the IL-6 gene with fatigue and sleep disturbance were found among breast cancer patients [41].
Being overweight/obese was associated with higher odds of being classified in class 3 (high fatigue, moderate distress). This is in line with previous research [42, 43], highlighting the need for interventions to improve survivors’ self-management strategies for a healthier survivorship.
Using the MFI, we found distinct CRF classes among long-term CRC survivors. Future research using different questionnaires or samples (e.g., incident cancer patients) should be conducted to replicate our findings. Longitudinal studies could also investigate whether identified CRF subtypes remain stable or change during follow-up as this could have implications when developing interventions. We do not have biological data to explore the possibility of inflammation underlying the association between fatigue and other symptoms such as poor sleep, depression, and anxiety. In our new prospective study on incident CRC patients, we are including the collection of biological data.
We identified three distinct latent classes of CRF. Sleep quality, anxiety, anhedonia, and lifestyle factors significantly differentiated the identified CRF subtypes. Survivors with the highest levels of fatigue and reduced activity and motivation had the lowest HRQL scores. The identification of CRF subtypes with distinct characteristics suggests that interventions should be specific for the CRF subtype. A recent meta-analysis reported that cognitive behavioral therapy or exercise intervention was superior to pharmaceutical treatments in reducing fatigue among cancer survivors [44]. For example, survivors characterized by high levels of distress or sleep problems could benefit more from cognitive behavioral therapy [45, 46] or mindfulness-based therapy [47]. Survivors with a low activity pattern could profit more from exercise interventions [9, 48].
Several limitations of this study have to be considered. We report results from a cross-sectional study as we only have MFI data from one data point. As such, the results of this exploratory study should be cautiously interpreted. Although the MFI purports to assess five dimensions of fatigue, these dimensions have not been wholly replicated [49]. Nevertheless, in this exploratory study, we identified three classes of CRF that had different associations with sleep quality, anxiety, anhedonia, and lifestyle factors. Dichotomizing the MFI scale scores could reduce the information available [50]. Potential loss of power from dichotomizing could be mitigated by our large sample size. We used the 75th IQR range as a cut-off for the MFI as there was no published cut-offs for cancer patients. Published cut-off scores were available only on the general fatigue and reduced activity dimensions in a study of individuals with chronic fatigue syndrome [51]. The cut-offs we used were comparable to those used in that study and to the mean fatigue scores of cancer patients (including CRC) undergoing chemotherapy [34]. Furthermore, our sample included long-term survivors which could introduce survivorship bias, i.e., causes of fatigue might not be necessarily cancer-related but could be due to aging and other comorbid conditions. However, time since diagnosis was not associated with the latent classes of CRF. We do not have data on disease progression so we cannot rule out the possibility that some survivors could be under active treatment for disease progression at the time of survey. If so, this could influence the fatigue scores.
In conclusion, three distinct classes of CRF were identified which could be differentiated with sleep quality, anxiety, anhedonia, and lifestyle factors. Better classification of patients and tailoring interventions to patients’ fatigue experiences could enhance the effectiveness of beneficial interventions for CRF currently developed.
References
Barsevick AM, Irwin MR, Hinds P, et al. Recommendations for high-priority research on cancer-related fatigue in children and adults. J Natl Cancer Inst. 2013;105:1432–40.
Bower JE, Ganz PA, Desmond KA, et al. Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer. 2006;106:751–8.
Berger AM, Abernethy AP, Atkinson A, et al. Cancer-related fatigue. J Natl Compr Cancer Netw. 2010;8:904–31.
Cheng KKF, Lee DTF. Effects of pain, fatigue, insomnia, and mood disturbance on functional status and quality of life of elderly patients with cancer. Crit Rev Oncol Hematol. 2011;78:127–37.
Hofman M, Ryan JL, Figueroa-Moseley CD, et al. Cancer-related fatigue: the scale of the problem. Oncologist. 2007;12(Suppl 1):4–10.
Prue G, Rankin J, Allen J, et al. Cancer-related fatigue: a critical appraisal. Eur J Cancer. 2006;42:846–63.
Goedendorp MM, Andrykowski MA, Donovan KA, et al. Prolonged impact of chemotherapy on fatigue in breast cancer survivors: a longitudinal comparison with radiotherapy-treated breast cancer survivors and noncancer controls. Cancer. 2012;118:3833–41.
Yennurajalingam S, Bruera E. Review of clinical trials of pharmacologic interventions for cancer-related fatigue: focus on psychostimulants and steroids. Cancer J. 2014;20:319–24.
Cramp F, Byron-Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;11:CD006145.
Goedendorp MM, Gielissen MF, Verhagen CA, et al. Psychosocial interventions for reducing fatigue during cancer treatment in adults. Cochrane Database Syst Rev. 2009;21:CD006953.
de Raaf PJ. Cancer-related fatigue: a multi-dimensional approach. Rotterdam: P.J. de Raaf; 2013.
Scott JA, Lasch KE, Barsevick AM, et al. Patients’ experiences with cancer-related fatigue: a review and synthesis of qualitative research. Oncol Nurs Forum. 2011;38:E191–203.
de Raaf PJ, de Klerk C, van der Rijt CCD. Elucidating the behavior of physical fatigue and mental fatigue in cancer patients: a review of the literature. Psychooncology. 2013;22:1919–29.
de Raaf PJ, de Klerk C, Timman R, et al. Differences in fatigue experiences among patients with advanced cancer, cancer survivors, and the general population. J Pain Symptom Manag. 2012;44:823–30.
Wright F, D’Eramo Melkus G, Hammer M, et al. Trajectories of evening fatigue in oncology outpatients receiving chemotherapy. J Pain Symptom Manag. 2015;50:163–75.
Wright F, D’Eramo Melkus G, Hammer M, et al. Predictors and trajectories of morning fatigue are distinct from evening fatigue. J Pain Symptom Manag. 2015;50:176–89.
Janssen-Heijnen MLG, Louwman WJ, Van de Poll-Franse LV, et al. Results of 50 years cancer registry in the south of the Netherlands: 1955–2004 (in Dutch). Eindhoven: Eindhoven Cancer Registry; 2005.
Smets EMA, Garssen B, Bonke B, et al. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39:315–25.
van de Poll-Franse LV, Horevoorts N, Van Eenbergen MC, et al. The patient reported outcomes following initial treatment and long term evaluation of survivorship registry: scope, rationale and design of an infrastructure for the study of physical and psychosocial outcomes in cancer survivorship cohorts. Eur J Cancer. 2011;47:2188–94.
Smets EM, Garssen B, Cull A, et al. Application of the multidimensional fatigue inventory (MFI-20) in cancer patients receiving radiotherapy. Br J Cancer. 1996;73:241–5.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
Olsson I, Mykletun A, Dahl AA. The hospital anxiety and depression rating scale: a cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry. 2005;5:46.
Denollet J, Pedersen SS, Daemen J, et al. Reduced positive affect (anhedonia) predicts major clinical events following implantation of coronary-artery stents. J Intern Med. 2008;263:203–11.
Damen NL, Pelle AJ, Boersma E, et al. Reduced positive affect (anhedonia) is independently associated with 7-year mortality in patients treated with percutaneous coronary intervention: results from the RESEARCH registry. Eur J Prev Cardiol. 2013;20:127–34.
Buysse DJ, Reynolds Iii CF, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res. 1998;45:5–13.
Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
Fayers PM, Aaronson NK, Bjordal K, et al. EORTC QLQ-C30 scoring manual, vol. 11. Brussels; 1995. p. 1–49.
Pols MA, Peeters PH, Ocke MC, et al. Estimation of reproducibility and relative validity of the questions included in the EPIC Physical Activity Questionnaire. Int J Epidemiol. 1997;26(Suppl 1):S181–9.
Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80.
Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–504.
Sangha O, Stucki G, Liang MH, et al. The Self-administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156–63.
UICC: TNM Atlas illustrated guide to the TNM/pTNM classification of malignant tumors, 7th ed. Chichester: Wiley-Blackwell; 2009.
Holzner B, Kemmler G, Greil R, et al. The impact of hemoglobin levels on fatigue and quality of life in cancer patients. Ann Oncol. 2002;13:965–73.
Vermunt JK, Magidson J. Latent Gold 5.0 upgrade manual. Belmont: Statistical Innovations; 2013.
Magidson J, Vermunt JK. Latent class models. In: Kaplan D, editor. The Sage handbook of quantitative methodology for the social sciences. Thousand Oaks: Sage Publications; 2004. p. 175–98.
Bennett BK, Goldstein D, Chen M, et al. Characterization of fatigue states in medicine and psychiatry by structured interview. Psychosom Med. 2014;76:379–88.
Kim HJ, Barsevick AM, Fang CY, et al. Common biological pathways underlying the psychoneurological symptom cluster in cancer patients. Cancer Nurs. 2012;35:E1–E20.
Bower JE, Ganz PA, Irwin MR, et al. Inflammation and behavioral symptoms after breast cancer treatment: do fatigue, depression, and sleep disturbance share a common underlying mechanism? J Clin Oncol. 2011;29:3517–22.
Rich T, Innominato PF, Boerner J, et al. Elevated serum cytokines correlated with altered behavior, serum cortisol rhythm, and dampened 24-hour rest-activity patterns in patients with metastatic colorectal cancer. Clin Cancer Res. 2005;11:1757–64.
Miaskowski C, Dodd M, Lee K, et al. Preliminary evidence of an association between a functional interleukin-6 polymorphism and fatigue and sleep disturbance in oncology patients and their family caregivers. J Pain Symptom Manag. 2010;40:531–44.
Grimmett C, Bridgewater J, Steptoe A, et al. Lifestyle and quality of life in colorectal cancer survivors. Qual Life Res. 2011;20:1237–45.
Koutoukidis DA, Knobf MT, Lanceley A. Obesity, diet, physical activity, and health-related quality of life in endometrial cancer survivors. Nutr Rev. 2015;73:399–408.
Mustian KM, Alfano CM, Heckler C, et al. Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: a meta-analysis. JAMA Oncol. 2017.
Gielissen MFM, Verhagen S, Witjes F, et al. Effects of cognitive behavior therapy in severely fatigued disease-free cancer patients compared with patients waiting for cognitive behavior therapy: a randomized controlled trial. J Clin Oncol. 2006;24:4882–7.
Garland SN, Johnson JA, Savard J, et al. Sleeping well with cancer: a systematic review of cognitive behavioral therapy for insomnia in cancer patients. Neuropsychiatr Dis Treat. 2014;10:1113–24.
Lengacher CA, Reich RR, Paterson CL, et al. Examination of broad symptom improvement resulting from mindfulness-based stress reduction in breast cancer survivors: a randomized controlled trial. J Clin Oncol. 2016;34:2827–34.
Dennett AM, Peiris CL, Shields N, et al. Moderate-intensity exercise reduces fatigue and improves mobility in cancer survivors: a systematic review and meta-regression. J Physiother. 2016;62:68–82.
Whitehead L. The measurement of fatigue in chronic illness: a systematic review of unidimensional and multidimensional fatigue measures. J Pain Symptom Manag. 2009;37:107–28.
Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332:1080.
Reeves WC, Wagner D, Nisenbaum R, et al. Chronic fatigue syndrome—a clinically empirical approach to its definition and study. BMC Med. 2005;3:19.
Acknowledgements
We thank all survivors and their doctors for their participation in the study. Special thanks are to Dr. M van Bommel for her availability as an independent advisor and her willingness to answer survivors’ queries. In addition, we thank the following hospitals for their cooperation: Amphia Hospital (Breda), Bernhoven Hospital (Veghel and Oss), Catharina Hospital (Eindhoven), Elkerliek Hospital (Helmond), Jeroen Bosch Hospital (‘s-Hertogenbosch), Maxima Medical Center (Eindhoven and Veldhoven), St Anna Hospital (Geldrop), St Elisabeth Hospital (Tilburg), Twee Steden Hospital (Tilburg and Waalwijk), and VieCuri Hospital (Venlo and Venray).
Funding
The data collection of this study was funded in part by a VENI grant from the Netherlands Organization for Scientific Research (#451-10-041) awarded to Dr. Floortje Mols, and a Medium Investment Grant from the Netherlands Organisation for Scientific Research (NWO#480-08-009), The Hague, and The Netherlands. Dr. Olga Husson (KUN2015-7527) is supported by a Social Psychology Fellowship from the Dutch Cancer Society, and Dr. Floortje Mols is supported by a VENI grant (#451-10-041) from the Netherlands Organization for Scientific Research. These funding agencies had no further role in study design, in the collection, analysis, and interpretation of data, in the writing of the report, and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval for the study was obtained from a local certified Medical Ethics Committee of the Maxima Medical Centre Veldhoven.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Thong, M.S.Y., Mols, F., van de Poll-Franse, L.V. et al. Identifying the subtypes of cancer-related fatigue: results from the population-based PROFILES registry. J Cancer Surviv 12, 38–46 (2018). https://doi.org/10.1007/s11764-017-0641-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-017-0641-0