Abstract
Pseudoaneurysms of the profunda femoris artery have been reported following different types of trauma and from orthopedic procedures performed in the proximal femur. Two cases of profunda femoris artery pseudoaneurysm with two rare causes are presented. The first one is a core decompression of femoral head for osteonecrosis and the second one is a proximal femur fracture nailing. Awareness and careful follow-up are the key issues for the early diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
We present two cases of profunda femoris artery pseudoaneurysm with two rare causes. The first case is a core decompression of the hip for osteonecrosis and the second one is a femur fracture treated with an intramedullary nailing device. Thigh swelling, bleeding from the wound and falling hemoglobin level should be warning for the early recognition and effective treatment.
Pseudoaneurysms of the profunda femoris artery have been reported following different types of trauma and from orthopedic procedures performed in the proximal femur [1–4]. These are rare injuries and in our knowledge this is the first case reported as the femoral head core decompression as a cause. In this paper, we are presenting our two pseudoaneurysm cases. The first one is a core decompression of femoral head for osteonecrosis and the second one is a proximal femur fracture nailing.
Case reports
Case 1
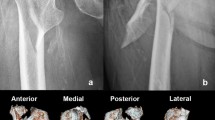
A 32-year-old female with multiple sclerosis presented with thigh pain and weakness in the left lower extremity for 3 months. She had a history of occasional use of methylprednisolone in the last 3 years for her relapse periods. Physical examination revealed limitation of motion of the left hip. The conventional laboratory data including prothrombin time (PT), International Normalized Ratio (INR), activated partial prothromboplastin time (aPTT), complete blood cell count, urine analysis and liver function tests were normal. Plain radiographs disclosed no pathologic changes of the left femoral head. MRI showed abnormal signal intensities in the superior regions of the left and right femoral head consistent with avascular necrosis (Fig. 1). Two stage core decompressions were planed for the bilateral femoral head avascular necrosis. The left side was first to be operated because of the pain with using a lateral incision. During the surgery, lancet was gone deeper than expected for the fascial incision but no bleeding was observed. The rest of the operation was carried out as usual. On the 4th postoperative day the patient developed an intense thigh swelling accompanied with bleeding from the surgical wound. Her hemoglobin levels fell from 12.1 to 7.9 g/dl. Then, an angiogram was performed which revealed a pseudoaneurysm from the profunda femoris artery (Fig. 2). This was successfully and selectively embolised with coil. The patient was discharged 7 days after her embolization with recovery.
Case 2
A 34-year-old male pedestrian sustained several injuries in a road traffic accident, including left subtrochanteric femur fracture and ipsilateral tibia shaft fracture. There were no other abdominal or thoracic injuries. Preoperatively laboratory values included a PT, INR, aPTT, complete blood cell count, urine analysis and liver function tests were normal. He underwent surgery on the next day with closed short gamma nailing of the left subtrochanteric femur fracture and closed intramedullary nailing of the ipsilateral tibia shaft fracture. Postoperative radiographs showed adequate reduction of both fractures. The patient recovered well after surgery and started a rehab protocol.
On the 7th day, the patient started to bleed profusely from the femoral nailing wound with the appearance of a large thigh swelling. Hemoglobin level fell from 11.7 to 8.1 g/dl in 24 h. An angiogram was scheduled and performed on the same day which revealed a pseudoaneurysm from the profunda femoris artery with extravasation of contrast (Fig. 3). This was successfully and selectively embolized with glue (N-butyl-2-cyanoacrylate). No additional problems were encountered. The patient was discharged from the hospital 10 days after the embolization.
Discussion
Case 1 is the first reported case of profunda femoris artery pseudoaneurysm in case of core decompression for hip osteonecrosis to our knowledge. The cause of this pseudoaneurysm seems to be the lancet, which had gone deeper than expected during the fascial incision. There are different causes for this condition reported in the literature. Damage of the femoral arterial system may have occurred at the time of injury. Arterial damages can occur because of bone spikes, tip of the screws, drills, displaced implants and retraction of surrounding tissue [1–5]. We thought that the cause of the second pseudoaneurysm case might be the bone spikes, because the region of the pseudoaneurysm was too close to the fracture side and far from the surgical area.
The time to diagnose in our cases is shorter than the ones reported in the literature [1–3, 5]. In last 8 years, four angiographies performed for the cases with proximal thigh swelling, bleeding from the wound and falling hemoglobin level after the operative procedures. Three out of four had positive results; two of them were pseudoaneurysm and one was injury of artery. The follow-up is important for early diagnosis of pseudoaneurysm. Thigh swelling, bleeding from the wound and falling hemoglobin level are the important warning signs. This condition may be inevitable despite of meticulous surgical technique. Awareness and careful follow-up are the key issues for the early diagnosis.
Conclusion
The diagnosis of pseudoaneurysm of femoral artery following trauma and orthopedic procedures requires awareness and a high index of suspicion. Due to the rarity of the condition, in case of suspicion, the early use of angiography is highly recommended. Although surgical procedures like core decompression are considered as simple procedures, previously described symptoms should arouse suspicion for a possible occurrence of pseudoaneurysm.
References
Chong KC, Yap EC, Lam KS, Low BY (2004) Profunda femoris artery pseudoaneurysm presenting with triad of thigh swelling, bleeding and anemia. Ann Acad Med Singapore 33:267–269
Alwhouhayb M, Howard A (2005) A false aneurysm mistaken for a DVT after hip surgery. Ulus Travma Acil Cerrahi Derg 11:178–179
Smejkal K, Zvak I, Trlica J, Raupach J, Neumann J (2007) Traumatic pseudoaneurysm of arteria femoralis profunda—the case report. Rozhl Chir 86:116–119
Canbaz S, Acipayam M, Gurbuz H, Duran E (2002) False aneurysm of perforating branch of the profunda femoris artery after external fixation for a complicated femur fracture. J Cardiovasc Surg 43:519–521
Yang KH, Park HW, Park SJ (2002) Pseudoaneurysm of the superficial femoral artery after closed hip nailing with a Gamma nail: report of a case. J Orthop Trauma 16:124–127
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Unay, K., Poyanli, O., Akan, K. et al. Profunda femoris artery pseudoaneurysm after surgery and trauma. Strat Traum Limb Recon 3, 127–129 (2008). https://doi.org/10.1007/s11751-008-0043-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11751-008-0043-y