Abstract
The incidence of hip fractures continues to rise. This study is the first evaluation of a new intramedullary implant, the Veronail, that provides double axis fixation into the femoral head and allows the surgeon to choose whether to use sliding or fixed locked proximal screw fixation for trochanteric femoral fractures. The fractures were classified according to the AO classification, and function was assessed with the Modified Harris Hip Score. 111 patients with trochanteric fractures were evaluated in eight Italian hospitals. The stable 31.A1 fractures were treated with sliding proximal screws, the subtrochanteric 31.A3 fractures with converging proximal screws, and the unstable 31.A2 fractures were treated with both types of proximal fixation. The unstable fractures treated with locked converging screws had the same function at one year as those treated with sliding screws. This study suggests a possible new method of treating unstable trochanteric femoral fractures. This may be the solution to prevent excessive collapse of the fracture with the resultant poor function and persisting pain noted in the literature. Two converging locked proximal screws seem to provide stable fixation in 31.A2 femoral fractures and produce as good a result as the use of traditional sliding screws. The role of converging locked proximal screws in unstable trochanteric fractures requires further evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of proximal femoral fractures has increased significantly in recent years and is expected to continue to rise with increasing life expectancy [10, 13, 17]. In 1990 there were approximately 1.7 million proximal femoral fractures worldwide and the projected estimate for 2050 approaches 6.3 million [20]. The effect of these fractures is frequently devastating [19]; the social impact is high and the relative costs of treatment are increasing. For these reasons methods of osteosynthesis that will permit early mobilization and a rapid return to pre-injury levels of independence are sought by surgeons who treat these patients.
Although the treatment success of hip fractures using modern sliding implants has improved compared with rigid implants [16], considerable morbidity and mortality still exist especially in comminuted and unstable fractures. Excessive sliding of the femoral neck screw has been associated with suboptimal results [1, 18]. At the December 2005 meeting of the AAOS Evidence Based Practice Committee, it was reported that 18–33% of hip fracture patients die within 1 year and 25–75% do not gain pre-fracture function [9]. A single-centre analysis of 1,024 patients with pertrochanteric fractures treated with the DHS reported satisfactory results, but the 12 month mortality rate documented was 31% and the proportion of the surviving patients walking, independently or with walking aides, at 1 year was 51% [4].
In this prospective multi-centre study, the authors investigated the ease of use, post-operative results and complication rate of a new intramedullary device, the Veronail Trochanteric System, for pertrochanteric fractures of the proximal femur. A unique feature that distinguishes this implant from other double-axis systems is the alternative configuration of the cephalic screws, with either two parallel sliding screws or two convergent screws locked to the nail. This design allows the surgeon to select, depending on the degree of stability present once the fracture is reduced, the configuration of screws to use. It was hypothesized that the full range of pertrochanteric fractures could be treated satisfactorily with an intramedullary device that offers either a double-axis sliding or locked converging pattern of screws into the femoral neck.
Materials and methods
Surgical technique
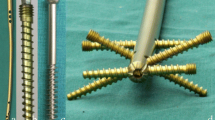
The implant used in this study was the Veronail (Orthofix Srl, Bussolengo, Italy). This is an intramedullary device which is 200 mm long with a proximal diameter of 15 mm and a distal diameter of 10 mm. The nail allows the use of two different proximal fixation options (Fig. 1): two parallel cephalic sliding screws or two converging fixed screws. The parallel sliding screws consist of two screws with an integral sleeve which are inserted together: each sleeve is first screwed into and locked to the nail, and then the 7 mm screw is advanced into the femoral head under X-ray control. This allows 10–40 mm of sliding (depending on the length of the screw) but without risk of the screw disengaging from the sleeve. The second proximal locking option utilises two converging screws without sleeves. These are inserted using the same guide handle as the sliding screws but with the proximal converging screw using a separate guide hole in the handle. The converging screws are locked firmly into the nail and provide secure locked fixation of the femoral neck and head. The two types of screws are colour-coded and it is important that they are not mixed. The choice of the proximal configuration therefore depends on the clinical and biomechanical characteristics of the fracture and of the patient. Fractures considered stable can be treated with the sliding configuration while unstable fractures may benefit from the use of convergent locked proximal screws. Surgeons would opt to use the fixed convergent proximal locking option if they considered there was risk of excessive collapse. Converging screws may also be used on the rare occasions when the femoral neck is too narrow to accommodate two parallel screws and for subtrochanteric fractures which are known to benefit from strong fixation with an intramedullary device [9].
Distal locking can be either static or dynamic at the discretion of the treating surgeon and according to the bone quality and fracture type. With these exceptions to the proximal and distal screw configurations, all patients were treated using the same protocol; they were mobilised as rapidly as their condition would allow, with weight-bearing as tolerated and full weight-bearing permitted early or as soon as deemed feasible by the treating institution protocol.
One hundred and eleven patients with proximal femoral fractures were prospectively evaluated in 8 Italian hospitals. Using the AO classification type A1 fractures are considered stable and type A3 unstable. With type A2 fractures the degree of instability is variable and is dependent on comminution. Some fractures remain very unstable even when fully reduced.
Pre-injury activity and functional levels were recorded using the modified Harris hip score (MHHS, Harris 1969, Fig. 2); the section on evaluation of hip movements by hospital personnel was omitted and replaced with follow-up telephone interviews [14]. The fracture was classified according to the AO and the distribution of fracture types and proximal screw configurations are shown in Table 1.
All patients received peri-operative antibiotics and antithromboembolic prophylaxis (with low-molecular weight heparin) in accordance with hospital protocols. Other data were recorded as in Tables 1 and 2.
All patients were enrolled into a rehabilitation programme for at least 30 days and were reviewed at 6 weeks, 4 months and 1 year after surgery using functional evaluations (MHHS, weight-bearing status achieved).
Statistical analysis
Data were entered into an Excel (Microsoft Office 2003) spreadsheet and imported into SAS v 9.1 (SAS, Carey, NC, USA) for statistical analysis. Descriptive analysis was based on the total number of subjects with data available at each time point. Univariate analysis of dichotomous data was conducted using Chi-square tests while continuous data were analyzed using Student’s t-test or Mann–Whitney U test as appropriate. Statistical significance was determined at a P value < 0.05.
Results
The mean age of the 111 patients was 79.3 years (47–97); 81 (73%) were female and 30 (27%) male. Fracture types were distributed as shown in Table 1. The mean time for surgery (incision to closure) was 46 min (20–120). Reaming of the diaphysis to 11 mm was necessary in only 5 cases (4.5%).
Post-operative blood transfusions were required in 42 patients (37.8%) with an average of 1.6 units (1–4) used per patient transfused. The overall transfusion requirement for the whole sample was 0.60 units per patient. The mean hospital stay was 7 days (5–14). The operative details as stratified by fracture type are reported in Table 1.
Fifteen patients (13.5%) died in the first year, 5 (4.5%) had a complication that necessitated hardware removal and in one patient (0.9%) the final evaluation could not be carried out due to amputation related to diabetes. Nineteen patients (17.1%) could not be contacted were lost at the 1 year review. The remaining 71 (64%) patients were assessed at 1 year for final review either at a hospital visit or through a telephone interview. Figures 3 and 4 show examples of fracture union of two patients treated with the parallel and converging proximal screw configurations, respectively.
The mean pre-operative MHHS was 73 (with a maximum of 91). This value was used to determine a relative percentage in the return to pre-trauma activity levels as shown in Fig. 5.
Screw cut out occurred in five cases (4.5%). Two were in type A1 fractures with one treated with parallel sliding screws and the other treated with converging screws; two in type A2 fractures treated with parallel sliding screws. The fifth patient developed screw cut out a few days after surgery. This was in an A3 fracture noted to have intra-articular penetration of the locked convergent screws (Table 2). All remaining fractures healed uneventfully without any reported instances of infection, pseudoarthrosis, or implant failures. There was no association between the method of proximal configuration and risk of cut out (P = 0.9) but distal locking configurations showed a smaller risk if used in dynamic mode (P = 0.004).
Analysis of variables associated with weight-bearing demonstrated that two factors were influential- the pre-operative MHHS and body mass index. Figures 6 and 7 suggest that weight-bearing ability is associated with pre-operative health as reported previously. This study also shows that the pre-injury modified HHS has a strong relationship to the weight-bearing ability at 12 months and that a lower BMI at presentation was predictive of poor function at 12 months.
When these variables were included in a logistic regression model that controlled for the body mass index, the study centre, methods of proximal and distal locking configuration and fracture type, the model was predictive (P = .009) of full weight bearing ability. The only factor independently associated with this outcome was the pre-operative MHHS (OR 1.107, 95% CI 1.023–1.197).
Figure 8 shows the changes of the MHHS by fracture type over 12 months. Although, as might be expected, the unstable A2 fractures had a lower score at discharge, the difference disappears thereafter and the A2 fractures had as good an MHHS score at 12 months as did the A1 fractures.
Discussion
The treatment of proximal femoral fractures using fixed angled implants was succeeded by sliding screw devices which produced an improvement in union rates and fewer fixation and implant failures [12, 15]. A meta-analysis of 14 studies with 3,069 patients showed an increased risk of cut-out (13% vs. 4%), non-union (2 vs. 0.5%), implant breakage (14 vs. 0.7%) and re-operation (10 vs. 4%) for fixed nail plates in comparison with the sliding implants [8]. In addition patients treated with fixed nail plates had a higher mortality rate and survivors more likely to have residual hip pain and impaired mobility. For the past 3 decades the use of sliding screw implants for the fixation of proximal femoral fractures has been almost universal. Two main designs are popular; an extramedullary device (e.g., the Dynamic Hip Screw, DHS) and an intramedullary device (the Gamma nail and equivalent cephalo-medullary constructs). Both types achieve fixation in the femoral head with one or two sliding screws. Extensive clinical investigation has failed to show that either type of device is superior although there is the suggestion that intramedullary devices may be biomechanically more stable [2, 3, 21–24, 26–28].
Alternatives to the sliding screw designs have been proposed for the treatment of unstable hip fractures. Rigid fixation with a reinforced device was reported to allow fracture healing without settling in intertrochanteric fractures in a 358 patient study [25]. Further analysis reported that 82% in this series obtained good or excellent results with no difference between stable or unstable fractures.
This study highlights several points in this vulnerable group of patients at the different stages of management.
Pre-operative
Health status of the subject prior to trauma appears to influence the primary outcome of ability to weight-bear following fracture repair. While this has been implied by earlier studies [7] and recent evidence [11], this study adds that two further objective measures, namely the MHHS and body mass index, establish the association more definitely.
Intraoperative
The percentage of patients who required a transfusion (37.8%) and the mean amount transfused for the whole group (0.60 units) was at the lower end of previous published results as was the duration of surgery (mean 47 min) [2, 21, 25]. The reasons for the lower morbidity may be implant related; the smaller nail diameter and screws used (as compared with other devices) leads to a reduced need for reaming of the intramedullary canal which, in this series, was required in only 5% of cases. It must be acknowledged that these better results may also be related to the gradual improvement of the peri- and post-operative care of elderly patients.
Postoperative
Average hospitalisation was 7 days and was dependent on social factors and hospital protocols. Of the 54 AO 31.A2 fractures, 23 were treated with parallel and 31 with converging proximal screws. The converging configuration of proximal screws, as used in type A3 fractures and the more unstable type A2 fractures (when the lateral wall proved to be particularly at risk), seemed to withstand the tendency of these fractures to collapse. In this series there were no implant failures or non-unions in the very unstable fractures; additionally, the unstable A2 fractures did as well as the stable A1 fractures.
Functional assessment
An improvement to 46% of the pre-operative modified Harris score was achieved during the hospitalisation period—this increased to 86% after 4 months. The percentage of all the patients at 1 year who were walking independently or with one stick was 52%. This compares very favourably with other published studies; in the largest single series of patients treated with the DHS this was 35.1% [9]. Another study that used the same criteria for mobility at 12 months found that 29% of their total number of patients was walking independently or with one stick at 1 year [2]. This suggests a possible association with better mobility (at 1 year) from stabilisation with this device.
No patients required hardware removal for pain on the lateral side of the thigh and there were no fractures distal to the nail, lending support to recent articles suggesting that the reduced diameter of modern trochanteric nails may be influencing the incidence of these complications [29, 31]. Coupled to the absence of implant failures in this series (there were no nail or screw breakages), there is now evidence that reduced diameter implants can provide adequate stability for immediate load-bearing even in unstable fractures.
We were unable to find an association between the type of fracture and post-operative walking ability (P = 0 .73). Previous studies have shown that a significant proportion of the more unstable 31A.2 fractures suffer from variable degrees of collapse and femoral shaft medialisation and that a high proportion of these patients go on to have poor function [5, 6, 30]. In this study patients who had sustained A2 fractures had equally good functional recovery as those with A1 fractures at 12 months. All patients with type A3 fractures were also without gait disturbance at 12 months. Further post-hoc analysis suggested that these patients with type A3 fractures maintained a higher MHHS throughout the observation period.
Conclusion
The treatment of stable fractures with a Veronail using a parallel sliding cephalic configuration of screws produced a similar complication rate to that experienced with other intramedullary nailing systems and for stable fractures treated with a DHS plate. The high stability, low incidence of mechanical complications and minimal invasiveness of this device are favourable factors supporting its use.
The fixation of unstable fractures with the Veronail using a converging cephalic configuration of screws represents a new solution in the search for the correct compromise between initial stability, minimal invasiveness and permitted immediate load-bearing. It protects the biological healing potential of the fracture site and minimises the classic complications of screw cut out, collapse and gait disturbance seen in these fractures The elasticity within the nail favours fracture healing (0% non-union rate), even when used with the cephalic convergent configuration of proximal screws, and may prevent secondary deformities which frequently occur in unstable fractures treated with a cephalic sliding configuration. The functional results at 1 year compare favourably with other published results.
These results demonstrate the Veronail can be adapted to the various patterns of proximal femoral fractures and its use is compatible with a good outcome in terms of healing, recovery of pain-free walking ability and a low incidence of complications. The results from this multi-centre study are promising and appear to challenge the established indications of the use of sliding implants. Fifty-seven percent of the 31.A2 fractures treated here with a fixed implant that did not allow sliding revealed 1-year mobility outcomes that were better than previously published figures. The initial hypothesis that this new device, owing to the adaptable configuration of proximal and distal locking screw options, may be suited to all types of pertrochanteric fractures is supported by these initial results. Further studies are required to define which combination of such screw configurations, both proximal and distal, are most appropriate for the different fracture types.
References
AAOS Bulletin (2005) vol 53, No. 6
Adams CI, Robinson CM, Court-Brown CM, McQueen MM (2001) Prospective randomized controlled trial of an intramedullary nail versus dynamic hip screw and plate for intertrochanteric fractures of the femur. J Orthop Trauma 15:394–400
Ahrengart L, Tornkvist H, Fornander P et al (2002) A randomized study of the compression hip screw and Gamma nail in 426 fractures. Clin Orthop Relat Res 401:209–222
Baixauli F, Vicenti V, Baixauli E et al (1999) A reinforced rigid fixation device for unstable intertrochanteric fractures. Clin Orthop 361:205–215
Bendo JA, Weiner LS, Strauss E, Yang E (1994) Collapse of intertrochanteric hip fractures fixed with sliding screws. Orthop Rev Aug (Suppl):30–37
Bolhofner BR, Russo PR, Carmen B (1999) Results of intertrochanteric femur fractures treated with a 135-degree sliding screw with a two-hole side plate. J Orthop Trauma 13(1):5–8
Broos PL, Stappaerts KH, Luiten EJ, Gruwez JA (1988) Home-going: prognostic factors concerning the major goal in treatment of elderly hip fracture-patients. Int Surg 73(3):148–150
Chinoy MA, Parker MJ (1999) Fixed nail plates versus sliding hip systems for the treatment of trochanteric femoral fractures: a meta analysis of 14 studies. Injury 30(2):157–163
Chirodian N, Arch B, Parker M (2005) Sliding hip screw fixation of trochanteric hip fractures: outcome of 1024 procedures. Injury 36:793–800
Cooper C, Campion G, Melton LJ 3rd (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2:285–289
Ensrud KE, Ewing SK,Taylor BC et al (2007) Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol 62A(7):744–751
Esser MP, Kassab JY, Jones DHA (1986) Trochanteric fractures of the femur: a randomised prospective trial comparing the Jewett nail-plate with the dynamic hip screw. J Bone Joint Surg (Br) 68B(4):557–560
Gullberg B, Duppe H, Nilsson B et al (1993) Incidence of hip fractures in Malmö, Sweden (1950–1991). Bone 14(Suppl 1):23–29
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51(4):737–755
Heyse-Moore GH, Maceachern AG, Jameson Evans DC (1983) Treatment of intertrochanteric fractures of the femur: a comparison of the Richards screw-plate with the Jewett nail-plate. J Bone Joint Surg (Br) 65(3):262–267
Jacobs RR, McClain O, Armstrong HJ (1980) Internal fixation of intertrochanteric hip fractures: a clinical and biomechanical study. Clin Orthop 146:62–70
Kannus P, Oarkkari J, Sievänen H et al (1996) Epidemiology of hip fractures. Bone 18(Suppl 1):57–63
Kim WY, Han C-H, Park J-I, Kim JY (2001) Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop 25(6):360–362
Koval KJ, Zuckerman JD (2001) Intertrochanteric fractures. In: Rockwood and Green’s fractures in adults, 5th edn, vol 2, pp 1635–1663
Lauritzen JB (1996) Hip fractures: incidence, risk factors, energy absorption, and prevention. Bone 18(1 Suppl):65S–75S
Leung KS, So WS, Shen WY, Hui PW (1992) Gamma nails and dynamic hip screws for peritrochanteric fractures. A randomised prospective study in elderly patients. J Bone Joint Surg Br 74(3):345–351
Miedel R, Ponzer S, Törnkvist H et al (2005) The standard Gamma nail or the Medoff sliding plate for unstable trochanteric and subtrochanteric fractures. A randomised, controlled trial. J Bone Joint Surg Br 87(1):68–75
Pajarinen J., Lindahl J, Michelsson O et al (2005) Pertrochanteric femoral fractures treated with a dynamic hip screw or a proximal femoral nail. A randomised study comparing post-operative rehabilitation. J Bone Joint Surg Br 87(1):76–81
Parker MJ, Handoll HHG (2000) Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures (Cochrane review). In: The Cochrane library, vol 4, Oxford, update software
Sadowski C, Lübbeke A, Saudan M et al (2002) Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: a prospective, randomized study. J Bone Joint Surg Am 84A(3):372–381
Saudan M, Lübbeke A, Sadowski C et al (2002) Pertrochanteric fractures: is there an advantage to an intramedullary nail? A randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma 16(6):386–393
Schipper IB, Marti RK, van der Werken C (2004) Unstable trochanteric femoral fractures: extramedullary or intramedullary fixation. Review of literature. Injury 35(2):142–151
Schipper IB, Steyerberg EW, Castelein RM et al (2004) Treatment of unstable trochanteric fractures. Randomised comparison of the Gamma nail and the proximal femoral nail. J Bone Joint Surg Br 86(1):86–94
Simmermacher RKJ, Bosch AM, Van der Werken Chr (1999) The AO/ASIF-proximal femoral nail (PFN): a new device for the treatment of unstable proximal femoral fractures. Injury 30:327–332
Stappaerts KH, Deldycke J, Broos et al (1995) Treatment of unstable peritrochanteric fractures in elderly patients with a compression hip screw or with the Vandeputte (VDP) endoprosthesis: a prospective randomized study. J Orthop Trauma 9(4):292–297
Utrilla AL, Reig JS, Muñoz FN et al (2005) Gamma nail and compression hip screw for trochanteric fractures a randomized, prospective, comparative study in 210 elderly patients with a new design of the Gamma nail. J Orthop Trauma 19:229–233
Author information
Authors and Affiliations
Corresponding author
Additional information
Ethical consideration: This work has been approved, where necessary, by the appropriate ethical committees of the institutions where the study has been performed. Subjects gave informed consent prior to participation in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lavini, F., Renzi-Brivio, L., Aulisa, R. et al. The treatment of stable and unstable proximal femoral fractures with a new trochanteric nail: results of a multicentre study with the Veronail. Strat Traum Limb Recon 3, 15–22 (2008). https://doi.org/10.1007/s11751-008-0035-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11751-008-0035-y