Abstract
Objectives
We conducted a multi-institutional prospective observational study of elderly patients (≥ 75 years-old) with resected non-small cell lung cancer. In this report, we have followed the cohorts for 2 years after surgery and examined both the influence of preoperative comorbidity [Adult Comorbidity Evaluation-27 (ACE-27) index] on the postoperative survival and the change in the Karnofsky Performance Status (KPS).
Methods
From March 2014 to April 2015, 264 patients were prospectively registered from 22 hospitals affiliated with the National Hospital Organization. The mean age at the time of surgery was 79.3 years (range 75–90 years), and 41% of the patients were ≥ 80 years of age. A total of 26% underwent sublobar resection. The study endpoints were the postoperative overall survival (OS), its prognostic factors, and the changes in the postoperative KPS.
Results
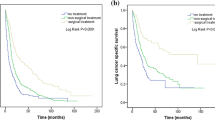
The 2-year OS was 85.3% (95% confidence interval 80.4–89.1%). Male gender, age ≥ 80, a smoking history, grade 2 of ACE-27, and an advanced disease stage were significantly poor prognostic factors for the OS in the univariate risk analysis. The multivariate analysis showed that male gender, age ≥ 80, an advanced disease stage and sublobar resection were significantly poor prognostic factors for the OS. In comparison with the preoperative KPS, no marked decline was observed in the postoperative chorological change of KPS.
Conclusions
In the surgical treatment of elderly patients, the comorbidity as assessed by the ACE-27 index might affect the postoperative survival, and therefore should be taken into accounts in the preoperative evaluation of the surgical indications.




Similar content being viewed by others
References
Sawabata N, Nagayasu T, Kadota Y, Goto T, Horio H, Mori T, et al. Risk assessment of lung resection for lung cancer according to pulmonary function: republication of systematic review and proposals by guideline committee of the Japanese association for chest surgery 2014. Gen Thorac Cardiovasc Surg. 2015;63:14–21.
Yano T, Yokoyama H, Fukuyama Y, Takai E, Mizutani K, Ichinose Y. The current status of postoperative complications and risk factors after a pulmonary resection for primary lung cancer—a multivariate analysis. Eur J Cardiothorac Surg. 1997;11:445–9.
Okami J, Higashiyama M, Asamura H, Goya T, Koshiishi Y, Sohara Y, et al. Japanese Joint Committee of Lung Cancer Registry. Pulmonary resection in patients aged 80 years or over with clinical stage I non-small cell lung cancer: prognostic factors for overall survival and risk factors for postoperative complications. J Thorac Oncol. 2009;4:1247–53.
Yano T, Kawashima O, Takeo S, Adachi H, Tagawa T, Fukuyama S, For the National Hospital Organization Network Collaborative Research—Thoracic Oncology Group, et al. A prospective observational study of pulmonary resection for non-small cell lung cancer in patients older than 75 years. Semin Thorac Cardiovasc Surg 2017;29:540–7. https://doi.org/10.1053/j.semtcvs.2017.05.004.
Piccirillo JF, Tierney RM, Costas I, Grove L, Spitznagel EL Jr. Prognostic importance of comorbidity in a hospital-based cancer registry. JAMA. 2004;291:2441–7.
Read WL, Tierney RM, Page NC, Costas I, Govindan R, Spitznagel EL, et al. Differential prognostic impact of comorbidity. J Clin Oncol. 2004;22:3099–103.
Miura N, Kohno M, Ito K, Senba M, Kajiwara K, Hamaguchi N, et al. Lung cancer surgery in patients aged 80 years or older: an analysis of risk factors, morbidity, and mortality. Gen Thorac Cardiovasc Surg. 2015;63:401–5.
Dell’Amore A, Monteverde M, Martucci N, Sanna S, Caroli G, Dolci G, et al. Lobar and sub-lobar lung resection in octogenarians with early stage non-small cell lung cancer: factors affecting surgical outcomes and long-term results. Gen Thorac Cardiovasc Surg 2015;63:222–30.
Dell’Amore A, Monteverde M, Martucci N, Sanna S, Caroli G, Stella F, et al. Early and long-term results of pulmonary resection for non-small-cell lung cancer in patients over 75 years of age: a multi-institutional study. Interact Cardiovasc Thorac Surg. 2013;16:250–6.
Endoh H, Yamamoto R, Satoh Y, Kuwano H, Nishizawa N. Risk analysis of pulmonary resection for elderly patients with lung cancer. Surg Today. 2013;43:514–20.
Umezu H, Miyoshi S, Araki O, Karube Y, Tamura M, Kobayashi S, et al. Efficacy of functional operability algorithm for octogenarians with primary lung cancer. Gen Thorac Cardiovasc Surg. 2012;60:36–42.
Read WL, Tierney RM, Page NC, Costas I, Govindan R, Spitznagel EL, et al. Differential prognostic impact of comorbidity. J Clin Oncol. 2004;122:3099–103.
Kallogjeri D, Piccirillo JF, Spitznagel EL Jr, Steyerberg EW. Comparison of scoring methods for ACE-27: simpler is better. J Geriatr Oncol. 2012;3:238–45.
Fanucchi O, Ambrogi MC, Dini P, Lucchi M, Melfi F, Davini F et al. Surgical treatment of non-small cell lung cancer in octogenarians. Interact Cardiovasc Thorac Surg. 2011;12:749–53.
Camposilvan I, Akhtar-Danesh N, Schneider L, Finley CJ. The effect of surgeon volume on procedure selection in non-small cell lung cancer surgeries. J Thorac Cardiovasc Surg. 2015;150:507–12.
Dhanasopon AP, Salazar MC, Hoag JR, Rosen JE, Kim AW, Detterbeck FC, et al. Fate of pneumonectomy patients variably captured by non-small cell lung cancer staging system. Ann Thorac Surg. 2017;104:1829–36.
Zhang Y, Yuan C, Zhang Y, Sun Y, Chen H. Survival following segmentectomy or lobectomy in elderly patients with early-stage lung cancer. Oncotarget. 2016;7:19081–6.
Brunelli A, Kim AW, Berger KI, Addrizzo-Harris DJ. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: diagnosis and management of lung cancer., 3rd ed.: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143(Suppl):166S–90S.
Brunelli A, Charloux A, Bolliger CT, Rocco G, Sculier JP, Varela G, et al. The European Respiratory Society and European Society of Thoracic Surgeons clinical guidelines for evaluating fitness for radical treatment (surgery and chemoradiotherapy) in patients with lung cancer. Eur J Cardiothorac Surg. 2009;36:181–4.
Acknowledgements
This study was funded by the National Hospital Organization (Tokyo, Japan). The authors declare no conflicts of interest in association with the present study. This manuscript was reviewed by all authors. The corresponding author had full access to the study data and takes full responsibility for the final decision to submit the manuscript. We thank the patients, all of the investigators who participated in the study, and the Data Center at the Kyushu Cancer Center. This manuscript was edited in English by Mr. Brian Quinn, the Official English Medical Editor of the Japan Surgical Society.
Funding
This work was supported by the National Hospital Organization (Tokyo, Japan).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Additional information
Clinical Trial Registration ID: UMIN000021904.
Appendix
Appendix
The participating hospitals that are affiliated with the National Hospital Organization in Japan as follows: Shibukawa Medical Center, Kyushu Medical Center, Hokkaido Cancer Center, Nagasaki Medical Center, Kyushu Cancer Center, Kure Medical Center, Obihiro National Hospital, Shikoku Cancer Center, Tokyo National Hospital, Mito Medical Center, Beppu Medical Center, Yokohama Medical Center, Higashihiroshima Medical Center, Takasaki General Medical Center, Saitama National Hospital, Ureshino Medical Center, Nagara Medical Center, Nishi-Niigata Chuo National Hospital, Asahikawa Medical Center, Tokyo Medical Center, Osaka Medical Center, Kochi National Hospital.
Rights and permissions
About this article
Cite this article
Yano, T., Shimokawa, M., Kawashima, O. et al. The influence of comorbidity on the postoperative survival in elderly (≥ 75 years old) with lung cancer. Gen Thorac Cardiovasc Surg 66, 344–350 (2018). https://doi.org/10.1007/s11748-018-0919-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-018-0919-9