Abstract
Objective
We assessed the efficacy of limited proximal arch replacement for type A acute aortic dissection (AAD) with critical complications.
Methods
Sixty-four patients with average age of 64.5 ± 13.0 years, who were intubated prior to arriving at hospital due to cardiopulmonary arrest, cardiac tamponade, or vital organ mal-perfusion, were divided into two groups: group PA consisted of 52 patients undergoing proximal arch repair with mild hypothermic circulatory arrest; group TA consisted of 12 patients who underwent total arch replacement with moderate hypothermia and selective cerebral perfusion.
Results
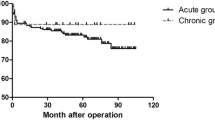
The intimal tear on the distal side of the left subclavian artery was not excised in 11 patients (21.2 %) of group PA. The intimal tear was excised in all patients in group TA. The durations of cerebral protection (PA, 18.7; TA, 70.3 min), cardiopulmonary bypass (PA, 121.5; TA, 206 min), and overall operation (PA, 181.8; TA, 403.8 min) were significantly shorter in group PA. The incidence of postoperative brain damage was significantly lower in group PA (9.6 %) than in group TA (33.3 %). The mortality rate was significantly lower in group PA (5.8 %) than in group TA (58.3 %). Distal arch to descending aortic replacement was required in four patients of group PA during follow-up period. There were no complications or mortality during the reoperation. The actuarial survival rate at 10 years was significantly better in group PA (66.5 %) than in group TA (25 %).
Conclusion
Limited proximal arch repair is suitable for high-risk patients with AAD, despite no excision of the intimal tear.

Similar content being viewed by others
Abbreviations
- AAD:
-
Type A acute aortic dissection
- CPA:
-
Cardiopulmonary arrest
- CT:
-
Computed tomography
- AR:
-
Aortic valve regurgitation
- AMI:
-
Acute myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- LMT:
-
Left main trunk
- CPR:
-
Cardiopulmonary resuscitation
- SD:
-
Standard deviation
References
Hata M, Akiyama K, Hata H, Sezai A, Yoshitake I, Wakui S, et al. Early and mid-term outcome of less invasive quick replacement (LIQR) for type A acute aortic dissection. J Thorac Cardiovasc Surg. 2013;146:119–23.
Kim JB, Chung CH, Moon DH, Ha GJ, Lee TY, Jong SH, et al. Total arch repair versus hemiarch repair in the management of DeBakey type I aortic dissection. Eur J Cardiothorac Surg. 2011;40:881–9.
Mehta RH, Suzuki T, Hagan PG, Bossone E, Gilon D, Llovet A, et al. Predicting death in patients with acute type A aortic dissection. Circulation. 2002;105:200–6.
Bayegan K, Domanovits H, Schillinger M, Ehrlich M, Sodeck G, Laggner AN. Acute type A aortic dissection: the prognostic impact of preoperative cardiac tamponade. Eur J Cardiothorac Surg. 2001;20:1194–8.
Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The International Registry of Acute Aortic Dissection (IRAD); new insights into an old disease. JAMA. 2000;283:897–903.
Amano J, Kuwano H, Yokomise H. Thoracic and cardiovascular surgery in Japan during 2011. Annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2013;2013(61):578–607.
Hata M, Shiono M, Inoue T, Sezai A, Funahashi M, Negishi N, et al. Preoperative cardiopulmonary resuscitation is the only predictor for operative mortality of type A Acute aortic dissection: a recent 8-year experience. Ann Thorac Cardiovasc Surg. 2004;10:101–5.
Kazui T, Washiyama N, Bashar AH, Terada H, Suzuki T, Ohkura K, et al. Surgical outcome of acute type A aortic dissection: analysis of risk factors. Ann Thorac Surg. 2002;74:75–81.
Pugliese P, Pessotto R, Santini F, Montalbano G, Luciani GB, Mazzucco A. Risk of late reoperations in patients with acute type A aortic dissection: impact of a more radical surgical approach. Eur J Cardiothorac Surg. 1998;13:576–80.
Ehrlich MP, Ergin MA, McCullough JN, Lansman SL, Galla JD, Bodian CA, et al. Results of immediate surgical treatment of all acute type A dissection. Circulation. 2000;102(Suppl III):III-248–52.
Greeley WJ, Kern FH, Ungerleider RM, Boyd JL III, Quill T, Smith LR, et al. The effect of hypothermic cardiopulmonary bypass and total circulatory arrest on cerebral metabolism in neonates, infants, and children. J Thorac Cardiovasc Surg. 1991;101:783–94.
Easo J, Weigang E, Hölzl PPF, Horst M, Hoffmann I, Blettner M, et al. Influence of operative strategy for the aortic arch in DeBakey type I aortic dissection: analysis of the German Registry for acute aortic dissection type A. J Thrac Cardiovasc Surg. 2012;144:617–23.
Kazui T, Washiyama N, Muhammad BA, Terada H, Yamashita K, Takinami M, et al. Extended total arch replacement for acute type A aortic dissection: experience with seventy patients. J Thorac Cardiovasc Surg. 2000;119:558–65.
Siono M, Hata M, Sezai A, Niino T, Yagi S, Negishi N. Validity of a limited ascending and hemiarch replacement for acute type A aortic dissection. Ann Thorac Surg. 2006;82:1665–9.
Bachet J, Goudot B, Dreyfus GD, Brodaty D, Dubois C, Delentdecker P, et al. Surgery for acute type A aortic dissection: The Hospital Foch experience (1977–1998). Ann Thorac Surg. 1999;67:2006–9.
Unosawa S, Hata M, Niino T, Shimura K, Shiono S. Prognosis of patients undergoing emergency surgery for type A acute aortic dissection without excision of the intimal tear. J Thorac Cardiovasc Surg. 2013;146:67–71.
Hata M, Sezai A, Niino T, Wakui S, Unosawa S, Minami K, et al. Prognosis for patients with type B acute aortic dissection: risk analysis of early death and requirement for elective surgery. Circ J. 2007;71:1279–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mitsumasa Hata and other coauthors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Hata, M., Orime, Y., Wakui, S. et al. Efficacy of limited proximal arch replacement for type A acute aortic dissection with critical complications. Gen Thorac Cardiovasc Surg 64, 651–656 (2016). https://doi.org/10.1007/s11748-016-0688-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-016-0688-2