Abstract
For recommendations of specific targets for the absolute amount of saturated fat intake, we need to know what dietary intake is most appropriate? Changing agricultural production and processing to lower the relative quantities of macronutrients requires years to accomplish. Changes can have unintended consequences on diets and the health of subsets of the population. Hence, what are the appropriate absolute amounts of saturated fat in our diets? Is the scientific evidence consistent with an optimal intake of zero? If not, is it also possible that a finite intake of saturated fats is beneficial to overall health, at least to a subset of the population? Conclusive evidence from prospective human trials is not available, hence other sources of information must be considered. One approach is to examine the evolution of lactation, and the composition of milks that developed through millennia of natural selective pressure and natural selection processes. Mammalian milks, including human milk, contain 50% of their total fatty acids as saturated fatty acids. The biochemical formation of a single double bond converting a saturated to a monounsaturated fatty acid is a pathway that exists in all eukaryotic organisms and is active within the mammary gland. In the face of selective pressure, mammary lipid synthesis in all mammals continues to release a significant content of saturated fatty acids into milk. Is it possible that evolution of the mammary gland reveals benefits to saturated fatty acids that current recommendations do not consider?
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diet, Fatty Acids, and Lipoproteins
Lipids and their simplest structural elements, the fatty acids, provide myriad functions at all levels of cellular life. Nutritional scientists are still wrestling to develop a rudimentary understanding of the roles that dietary lipids exert. Lipids as simple fats are the most concentrated energy source in the diet. Until recently, this fact alone made lipids a valuable food component; however, a global epidemic of caloric imbalance and obesity has undermined this one aspect of lipid nutrition. Nonetheless, dietary lipids are well recognized as providing the essential fatty acids and to dissolve and aid in the absorption of fat-soluble vitamins. Fats also produce a broad range of effects to whole body metabolism when consumed in foods. These effects, although not yet fully understood, are a complex consequence of the absolute and relative fat content, the fatty acid composition, the structure of other components in the foods, the timing of consumption and individual variations among those consuming them. Once ingested, lipids provide a diverse range of molecular functions and actions within cells and tissues beyond providing simple energy. Fatty acids are required for membrane synthesis, modifications of proteins and carbohydrates, construction of various structural elements in cells and tissues, production of signaling compounds and for oxidative fuel. The ability of lipids to associate spontaneously into multi-molecular structures of non-polar substituents provides a unique domain structure to biology (vesicles, globules, lipoproteins). These structures solubilize a variety of non-polar and poorly soluble cellular and extracellular constituents and transport such molecules within and between cells and tissues.
Given these various roles, why would saturated fats be so poorly thought of nutritionally? In one sense, saturated fats in the diet are unnecessary. All organisms, including humans, are fully capable of synthesizing saturated fatty acids. In the absence of sufficient dietary fat, the body is apparently capable of synthesizing all of the saturated fatty acids that it needs from the ubiquitous precursor building block acetate. This does not mean to infer that all saturated fatty acids are biologically indistinguishable. In fact, cells produce a remarkable diversity of saturated fatty acids under particular conditions, and although not all of their functions are known, they are clearly not simply interchangeable. Compositional analyses reveal remarkable specificities for particular saturated fatty acids in different lipid classes, cellular compartments and tissues [1]. Stubbs and Smith [2] reviewed studies aimed at understanding the requirement of membranes for specific fatty acid compositions. Interestingly, although composition is sensitive to polyunsaturated fatty acids, the content of saturated fatty acids in rat tissue membrane phospholipids is relatively constant at ~40% regardless of dietary fat source, indicating a control mechanism at some level. The de novo synthesis of saturated fatty acids is inhibited by feeding a high-fat diet [3], and membrane fragility resulting from feeding a low dietary saturated fatty acid diet is overcome by feeding a diet rich in fat [4].
The complexity of structure and the diversity of functions of fatty acids, both unsaturated and saturated, remain poorly understood, and in only a few biological situations have distinct actions of fatty acids been described. The majority of research on fatty acids consumed in the diet has focused principally on their role in lipoprotein metabolism. Authors of a recent meta-analysis of prospective studies on dairy food consumption and incident vascular disease and Type 2 diabetes concluded that it is not possible to estimate quantitative relationships with disease incidence with any confidence. The authors also point out that apart from the effects of dairy foods on plasma lipids and on blood pressure, very little is known about the biological mechanisms underlying such relationships [5]. Even for lipoprotein metabolism, for which literally billions of dollars have been invested in research, little is actually known. For example, only in 2005 was the basic mechanistic link between saturated fatty acids and cholesterol metabolism revealed [6]. This relationship between saturated fat in the diet and cholesterol metabolism was one of the most baffling scientific challenges of the twentieth century. How could such a ubiquitous, non-essential component of diets and tissues—saturated fat—cause an increase in the accumulation of cholesterol-rich LDL in blood? As scientific research on cholesterol metabolism proceeded through the twentieth century, the question became even more perplexing. Brown and Goldstein [7] won the Nobel prize for identifying the LDL receptor on the liver as being what controlled the concentration of serum cholesterol. What then regulates the expression of the LDL receptor on the surface of liver cells? Cellular cholesterol levels within the liver cell simultaneously control cholesterol synthesis and uptake by regulating the expression of the genes for the proteins that make cholesterol in the cell and for the proteins that take up cholesterol from blood as LDL. Not surprisingly, when cholesterol levels in the cell are adequate, the genes are not turned on. However, when cholesterol levels are low, all of these genes are turned on using the identical transcription factor protein—sterol response factor binding protein [8]. Although these studies made sense of cellular cholesterol regulation—if the cell needs more cholesterol, it simultaneously turns on the genes to make more via cholesterol biosynthetic enzymes and takes more from blood via the LDL receptor—they failed to explain the role of diet in these processes.
If the same transcription factor turns on both cholesterol biosynthesis and the LDL receptor, how can saturated fat uncouple these two processes, simultaneously making more cholesterol and yet shutting down the receptor? Puigserver and Spiegelman [9] found that the liver contains an additional gene control system, the peroxisome proliferator activating receptor (PPAR), and it is in turn controlled by a higher order protein complex termed (logically) the PPAR gene transcription coactivator (PGC-1). This transcription factor coactivator family recruits entire complexes of proteins into transcriptional regulatory units controlling such multi-faceted properties as mitochondrial biogenesis [10]. In a striking result, Lin et al. [6] discovered that, when exposed to high levels of saturated fatty acids, liver cells both in vivo and in vitro actively turned on PGC-1b, and even more astonishingly, this coactivator simultaneously turned on cholesterol biosynthesis and turned off the LDL receptor. Thus, in one bold study, the basic target linking dietary saturated fat and serum cholesterol was revealed. This mechanism would account for the tendency of diets very high in saturated fat to raise total cholesterol in blood. For some individuals, such a response could raise one of the risk factors for heart disease if they consumed diets high in saturated fat. An obvious question is what are the benefits to this biochemical response that would have caused it to be selected through evolution? Scientists are only now beginning to address the basic biological value of this regulatory control system. Nonetheless, diets very high in saturated fat would not seem prudent, as would any diet high in any food component.
Recommendations that the population decrease their intake of saturated fats was based not on a mechanistic understanding, but on years of observational evidence that dietary saturated fats generally increase blood cholesterol concentrations in animals and humans [11]. This alteration of risk factors does not necessarily lead to increases in heart disease and is certainly not universally true in all populations studied. Some studies of human populations evaluating the effects of saturated fat diets do not show the predicted elevation in heart disease; in fact, some studies see the reverse effect [12]. Recent studies are beginning to assign genetic or physiological explanations to these varying outcomes; for example, low birth weight appears to have an effect on subsequent responses to dietary fat [13]. Beare-Rogers [14] suggested that the saturated fatty acid requirements are also related to the stage of development. For example, saturated fatty acids appear to be essential for the newborn, the young and during rapid growth as they are required for the synthesis of membranes and lipoprotein.
Are Recommendations to Lower Total Fat Intakes Justified for Everyone?
Is the justification for broad recommendations to lower total fat intakes in all individuals supported by scientific evidence? In 1977, the US population was first recommended to reduce the intake of fat, with some recommendations being to reduce total fat to below 30% of calories [15]. The American Heart Association recommended that the percentage of calories be 28.6 and 25.3% total fat, respectively, and 9 and 6.1% saturated fat, respectively, in Step 1 and Step 2 diets for treatment of high blood cholesterol. This recommendation had unanticipated effects. Framingham Heart Study data showed that people with high triacylglycerol concentrations (>1.7 mmol/l) and low HDL cholesterol concentrations (<1.03 mmol/l) run a significantly higher risk of coronary artery disease [16]. The long-term health benefits of consuming a low-fat diet—particularly taking into account the variation in human responses—have not been proven and, to the contrary, some individuals move their risk profile, even for heart disease, in an adverse direction [17, 18]. In one study, healthy, non-diabetic volunteers consumed diets that contained, as a percentage of total calories, either 60% carbohydrate, 25% fat and 15% protein, or 40% carbohydrate, 45% fat and 15% protein [19]. Those consuming the 60% carbohydrate diet had higher fasting plasma triacylglycerol, remnant lipoprotein and remnant lipoprotein triacylglycerol, and lower HDL cholesterol without changing LDL cholesterol concentration. The low-fat diet lowered HDL cholesterol and caused a persistent elevation in remnant lipoproteins [19], both factors that are increasingly recognized to be important independent risk factors for heart disease and other metabolic diseases. These findings led the investigators to publish the question whether it is wise to recommend that all Americans replace dietary saturated fat with carbohydrate. It is important to point out that dietary carbohydrates have been associated with dyslipidemia [20], and lipoprotein risk factors are similar whether diets are high in fat and saturated fat or low in fat and high in sugar. Elevated triglyceride concentrations are related to increased hepatic secretion and impaired clearance of VLDL lipoprotein [21, 22]. Triglyceride response to dietary sugar may vary with the amount of sugar and the presence of other nutrients. Stanhope and Havel [23] reported that a high-fructose diet led to visceral adiposity, dyslipidemia and insulin resistance, and insulin resistance upregulates VLDL production. Perhaps the study most devastating to the basic principle that a lower fat diet improves the health of the entire population was a prospective study (The Women’s Health Initiative Randomized Controlled Dietary Modification Trial) that selected approximately 49,000 women to compare a group of women consuming low-fat diets and increased fruit and vegetable consumption with a group receiving only diet-related education materials. After 8.1 years, there were no statistical differences in heart disease outcomes [24]. Two possible interpretations could be drawn from this study: first, that lower fat intakes have no effect on any women, and second, that individuals vary in their response to fat and some women are benefitted and some are adversely affected and the net numbers of each are relatively close, leading to a conclusion in this trial of no effect of a low-fat diet.
Individual Response to Dietary Fat Intakes
Ordovas [25] reviewed key factors in lipid metabolism and obesity that indicate an interplay among genes, gender, and environmental factors that modulate disease susceptibility. Studies of response to dietary fats have found variation among individuals [26] and differences between men and women [27] in their response to dietary fat changes. Studies of individual sensitivity to changes in dietary saturated fats showed groups of consistent hyper-responders and minimal responders within a population of hypercholesterolaemic individuals [26]. Measurements of serum cholesterol in response to a decrease in dietary saturated fat showed that total cholesterol decreased to a greater extent in men than in women [27]. There are also differential responses in individuals that consume low-fat diets [28]. A series of studies showed that very-low-fat (10%), high-carbohydrate diets enriched in simple sugars increased the synthesis of fatty acids, especially palmitate, and that the individual differences in increased blood triglyceride concentrations varied considerably [29]. These fluctuations observed time after time have given impetus to the field of Nutrigenomics, and scientists are now pursuing more detailed analyses of individuals, their responses to diet and the mechanistic basis for variations in diet and health risk [30].
Controversy still remains high as to the roles that dietary fat and cholesterol play in the risk of heart disease, and the wealth of confounding factors demonstrate that saturated fat is not an overwhelming input variable for any population studied to date. Dietary saturated fats are not the only variables associated with heart disease—the causes are multi-factorial. The results of studies on the etiology of heart disease are inclusive and sometimes contradictory. It is time to take a broader view to the multiple actions and functions of each of the different saturated fats and a more individual view to assessment of diet and risk.
Biological Activities of Saturated Fatty Acids
The overwhelming emphasis on the role of saturated fats in the diet and risk of coronary heart disease has distracted investigators from studying other effects that individual saturated fatty acids may have in the body. This omission is perhaps important considering the abundance in mammalian milks of a wide range of saturated fatty acids with different chain lengths. In the context of evolution and the obvious natural selective pressure on the development of milk and all of its constituents, how do saturated fatty acids affect growth, development and survival of mammalian offspring?
Fatty acids are present in all body tissues, where they are a major part of the phospholipid component of the cell membrane. They contribute to the structural diversity within the membrane, which is now recognized to be a key aspect of membrane functions [31]. Fatty acids anchor proteins to particular regions of cell membranes, participate in signaling activities, transport cellular components and provide fuel. Saturated fatty acids have been suggested as being the preferred fuel for the heart [32]. In the absence of sufficient fat from the diet, the body synthesizes fatty acids, typically from carbohydrates. An interesting observation has been made that in adult rat liver, erucic acid (22:1)—a fatty acid that has been associated with heart disease and that is present in rapeseed oil—is rapidly converted to 18:0, demonstrating the conservation of carbons by chain-shortening of a monounsaturated fatty acid to an unsaturated fatty acid [33]. Even though all fatty acids present in the diet can be broken down and resynthesized into saturated fats, they have discrete effects. Different structures of fatty acids appear to have differing effects on a variety of metabolic and physiological processes when they are ingested.
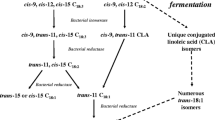
Short-chain fatty acids are hydrolyzed preferentially from triacylglycerols and absorbed from the intestine into the portal circulation without resynthesis of triacylglycerols. These fatty acids serve as a ready source of energy. Butyric acid (4:0) is the shortest saturated fatty acid and is present in ruminant milk fat at 2–5% by weight [34], which on a molar basis is about one-third the amount of palmitic acid (16:0). Human milk contains a lower percentage (ca. 0.4%) of butyric acid. No other common food fat contains this fatty acid directly; however, the consumption of a wide range of fermentable carbohydrates can lead to the synthesis of butyric acid by endogenous microflora in the lower intestine. Butyrate is a well-known modulator of genetic regulation, and its ability to promote differentiation has led various investigators to pursue this mechanism as a means to alter the risk and development of cancer [35, 36]. This fatty acid also lowers processes of inflammation in the intestine, acting through short-chain fatty acid-binding receptors [37].
In bovine and human milk, caproic acid (6:0) is present at ca. 1 and 0.1%, respectively, and caprylic acid (8:0) and capric acid (10:0) are present at ca. 0.3 and 1.2%, respectively, of the milk fat. Not surprisingly from its nomenclature, goat milk contains the highest percentage of caprylic acid, at 2.7% of milk fat. Studies to date have documented that these three fatty acids have similar biological activities when tested as antimicrobial agents. Caprylic acid lowers salmonella infection in chickens [38]. Caprylic and capric acid have antiviral activity. The monoglyceride form, monocaprin, has been shown in vivo in animals to possess antiviral activity against retrovirus infection [39].
Lauric acid (12:0) is present in human and bovine milk at ca. 5.8 and 2.2%, respectively, of the milk fat. Studies have shown antiviral and antibacterial activities of lauric acid [40, 41]. Release of lauric acid in the stomach may have direct antimicrobial activities towards Helicobacter pylori, either as the fatty acid or monoacylglycerols produced by lingual lipase(s) acting on the triacylglycerols present milk fat [42, 43]. These antibacterial actions of lauric acid have been proposed to provide anticaries and antiplaque activities [44]. The overall antimicrobial effects of the medium-chain saturated fatty acids and their monoacylglycerol derivatives on various microorganisms, including bacteria, yeast, fungi and enveloped viruses, were originally suggested to be acting through the lipid membranes of the organisms [45]. Support for this deactivation process has been shown using human and bovine milk [46]. Monolaurin released from milk lipids by lipases may account for milk’s anti-protozoal activities [47]. The biological activity of laurate has been interesting in other aspects not related to the diet. For example, a remarkable experiment showed that monolaurate provided considerable protection from HIV infection when used topically on reproductive tissues in primates [48].
Bovine milk fat contains 8–14% myristic acid (14:0) and in human milk, it averages 8.6% of the milk fat. Human epidemiological studies have shown that myristic acid and lauric acid were the saturated fatty acids most strongly related to the average serum cholesterol concentrations in humans [49]. Nonetheless, several studies have shown that myristic acid increases HDL cholesterol at least as much as LDL cholesterol, and further studies have demonstrated that the unique positional distribution of myristic acid in the sn-2 position of triglycerides in milk fat is responsible for its tendency to raise HDL [50].
Palmitic acid is present in human and bovine milk at 22.6 and 26.3%, yet almost exclusively esterified at the sn-2 position of the triglyceride. This unusual stereospecific distribution appears to have important nutritional and biological implications. Human infants consuming a formula containing triacylglycerides similar to those in human milk (16% palmitic acid esterified predominantly to the sn-2 position) have improved intestinal absorption not just of the palmitic acid but calcium as well [51, 52]. Recently, Speigelman’s group showed that palmitic acid stimulated the expression and activities of the transcription coactivator PGC-1b and by so doing promoted the transcriptional regulation of biosynthesis of lipoproteins from the liver [6]. This finding places a mechanistic understanding of the cellular actions of saturated fatty acids, particularly palmitic acid. In the context of milk, this mechanism implies that palmitic acid may have an important role in promoting successful lipoprotein metabolism in infants. This same transcription coactivator PGC-1b was also found to promote myocardial development [53]. Finally, PGC-1b was shown to increase biogenesis of mitochondria in neurons [54], further implying that this mechanism could well be involved in diverse aspects of metabolic regulation and its saturated fatty acid-appropriate development throughout the body in infants. It is not known if the presence of palmitic acid in human milk is important in the coordinate regulation and activity of PGC-1b in any of these activities.
Stearic acid (18:0) is an abundant fatty acid in milk, present in human and bovine milk fat at 7.7 and 13.2% of fat, respectively. Stearic acid is synthesized from palmitate via the elongase enzyme, either in the mammary gland by the same enzyme that is active in liver, coded by gene ELOV5 [55, 56], or by ELOV1, whose expression is induced in the mammary gland during lactation [57, 58]. Both of these genes are regulated by diet, hence the net production of stearic acid is under various aspects of metabolic control. Surprisingly, little research has pursued the specific actions of stearic acid when consumed in milk by infants, in spite of its abundance and obvious regulation within the mammary gland during fat synthesis. In adults, stearic acid does not appear to raise serum cholesterol, hence it is considered neutral to heart disease risk. This fatty acid may exert other effects also consistent with protection from heart disease via separate mechanisms. Healthy males who consumed dietary stearic acid (19 g/d) for 4 weeks exhibited beneficial effects on thrombogenic and atherogenic risk factors as compared with the effects of dietary palmitic acid [59].
Delivery of Fat-Soluble Nutrients
Fat-soluble nutrients include the essential nutrients vitamins A, D, E and K, carotenoids as vitamin A precursors, essential polyunsaturated fatty acids, and non-essential nutrients such as various tocopherols, phenolics, carotenoids (e.g., lycopene, lutein and zeaxanthin) and conjugated linoleic acid isomers that cannot be made by humans. Fat-soluble nutrients are increasingly recognized as pleotrophic nutrients with several discrete actions in addition to the direct functions for which their essentiality has been established. As a result, consumption of these components is considered to have biological activities beyond the simple prevention of deficiency and is consistent with many aspects of health [60–62]. In epidemiological studies, the abundance of fat-soluble nutrients in tissues is frequently reported to be inversely correlated with a variety of chronic and degenerative diseases, including cancers [63, 64], cardiovascular diseases [65, 66], diabetes [67] and specific tissue degeneration such as macular degeneration [68] [58, 59]. With the recognition that there are potential health values associated with the presence of fat-soluble nutrients in tissues, their absorption from the diet has become a key issue. In general, non-polar molecules are poorly absorbed, and it is not certain that the presence of a component in a food means that it will be absorbed and delivered to particular tissues in which it might be active [69]. The lipid-soluble components of milk appear to be well absorbed into and accumulated in tissues, although the basic mechanisms by which such a net delivery is accomplished are not known [70, 71].
Milkfat and HDL
Breast feeding stimulates the production of serum lipids and lipoproteins [72, 73]. Interestingly, this increase in serum lipids in infancy is reversed in adulthood [74]. Nonetheless, throughout life, when compared with either carbohydrates or polyunsaturated fatty acids, the consumption of bovine milk fat results in the elevation of circulating HDL cholesterol. Decades of research have documented that blood HDL cholesterol concentrations are a very strong and independent predictor of heart disease [75]. This relationship has not been as successfully exploited therapeutically as lowering LDL, however, because HDL concentrations are not as responsive to diet and drugs as those of LDL. A major pharmacologic effort has pursued an increase in HDL cholesterol concentrations in humans as a means to reduce cardiovascular risk. This research is based on the extensive evidence of the associations of high HDL with protection from heart disease, even in the face of elevated LDL. There is also evidence of an opposite relationship, that low HDL is associated with increased risk, with or without elevated triglycerides. However, it has not been possible to assign independent variables to HDL differences, and studies have largely been based on HDL concentrations that are presumably high or low based on genetic rather than dietary determinants [76, 77].
HDL exert beneficial effects on overall health by myriad mechanisms, including binding and eliminating toxins, delivering bioactive compounds, protecting various cells and lipoproteins from damage and participating in their repair [78–80]. HDL is particularly important in the successful response to infection by binding and clearing bacterial endotoxin or lipopolysaccharide (LPS). LPS is the major glycolipid component of gram-negative bacterial outer membranes and is responsible for pathophysiological symptoms characteristic of infection. A wide variety of studies have documented that LPS is associated with plasma lipoproteins, suggesting that sequestering of LPS by lipid particles may form an integral part of a humoral detoxification mechanism [81, 82]. The binding of LPS to lipoproteins is highly specific under simulated physiological conditions, and HDL has the highest binding capacity for LPS [83, 84]. This basic protection mechanism may be particularly important for children [85] and for intestinally derived endotoxin. Thus, lipoprotein-binding protein–lipoprotein complexes may be part of a local defense mechanism of the intestine against translocated bacterial toxin. Because milk fats enhance HDL concentrations, they are of potential importance in protection against bacterial LPS toxicity.
Conclusions
The genes and biochemical processes of lactation that produce milk fat evolved under the constant selective pressure of nourishing mammalian infants. Lipids in milk are a source of energy for the neonate of each species. The composition and structures of lipids in milk provide bioactive components that, although not identified as “essential” nutrients by standard definitions, none-the-less serve important functions as structural building blocks, fuels, transport systems, anti-inflammatory, anti-bacterial and antiviral agents in the intestine. These lipids include triacylglycerols—which are metabolized to monoacyl- and diacylcerides and fatty acids—and phospholipids such as sphingomyelin. The lipids in milk are also carriers of important fat-soluble vitamins such as vitamin E, vitamin A and vitamin D.
The absolute quantities and proportionate balance of the various macronutrients in human diets remains the subject of both scientific research and public health speculation. Although unquestionably evolved to nourish infants, detailed examinations of milk and lactation in humans and other mammals are revealing new insights into structures and functions of different components in the diet, including fat. The gene set responsible for the production of lipids is a conspicuously retained subset of the genome throughout mammalian lactation, implying that milk is, in many respects, a lipid delivery system [86]. Saturated fatty acids are a significant component of all mammalian milks examined, including human milk. Thus, whereas diets inordinately high in any component are likely to be net deleterious, finite quantities of saturated fatty acids may provide distinct mechanistic benefits to various metabolic processes. Recognizing that different humans with different lifestyles respond differently to fat intakes and compositions implies that in the future, diets will be designed for individuals not populations. In such a future, finite intakes of specific saturated fats may actually be recommended.
Abbreviations
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- PPAR:
-
Peroxisome proliferator activated receptor
- PGC-1:
-
PPAR gene transcription coactivator
- LPS:
-
Lipopolysaccharide
References
Watkins SM, Reifsnyder PR, Pan HJ, German JB, Leiter EH (2002) Lipid metabolome-wide effects of the PPARgamma agonist rosiglitazone. J Lipid Res 43:1809–1817
Stubbs CD, Smith AD (1984) The modification of mammalian membrane polyunsaturated fatty acid composition in relation to membrane fluidity and function. Biochim Biophys Acta 779:89–137
Iritani N, Fukuda E (1980) Effect of corn oil feeding on triglyceride synthesis in the rat. J Nutr 110:1138–1143
Kramer JK, Farnworth ER, Thompson BK, Corner AH, Trenholm HL (1982) Reduction of myocardial necrosis in male albino rats by manipulation of dietary fatty acid levels. Lipids 17:372–382
Elwood PC, Pickering JE, Givens DI, Gallacher JE (2010) The consumption of milk and dairy foods and the incidence of vascular disease and diabetes: an overview of the evidence. Lipids. doi:10.1007/s11745-010-3412-5
Lin J, Yang R, Tarr PT, Wu PH, Handschin C, Li S, Yang W, Pei L, Uldry M, Tontonoz P, Newgard CB, Spiegelman BM (2005) Hyperlipidemic effects of dietary saturated fats mediated through PGC-1beta coactivation of SREBP. Cell 120:261–273
Brown MS, Goldstein JL (1986) A receptor-mediated pathway for cholesterol homeostasis. Science 232:34–47
Brown MS, Goldstein JL (1997) The SREBP pathway: regulation of cholesterol metabolism by proteolysis of a membrane-bound transcription factor. Cell 89:331–340
Puigserver P, Spiegelman BM (2003) Peroxisome proliferator-activated receptor-gamma coactivator 1 alpha (PGC-1 alpha): transcriptional coactivator and metabolic regulator. Endocr Rev 24:78–90
Wu Z, Puigserver P, Andersson U, Zhang C, Adelmant G, Mootha V, Troy A, Cinti S, Lowell B, Scarpulla RC, Spiegelman BM (1999) Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC-1. Cell 98:115–124
Food and Nutrition Board (2002) Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids (Macronutrients). National Academies Press, Washington, DC
Mozaffarian D, Rimm EB, Herrington DM (2004) Dietary fats, carbohydrate, and progression of coronary atherosclerosis in postmenopausal women. Am J Clin Nutr 80:1175–1184
Robinson SM, Batelaan SF, Syddall HE, Sayer AA, Dennison EM, Martin HJ, Barker DJ, Cooper C, Hertfordshire Cohort Study (2006) Combined effects of dietary fat and birth weight on serum cholesterol concentrations: the Hertfordshire Cohort Study. Am J Clin Nutr 84:237–244
Beare-Rogers JL (1998) Dietary fatty acids, where are we going? J Food Lipids 5:135–140
US Senate Select Committee on Nutrition and Human Needs (1977) Dietary goals for the United States, 2nd edn. US Government Printing Office, Washington, DC
Castelli WP (1992) Epidemiology of triglycerides: a view from Framingham. Am J Cardiol 70:3H–9H
Dreon DM, Fernstrom HA, Miller B, Krauss RM (1994) Low-density lipoprotein subclass patterns and lipoprotein response to a reduced-fat diet in men. FASEB J 8:121–126
Krauss RM, Dreon DM (1995) Low-density-lipoprotein subclasses and response to a low-fat diet in healthy men. Am J Clin Nutr 62:478S–487S
Abbasi F, McLaughlin T, Lamendola C, Kim HS, Tanaka A, Wang T, Nakajima K, Reaven GM (2000) High carbohydrate diets, triglyceride-rich lipoproteins, and coronary heart disease risk. Am J Cardiol 85:45–48
Welsh JA, Sharma A, Abramson JL, Vaccarino V, Gillespie C, Vos MB (2010) Caloric sweetener consumption and dyslipidemia among US adults. JAMA 303:1490–1497
Frayn KN, Kingman SM (1995) Dietary sugars and lipid metabolism in humans. Am J Clin Nutr 62:250S–261S (discussion 261S–263S)
Parks EJ, Hellerstein MK (2000) Carbohydrate-induced hypertriacylglycerolemia: historical perspective and review of biological mechanisms. Am J Clin Nutr 71:412–433
Stanhope KL, Havel PJ (2008) Fructose consumption: potential mechanisms for its effects to increase visceral adiposity and induce dyslipidemia and insulin resistance. Curr Opin Lipidol 19:16–24
Howard BV, Van Horn L, Hsia J, Manson JE, Stefanick ML et al (2006) Low-fat dietary pattern and risk of cardiovascular disease: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA 295:655–666
Ordovas JM (2007) Gender, a significant factor in the cross talk between genes, environment, and health. Gend Med 4(Suppl B):S111–S122
Cox C, Mann J, Sutherland W, Ball M (1995) Individual variation in plasma cholesterol response to dietary saturated fat. BMJ 311:1260–1264
Weggemans R, Zock P, Urgert R, Katan M (1999) Differences between men and women in the response of serum cholesterol to dietary changes. Eur J Clin Invest 29:827–834
Asztalos B, Lefevre M, Wong L, Foster T, Tulley R, Windhauser M, Zhang W, Roheim PS (2000) Differential response to low-fat diet between low and normal HDL-cholesterol subjects. J Lipid Res 41:321–328
Hudgins LC (2000) Effect of high-carbohydrate feeding on triglyceride and saturated fatty acid synthesis. Proc Soc Exp Biol Med 225:178–183
Ordovas JM (2004) The quest for cardiovascular health in the genomic era: nutrigenetics and plasma lipoproteins. Proc Nutr Soc 63:145–152
Fielding CJ (2004) Lipid rafts and caveolae: from membrane biophysics to cell biology. Wiley-VCH, Weinheim
Lawson L, Kummerow F (1979) [beta]-Oxidation of the coenzyme a esters of elaidic, oleic, and stearic acids and their full-cycle intermediates by rat heart mitochondria. Biochim Biophys Acta 573:245–254
Murphy CC, Murphy EJ, Golovko MY (2008) Erucic acid is differentially taken up and metabolized in rat liver and heart. Lipids 43:391–400
Smith J, German J (1995) Molecular and genetic effects of dietary derived butyric acid. Food Tech 49:87–90
Smith JG, Yokoyama WH, German JB (1998) Butyric acid from the diet: actions at the level of gene expression. Crit Rev Food Sci Nutr 38:259–297
Young GP, Hu Y, Le Leu RK, Nyskohus L (2005) Dietary fibre and colorectal cancer: a model for environment–gene interactions. Mol Nutr Food Res 49:571–584
Maslowski KM, Vieira AT, Ng A, Kranich J, Sierro F, Yu D, Schilter HC, Rolph MS, Mackay F, Artis D, Xavier RJ, Teixeira MM, Mackay CR (2009) Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature 461:1282–1286
Johny A, Baskaran S, Charles A, Amalaradjou M, Darre M, Khan MI, Hoagland TA, Schreiber DT, Donoghue AM, Donoghue DJ (2009) Prophylactic supplementation of caprylic acid in feed reduces Salmonella enteritidis colonization in commercial broiler chicks. J Food Prot 72:722–727
Neyts J, Kristmundsdottir T, De Clercq E, Thormar H (2000) Hydrogels containing monocaprin prevent intravaginal and intracutaneous infections with HSV-2 in mice: impact on the search for vaginal microbicides. J Med Virol 61:107–110
Hornung B, Amtmann E, Sauer G (1994) Lauric acid inhibits the maturation of vesicular stomatitis virus. J Gen Virol 75:353–361
Batovska D, Todorova I, Tsvetkova I, Najdenski H (2009) Antibacterial study of the medium chain fatty acids and their 1-monoglycerides: individual effects and synergistic relationships. Pol J Microbiol 58:43–47
Sun CQ, O’Connor CJ, Roberton AM (2003) Antibacterial action of fatty acids and monoglycerides against Helicobacter pylori. FEMS Immunol Med Microbiol 36:9–17
Sun CQ, O’Connor CJ, Roberton AM (2002) The antimicrobial properties of milkfat after partial hydrolysis by calf pregastric lipase. Chem Biol Interact 140:185–198
Schuster GS, Dirksen TR, Ciarlone AE, Burnett GW, Reynolds MT, Lankford MT (1980) Anticaries and antiplaque potential of free-fatty acids in vitro and in vivo. Pharmacol Ther Dent 5:25–33
Thormar H, Isaacs C, Brown H, Barshatzky M, Pessolano T (1987) Inactivation of enveloped viruses and killing of cells by fatty acids and monoglycerides. Antimicrob Agents Chemother 31:27–31
Isaacs CE, Litov RE, Thormar H (1995) Antimicrobial activity of lipids added to human milk, infant formula, and bovine milk. J Nutr Biochem 6:362–366
Reiner DS, Wang CS, Gillin FD (1986) Human milk kills Giardia lamblia by generating toxic lipolytic products. J Infect Dis 154:825–832
Li Q, Estes JD, Schlievert PM, Duan L, Brosnahan AJ, Southern PJ, Reilly CS, Peterson ML, Schultz-Darken N, Brunner KG, Nephew KR, Pambuccian S, Lifson JD, Carlis JV, Haase AT (2009) Glycerol monolaurate prevents mucosal SIV transmission. Nature 458:1034–1038
Kromhout D, Menotti A, Bloemberg B, Aravanis C, Blackburn H, Buzina R, Dontas AS, Fidanza F, Giampaoli S, Jansen A, Martti K, Martijn K, Aulikki N, Srecko N, Juha P, Maija P, Sven P, Leena R, Bozidar S, Hironori T (1995) Dietary saturated and transfatty acids and cholesterol and 25-year mortality from coronary heart disease: the seven countries study. Prev Med 24:308–315
Dabadie H, Peuchant E, Bernard M, LeRuyet P, Mendy F (2005) Moderate intake of myristic acid in sn-2 position has beneficial lipidic effects and enhances DHA of cholesteryl esters in an interventional study. J Nutr Biochem 16:375–382
Carnielli VP, Luijendijk IH, van Goudoever JB, Sulkers EJ, Boerlage AA, Degenhart HJ, Sauer PJ (1995) Feeding premature newborn infants palmitic acid in amounts and stereoisomeric position similar to that of human milk: effects on fat and mineral balance. Am J Clin Nutr 61:1037–1042
Carnielli VP, Luijendijk IH, Van Goudoever JB, Sulkers EJ, Boerlage AA, Degenhart HJ, Sauer PJ (1996) Structural position and amount of palmitic acid in infant formulas: effects on fat, fatty acid, and mineral balance. J Pediatr Gastroenterol Nutr 23:553–560
Lai L, Leone TC, Zechner C, Schaeffer PJ, Kelly SM, Flanagan DP, Medeiros DM, Kovacs A, Kelly DP (2008) Transcriptional coactivators PGC-1alpha and PGC-lbeta control overlapping programs required for perinatal maturation of the heart. Genes Dev 22:1948–1961
Wareski P, Vaarmann A, Choubey V, Safiulina D, Liiv J, Kuum M, Kaasik A (2009) PGC-1 and PGC-1 regulate mitochondrial density in neurons. J Biol Chem 284:21379–21385
Moon YA, Shah NA, Mohapatra S, Warrington JA, Horton JD (2001) Identification of a mammalian long chain fatty acyl elongase regulated by sterol regulatory element-binding proteins. J Biol Chem 276:45358–45366
Moon Y, Hammer R, Horton J (2009) Deletion of ELOVL5 leads to fatty liver through activation of SREBP-1c in mice. J Lipid Res 50:412–423
Rudolph MC, Neville MC, Anderson SM (2007) Lipid synthesis in lactation: diet and the fatty acid switch. J Mammary Gland Biol Neoplasia 12:269–281
Russell TD, Palmer CA, Orlicky DJ, Fischer A, Rudolph MC, Neville MC, McManaman JL (2007) Cytoplasmic lipid droplet accumulation in developing mammary epithelial cells: roles of adipophilin and lipid metabolism. J Lipid Res 48:1463–1475
Kelly FD, Sinclair AJ, Mann NJ, Turner AH, Abedin L, Li D (2001) A stearic acid-rich diet improves thrombogenic and atherogenic risk factor profiles in healthy males. Eur J Clin Nutr 55:88–96
Giovannucci E, Ascherio A, Rimm E, Stampfer M, Colditz G, Walter C, Willett WC (1995) Intake of carotenoids and retinol in relation to risk of prostate cancer. J Nat Cancer Inst 87:1767–1776
Traber MG, Packer L (1995) Vitamin E: beyond antioxidant function. Am J Clin Nutr 62:1501S–1509S
Dietrich M, Traber MG, Jacques PF, Cross CE, Hu Y, Block G (2006) Does gamma-tocopherol play a role in the primary prevention of heart disease and cancer? A review. J Am Coll Nutr 25:292–299
Zhu Z, Parviainen M, Männistö S, Pietinen P, Eskelinen M, Syrjänen K, Uusitupa M (1996) Vitamin E concentration in breast adipose tissue of breast cancer patients (Kuopio, Finland). Cancer Causes Control 7:591–595
Ahmed M, Fayed S, Hossein H, Tash F (1999) Lipid peroxidation and antioxidant status in human cervical carcinoma. Dis Markers 15:283–291
Palace VP, Khaper N, Qin Q, Singal PK (1999) Antioxidant potentials of vitamin A and carotenoids and their relevance to heart disease. Free Radic Biol Med 26:746–761
Palace VP, Hill MF, Khaper N, Singal PK (1999) Metabolism of vitamin A in the heart increases after a myocardial infarction. Free Radic Biol Med 26:1501–1507
Haffner SM (2000) Coronary heart disease in patients with diabetes. N Engl J Med 342:1040–1042
Belda JI, Roma J, Vilela C, Puertas FJ, Diaz-Llopis M, Bosch-Morell F, Romero FJ (1999) Serum vitamin E levels negatively correlate with severity of age-related macular degeneration. Mech Ageing Dev 107:159–164
Papas AM (1996) Determinants of antioxidant status in humans. Lipids 31(Suppl):S77–S82
Jeanes YM, Hall WL, Ellard S, Lee E, Lodge JK (2004) The absorption of vitamin E is influenced by the amount of fat in a meal and the food matrix. Br J Nutr 92:575–579
Lodge JK, Hall WL, Jeanes YM, Proteggente AR (2004) Physiological factors influencing vitamin E biokinetics. Ann N Y Acad Sci 1031:60–73
Harit D, Faridi MM, Aggarwal A, Sharma SB (2008) Lipid profile of term infants on exclusive breastfeeding and mixed feeding: a comparative study. Eur J Clin Nutr 62:203–209
Fujita H, Okada T, Inami I, Makimoto M, Hosono S, Minato M, Takahashi S, Mugishima H, Yamamoto T (2008) Low-density lipoprotein profile changes during the neonatal period. J Perinatol 28:335–340
Owen CG, Whincup PH, Odoki K, Gilg JA, Cook DG (2002) Infant feeding and blood cholesterol: a study in adolescents and a systematic review. Pediatrics 110:597–608
Chapman MJ (2006) Therapeutic elevation of HDL-cholesterol to prevent atherosclerosis and coronary heart disease. Pharmacol Ther 111:893–908
Wang N, Lan D, Chen W, Matsuura F, Tall AR (2004) ATP-binding cassette transporters G1 and G4 mediate cellular cholesterol efflux to high-density lipoproteins. Proc Natl Acad Sci USA 101:9774–9779
Wang X, Paigen B (2005) Genetics of variation in HDL cholesterol in humans and mice. Circ Res 96:27–42
Argraves KM, Argraves WS (2007) HDL serves as a S1P signaling platform mediating a multitude of cardiovascular effects. J Lipid Res 48:2325–2333
Rader DJ (2006) Molecular regulation of HDL metabolism and function: implications for novel therapies. J Clin Invest 116:3090–3100
Canturk NZ, Canturk Z, Okay E, Yirmibesoglu O, Eraldemir B (2002) Risk of nosocomial infections and effects of total cholesterol, HDL cholesterol in surgical patients. Clin Nutr 21:431–436
Feingold KR, Funk JL, Moser AH, Shigenaga JK, Rapp JH, Grunfeld C (1995) Role for circulating lipoproteins in protection from endotoxin toxicity. Infect Immun 63:2041–2046
Pajkrt D, Doran JE, Koster F, Lerch PG, Arnet B, van der Poll T, ten Cate JW, van Deventer SJ (1996) Antiinflammatory effects of reconstituted high-density lipoprotein during human endotoxemia. J Exp Med 184:1601–1608
van Leeuwen HJ, van Beek AP, Dallinga-Thie GM, van Strijp JA, Verhoef J, van Kessel KP (2001) The role of high density lipoprotein in sepsis. Neth J Med 59:102–110
Levels JH, Abraham PR, van den Ende A, van Deventer SJ (2001) Distribution and kinetics of lipoprotein-bound endotoxin. Infect Immun 69:2821–2828
Liuba P, Persson J, Luoma J, Yla-Herttuala S, Pesonen E (2003) Acute infections in children are accompanied by oxidative modification of LDL and decrease of HDL cholesterol, and are followed by thickening of carotid intima-media. Eur Heart J 24:515–521
Lemay DG, Lynn DJ, Martin WF, Casey TM, Kriventseva EV, Rincon G, Barris WC, Hinrichs AS, Molenaar AJ, Pollard KS, Neville MC, Maqbool NJ, Zdobnov EM, Tellam RL, Medrano JF, German JB, Rijnkels M (2009) The bovine lactation genome: insights into the evolution of mammalian milk. Genome Biol 10:R43
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
German, J.B., Dillard, C.J. Saturated Fats: A Perspective from Lactation and Milk Composition. Lipids 45, 915–923 (2010). https://doi.org/10.1007/s11745-010-3445-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11745-010-3445-9