Abstract
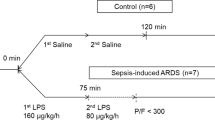
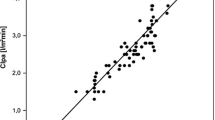
Pulmonary edema and its association with low flow times has been observed in postcardiac arrest patients. However, diagnosis of distinct types of lung pathology is difficult.The aim of this study was to investigate pulmonary edema by transpulmonary thermodilution (TPTD) after out-of-hospital cardiac arrest (OHCA), and the correlation to downtimes. In this retrospective single-center study consecutive patients with return of spontaneous circulation (ROSC) following OHCA, age ≥ 18, and applied TPTD were enrolled. According to downtimes, patients were divided into a short and a long no-flow-time group, and data of TPTD were analysed. We identified 45 patients (n = 25 short no-flow time; n = 20 long no-flow time) who met the inclusion criteria. 24 h after ROSC, the extra vascular lung water index (EVLWI) was found to be lower in the group with short no-flow time compared to the group with long no-flow time (10.7 ± 3.5 ml/kg vs. 12.8 ± 3.9 ml/kg; p = 0.08) and remained at a similar level 48 h (10.9 ± 4.3 ml/kg vs. 12.9 ± 4.9 ml/kg; p = 0.25) and 72 h (11.1 ± 5.0 ml/kg vs. 13.9 ± 7.7 ml/kg; p = 0.27) post-ROSC. We found a statistically significant and moderate correlation between no-flow duration and EVLWI 48 h (r = 0.51; p = 0.002) and 72 h (r = 0.54; p = 0.004) post-ROSC. Pulmonary vascular permeability index (PVPI) was not correlated with downtimes. Our observation underlines the presence of cardiac arrest-related lung edema by determination of EVLWI. The duration of no-flow times is a relevant factor for increased extravascular lung water index.


Similar content being viewed by others
Data availability
Data will be available for reasonable requests.
References
Benjamin EJ, Muntner P, Alonso A et al (2019) Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation 139:e56–e528. https://doi.org/10.1161/CIR.0000000000000659
Gräsner J-T, Wnent J, Herlitz J et al (2020) Survival after out-of-hospital cardiac arrest in Europe—results of the EuReCa TWO study. Resuscitation 148:218–226. https://doi.org/10.1016/j.resuscitation.2019.12.042
Nolan JP, Sandroni C, Böttiger BW et al (2021) European Resuscitation Council and European Society of Intensive Care Medicine Guidelines 2021: post-resuscitation care. Resuscitation 161:220–269. https://doi.org/10.1016/j.resuscitation.2021.02.012
Mongardon N, Dumas F, Ricome S et al (2011) Postcardiac arrest syndrome: from immediate resuscitation to long-term outcome. Ann Intensive Care 1:45. https://doi.org/10.1186/2110-5820-1-45
Dohi S (1983) Postcardiopulmonary resuscitation pulmonary edema. Crit Care Med 11:434–437. https://doi.org/10.1097/00003246-198306000-00008
Johnson NJ, Caldwell E, Carlbom DJ et al (2019) The acute respiratory distress syndrome after out-of-hospital cardiac arrest: Incidence, risk factors, and outcomes. Resuscitation 135:37–44. https://doi.org/10.1016/j.resuscitation.2019.01.009
Adrie C, Laurent I, Monchi M et al (2004) Postresuscitation disease after cardiac arrest: a sepsis-like syndrome? Curr Opin Crit Care 10:208–212. https://doi.org/10.1097/01.ccx.0000126090.06275.fe
Yao Y, Johnson NJ, Perman SM et al (2018) Myocardial dysfunction after out-of-hospital cardiac arrest: predictors and prognostic implications. Intern Emerg Med 13:765–772. https://doi.org/10.1007/s11739-017-1756-z
Jentzer JC, Anavekar NS, Mankad SV et al (2018) Echocardiographic left ventricular diastolic dysfunction predicts hospital mortality after out-of-hospital cardiac arrest. J Crit Care 47:114–120. https://doi.org/10.1016/j.jcrc.2018.06.016
Schick A, Prekker ME, Kempainen RR et al (2022) Association of hypoxic ischemic brain injury on early CT after out of hospital cardiac arrest with neurologic outcome. Am J Emerg Med 54:257–262. https://doi.org/10.1016/j.ajem.2022.02.003
Liu Z, Liu Q, Wu G et al (2018) Quantitative CT assessment of lung injury after successful cardiopulmonary resuscitation in a porcine cardiac arrest model of different downtimes. Quant Imaging Med Surg 8:946–956. https://doi.org/10.21037/qims.2018.10.04
Shih JA, Robertson HK, Issa MS et al (2022) Acute respiratory distress syndrome after in-hospital cardiac arrest. Resuscitation 177:78–84. https://doi.org/10.1016/j.resuscitation.2022.05.006
Magliocca A, Rezoagli E, Zani D et al (2021) Cardiopulmonary resuscitation-associated lung edema (CRALE). A translational study. Am J Respir Crit Care Med 203:447–457. https://doi.org/10.1164/rccm.201912-2454OC
Kang D-H, Kim J, Rhee JE et al (2015) The risk factors and prognostic implication of acute pulmonary edema in resuscitated cardiac arrest patients. Clin Exp Emerg Med 2:110–116. https://doi.org/10.15441/ceem.14.016
Kim J, Kim T, Kim K et al (2013) Risk factors and prognostic implication of acute pulmonary edema in resuscitated out-of-hospital cardiac arrest patients. Resuscitation 84:S78. https://doi.org/10.1016/j.resuscitation.2013.08.199
Johnson NJ, Town JA (2022) Don’t go breaking my…lungs? The acute respiratory distress syndrome is common, deadly, and probably underrecognized after cardiac arrest. Resuscitation 177:1–2. https://doi.org/10.1016/j.resuscitation.2022.06.002
Ar P, Ja B, Jg C et al (2020) Part 3: adult basic and advanced life support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. https://doi.org/10.1161/CIR.0000000000000916
Snashall PD, Keyes SJ, Morgan BM et al (1981) The radiographic detection of acute pulmonary oedema. A comparison of radiographic appearances, densitometry and lung water in dogs. Br J Radiol 54:277–288. https://doi.org/10.1259/0007-1285-54-640-277
Zeeuw van der Laan EAN, van der Velden S, Porcelijn L et al (2020) Update on the pathophysiology of transfusion-related acute lung injury. Curr Opin Hematol 27:386–391. https://doi.org/10.1097/MOH.0000000000000607
Jozwiak M, Teboul J-L, Monnet X (2015) Extravascular lung water in critical care: recent advances and clinical applications. Ann Intensive Care 5:38. https://doi.org/10.1186/s13613-015-0081-9
Cecconi M, De Backer D, Antonelli M et al (2014) Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med 40:1795–1815. https://doi.org/10.1007/s00134-014-3525-z
Fischer M, Wnennt J, Gräsner J-T et al (2021) Öffentlicher Jahresbericht 2021 des Deutschen Reanimationsregisters: Außerklinische Reanimation
Yang Z, Zheng H, Lin L et al (2019) Alterations in respiratory mechanics and neural respiratory drive after restoration of spontaneous circulation in a porcine model subjected to different downtimes of cardiac arrest. J Am Heart Assoc. https://doi.org/10.1161/JAHA.119.012441
Bhattacharjee A, Pradhan D, Bhattacharyya P et al (2017) How useful is extravascular lung water measurement in managing lung injury in intensive care unit? Indian J Crit Care Med Peer-Rev 21:494. https://doi.org/10.4103/ijccm.IJCCM_40_17
Rasch S, Schmidle P, Sancak S et al (2021) Increased extravascular lung water index (EVLWI) reflects rapid non-cardiogenic oedema and mortality in COVID-19 associated ARDS. Sci Rep 11:11524. https://doi.org/10.1038/s41598-021-91043-3
Oksanen T, Skrifvars M, Wilkman E et al (2014) Postresuscitation hemodynamics during therapeutic hypothermia after out-of-hospital cardiac arrest with ventricular fibrillation: a retrospective study. Resuscitation 85:1018–1024. https://doi.org/10.1016/j.resuscitation.2014.04.026
Geri G, Richard J-C (2021) Cardiopulmonary resuscitation–associated lung edema: the price to pay to get the heartbeat? Am J Respir Crit Care Med 203:405–406. https://doi.org/10.1164/rccm.202009-3445ED
Saugel B, Wildgruber M, Staudt A et al (2019) Quantitative computed tomography in comparison with transpulmonary thermodilution for the estimation of pulmonary fluid status: a clinical study in critically ill patients. J Clin Monit Comput. https://doi.org/10.1007/s10877-018-0144-1
Saugel B, Holzapfel K, Stollfuss J et al (2011) Computed tomography to estimate cardiac preload and extravascular lung water. A retrospective analysis in critically ill patients. Scand J Trauma Resusc Emerg Med 19:31. https://doi.org/10.1186/1757-7241-19-31
Bro-Jeppesen J, Kjaergaard J, Wanscher M et al (2015) Systemic inflammatory response and potential prognostic implications after out-of-hospital cardiac arrest: a substudy of the target temperature management trial. Crit Care Med 43:1223–1232. https://doi.org/10.1097/CCM.0000000000000937
Langeland H, Damås JK, Mollnes TE et al (2022) The inflammatory response is related to circulatory failure after out-of-hospital cardiac arrest: a prospective cohort study. Resuscitation 170:115–125. https://doi.org/10.1016/j.resuscitation.2021.11.026
Bro-Jeppesen J, Kjaergaard J, Wanscher M et al (2014) The inflammatory response after out-of-hospital cardiac arrest is not modified by targeted temperature management at 33 °C or 36 °C. Resuscitation 85:1480–1487. https://doi.org/10.1016/j.resuscitation.2014.08.007
Braunstein M, Williamson M, Kusmenkov T et al (2017) Significant cytokine mRNA expression changes immediately after initiation of cardiopulmonary resuscitation. Mediat Inflamm 2017:1–10. https://doi.org/10.1155/2017/8473171
Park Y, Tae H-J, Cho JH et al (2018) The relationship between low survival and acute increase of tumor necrosis factor α expression in the lung in a rat model of asphyxial cardiac arrest. Anat Cell Biol 51:128–135. https://doi.org/10.5115/acb.2018.51.2.128
Kovács E, Pilecky D, Becker D et al (2012) Hemodynamic changes and invasive hemodynamic monitoring during post-resuscitation therapeutic hypothermia (preliminary data). Resuscitation 83:e96–e97. https://doi.org/10.1016/j.resuscitation.2012.08.250
Kovács E, Gyarmathy VA, Pilecky D et al (2021) An interaction effect analysis of thermodilution-guided hemodynamic optimization, patient condition, and mortality after successful cardiopulmonary resuscitation. Int J Environ Res Public Health 18:5223. https://doi.org/10.3390/ijerph18105223
Author information
Authors and Affiliations
Contributions
IV conceptualization, methodology, investigation, writing—original draft, writing—review and editing, visualization. MM investigation, writing—review and editing. HW, OB writing—review and editing, supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Ethical Statement
Ethical approval was waived by the Ethics Committee of the regional Medical Association (North-Rhine; Nr. 20210506) because of the retrospective nature of the study, and all the procedures performed were part of routine care. Procedures were followed in accordance with the ethical and data protection standards of the approving committees and with the Helsinki Declaration of 1975.
Informed consent
For this study Informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
11739_2023_3420_MOESM1_ESM.pdf
Supplementary file1 Online Resource 1 Inflammatory biomarkers post- ROSC : At admission (Leuko0,CRP0), 24h (Leuko24,CRP24), 48h (Leuko48,CRP48) and 72h(Leuko72,CRP72) post-ROSC (PDF 93 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Voigt, I., Mighali, M., Wieneke, H. et al. Cardiac arrest related lung edema: examining the role of downtimes in transpulmonary thermodilution analysis. Intern Emerg Med 19, 501–509 (2024). https://doi.org/10.1007/s11739-023-03420-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-023-03420-7