Abstract
Purpose
Predict in advance the need for hospitalization of adult patients for fall-related fractures based on information available at the time of triage to help decision-making at the emergency department (ED).
Methods
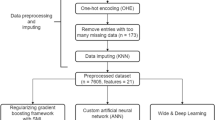
We developed machine learning models using routinely collected triage data at a regional hospital chain in Pennsylvania to predict admission to an inpatient unit. We considered all patients presenting to the ED for fall-related fractures. Patients who were 18 years or younger, who left the ED against medical advice, left the ED waiting room without being seen by a provider, and left the ED after initial diagnostics were excluded from the analysis. We compared models obtained using triage data (pre-model) with models developed using additional data obtained after physicians’ diagnoses (post-model).
Results
Our results show good discriminatory power on predicting hospital admissions. Neural network models performed the best (AUC: pre-model = 0.938 [CI 0.920–0.956], post-model = 0.983 [0.974–0.992]). The logistic regression analysis provides additional insights into the data and the relationships between the variables.
Conclusions
Using limited data available at the time of triage, we developed four machine learning models aimed at predicting hospitalization for patients presenting to the ED for fall-related fractures. All the four models were robust and performed well. Neural network method, however, performed the best for both pre- and post-models. Simple, parsimonious machine learning models can provide high accuracy for predicting hospital admission.

Similar content being viewed by others
Availability of data and material
On request to corresponding author.
Code availability
On request to corresponding author.
References
Owens PL, Russo CA, Spector W, Mutter R (2006) Emergency Department Visits for Injurious Falls among the Elderly, 2006: Statistical Brief #80. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US), Rockville (MD)
Lewiecki EM, Ortendahl JD, Vanderpuye-Orgle J et al (2019) Healthcare policy changes in osteoporosis can improve outcomes and reduce costs in the United States. JBMR Plus. https://doi.org/10.1002/jbm4.10192
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet Lond Engl 359:1761–1767. https://doi.org/10.1016/S0140-6736(02)08657-9
Hoffman GJ, Hays RD, Shapiro MF et al (2017) The costs of fall-related injuries among older adults: annual per-faller, service component, and patient out-of-pocket costs. Health Serv Res 52:1794–1816. https://doi.org/10.1111/1475-6773.12554
Bouee S, Lafuma A, Fagnani F et al (2006) Estimation of direct unit costs associated with non-vertebral osteoporotic fractures in five European countries. Rheumatol Int 26:1063–1072. https://doi.org/10.1007/s00296-006-0180-x
Hartholt KA, Stevens JA, Polinder S et al (2011) Increase in fall-related hospitalizations in the United States, 2001–2008. J Trauma 71:255–258. https://doi.org/10.1097/TA.0b013e31821c36e7
Orces CH (2013) Emergency department visits for fall-related fractures among older adults in the USA: a retrospective cross-sectional analysis of the national electronic injury surveillance system all injury program, 2001–2008. BMJ Open 3:e001722. https://doi.org/10.1136/bmjopen-2012-001722
Shankar K, Liu S, Ganz D (2017) Trends and characteristics of emergency department visits for fall-related injuries in older adults, 2003–2010. West J Emerg Med 18:785–793. https://doi.org/10.5811/westjem.2017.5.33615
Judd KT, Christianson E (2015) Expedited operative care of hip fractures results in significantly lower cost of treatment. Iowa Orthop J 35:62–64
Harvin JA, Harvin WH, Camp E et al (2012) Early femur fracture fixation is associated with a reduction in pulmonary complications and hospital charges: a decade of experience with 1376 diaphyseal femur fractures. J Trauma Acute Care Surg 73:1442–1448. https://doi.org/10.1097/TA.0b013e3182782696
Orosz GM (2004) Association of timing of surgery for hip fracture and patient outcomes. JAMA 291:1738. https://doi.org/10.1001/jama.291.14.1738
Vallier HA, Dolenc AJ, Moore TA (2016) Early appropriate care: a protocol to standardize resuscitation assessment and to expedite fracture care reduces hospital stay and enhances revenue. J Orthop Trauma 30:306–311. https://doi.org/10.1097/BOT.0000000000000524
Orosz GM, Hannan EL, Magaziner J et al (2002) Hip fracture in the older patient: reasons for delay in hospitalization and timing of surgical repair. J Am Geriatr Soc 50:1336–1340. https://doi.org/10.1046/j.1532-5415.2002.50353.x
Morley C, Unwin M, Peterson GM et al (2018) Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS ONE 13:e0203316. https://doi.org/10.1371/journal.pone.0203316
Patterson BW, Engstrom CJ, Sah V et al (2019) Training and interpreting machine learning algorithms to evaluate fall risk after emergency department visits. Med Care 57:560–566. https://doi.org/10.1097/MLR.0000000000001140
Janke AT, Overbeek DL, Kocher KE, Levy PD (2016) Exploring the potential of predictive analytics and big data in emergency care. Ann Emerg Med 67:227–236. https://doi.org/10.1016/j.annemergmed.2015.06.024
Cameron A, Rodgers K, Ireland A et al (2015) A simple tool to predict admission at the time of triage. Emerg Med J 32:174–179. https://doi.org/10.1136/emermed-2013-203200
Hong WS, Haimovich AD, Taylor RA (2018) Predicting hospital admission at emergency department triage using machine learning. PLoS ONE 13:e0201016. https://doi.org/10.1371/journal.pone.0201016
LaMantia MA, Platts-Mills TF, Biese K et al (2010) Predicting hospital admission and returns to the emergency department for elderly patients. Acad Emerg Med 17:252–259. https://doi.org/10.1111/j.1553-2712.2009.00675.x
Parker CA, Liu N, Wu SX et al (2019) Predicting hospital admission at the emergency department triage: a novel prediction model. Am J Emerg Med 37:1498–1504. https://doi.org/10.1016/j.ajem.2018.10.060
Peck JS, Benneyan JC, Nightingale DJ, Gaehde SA (2012) Predicting emergency department inpatient admissions to improve same-day patient flow: predicting ed inpatient admissions. Acad Emerg Med 19:E1045–E1054. https://doi.org/10.1111/j.1553-2712.2012.01435.x
Peck JS, Gaehde SA, Nightingale DJ et al (2013) Generalizability of a simple approach for predicting hospital admission from an emergency department. Acad Emerg Med 20:1156–1163. https://doi.org/10.1111/acem.12244
Raita Y, Goto T, Faridi MK et al (2019) Emergency department triage prediction of clinical outcomes using machine learning models. Crit Care 23:64. https://doi.org/10.1186/s13054-019-2351-7
Sun Y, Heng BH, Tay SY, Seow E (2011) Predicting hospital admissions at emergency department triage using routine administrative data: predicting hospital admission at ED triage. Acad Emerg Med 18:844–850. https://doi.org/10.1111/j.1553-2712.2011.01125.x
Zlotnik A, Alfaro MC, Pérez MCP et al (2016) Building a decision support system for inpatient admission prediction with the Manchester triage system and administrative check-in variables. CIN: Comput Inform Nurs 34:224–230. https://doi.org/10.1097/CIN.0000000000000230
Fernandes M, Mendes R, Vieira SM et al (2020) Predicting Intensive Care Unit admission among patients presenting to the emergency department using machine learning and natural language processing. PLoS ONE 15:e0229331. https://doi.org/10.1371/journal.pone.0229331
Hripcsak G, Sengupta S, Wilcox A, Green RA (2007) Emergency department access to a longitudinal medical record. J Am Med Inform Assoc 14:235–238. https://doi.org/10.1197/jamia.M2206
Joseph JW, Leventhal EL, Grossestreuer AV et al (2020) Deep-learning approaches to identify critically Ill patients at emergency department triage using limited information. J Am Coll Emerg Physicians Open 1:773–781. https://doi.org/10.1002/emp2.12218
Patel SJ, Chamberlain DB, Chamberlain JM (2018) A machine learning approach to predicting need for hospitalization for pediatric asthma exacerbation at the time of emergency department triage. Acad Emerg Med Off J Soc Acad Emerg Med 25:1463–1470. https://doi.org/10.1111/acem.13655
Rowe BH, Villa-Roel C, Guttman A et al (2009) Predictors of hospital admission for chronic obstructive pulmonary disease exacerbations in Canadian emergency departments. Acad Emerg Med Off J Soc Acad Emerg Med 16:316–324. https://doi.org/10.1111/j.1553-2712.2009.00366.x
Goto T, Camargo CA, Faridi MK et al (2018) Machine learning approaches for predicting disposition of asthma and COPD exacerbations in the ED. Am J Emerg Med 36:1650–1654. https://doi.org/10.1016/j.ajem.2018.06.062
Sax DR, Mark DG, Huang J et al (2021) Use of machine learning to develop a risk-stratification tool for emergency department patients with acute heart failure. Ann Emerg Med 77:237–248. https://doi.org/10.1016/j.annemergmed.2020.09.436
Martinez DA, Levin SR, Klein EY et al (2020) Early prediction of acute kidney injury in the emergency department with machine-learning methods applied to electronic health record data. Ann Emerg Med 76:501–514. https://doi.org/10.1016/j.annemergmed.2020.05.026
Miles J, Turner J, Jacques R et al (2020) Using machine-learning risk prediction models to triage the acuity of undifferentiated patients entering the emergency care system: a systematic review. Diagn Progn Res 4:16. https://doi.org/10.1186/s41512-020-00084-1
Trevisan C, Di Gregorio P, Debiasi E et al (2018) Decision tree for ward admissions of older patients at the emergency department after a fall. Geriatr Gerontol Int 18:1388–1392. https://doi.org/10.1111/ggi.13497
Pouramin P, Li CS, Busse JW et al (2020) Delays in hospital admissions in patients with fractures across 18 low-income and middle-income countries (INORMUS): a prospective observational study. Lancet Glob Health 8:e711–e720. https://doi.org/10.1016/S2214-109X(20)30067-X
Mowbray F, Zargoush M, Jones A et al (2020) Predicting hospital admission for older emergency department patients: Insights from machine learning. Int J Med Inf 140:104163. https://doi.org/10.1016/j.ijmedinf.2020.104163
Cawthon PM (2011) Gender differences in osteoporosis and fractures. Clin Orthop 469:1900–1905. https://doi.org/10.1007/s11999-011-1780-7
Kiebzak GM, Beinart GA, Perser K et al (2002) Undertreatment of osteoporosis in men with hip fracture. Arch Intern Med 162:2217–2222. https://doi.org/10.1001/archinte.162.19.2217
Haentjens P, Magaziner J, Colón-Emeric CS et al (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390. https://doi.org/10.7326/0003-4819-152-6-201003160-00008
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
DRP and BR conceived the study. SMR collected the data. DRP performed data wrangling. DRP and BR conceived the study design and analyzed the data. PJ provided advice on clinical aspect of the study. DRP drafted the manuscript, and all authors contributed substantially to its revision. DRP takes responsibility for the paper as a whole.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no conflict of interest.
IRB statement
The data for this were de-identified, non-coded data set, the use of which does not constitute research with human subjects because there is no interaction with any individual and no identifiable private information was used. The study does not therefore require IRB review.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Human and animal rights
There are no human or animals subjects used for research in this article. Human and animal rights is therefore not applicable.
Informed consent
There are no human subjects in this article and informed consent is not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pai, D.R., Rajan, B., Jairath, P. et al. Predicting hospital admission from emergency department triage data for patients presenting with fall-related fractures. Intern Emerg Med 18, 219–227 (2023). https://doi.org/10.1007/s11739-022-03100-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-022-03100-y