Abstract
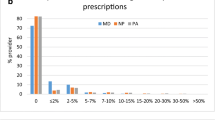
Abuse of opioid prescription drugs has become an epidemic across the developed world. Despite the fact that emergency physicians overall account for a small proportion of total opioids prescribed, the number of prescriptions has risen dramatically in the past decade and, to some degree, contributes to the available supply of opioids in the community, some of which are diverted for non-medical use. Since successfully reducing opioid prescribing on the individual level first requires knowledge of current prescribing patterns, we sought to determine to what extent variation exists in opioid prescribing patterns at our institution. This was a single-institution observational study at a community hospital with an annual ED volume of 47,000 visits. We determined the number of prescriptions written by each provider, both total number and accounting for the number of patients seen. Our primary outcome measure was the level of variation at the physician level for number of prescriptions written per patient. We also identified the mean number of pills written per prescription. We analyzed data from November 13, 2014 through July 31, 2015 for 21 full-time providers. There were a total of 2211 prescriptions for opioids written over this time period for a total of 17,382 patients seen. On a per-patient basis, the rate of opioid prescriptions written per patient during this period was 127 per 1000 visits (95 % CI 122–132). There was a variation on the individual provider level, with rates ranging from 33 per to 332 per 1000 visits. There was also substantial variation by provider in the number of pills written per prescription with coefficient of variation (standard deviation divided by mean) averaged over different opioids ranging from 16 to 40 %. There was significant variation in opioid prescribing patterns at the individual physician level, even when accounting for the number of patients seen.

Similar content being viewed by others
References
Larochelle MR, Liebschutz JM, Zhang F (2016) Opioid prescribing after nonfatal overdose and association with repeated overdose: a cohort study. Ann Intern Med 164(1):1–9
Dhalla IA, Persaud N, Juurlink DN (2011) Facing up to the prescription opioid crisis. BMJ 343:d5142
Silversides A Backgrounder: Canada’s prescription opioid crisis. http://umanitoba.ca/outreach/evidencenetwork/archives/19635. Accessed 26 Mar 2016
Berry PH, Dahl JL (2000) The new JCAHO pain standards: implications for pain management nurses. Pain Manag Nurs 1(1):3–12
Phillips DM (2000) Joint Commission on Accreditation of Healthcare Organizations. JCAHO pain management standards are unveiled. JAMA 284:428–429
Sibert KS (2014) Caught between patient satisfaction and prescription drug abuse. http://www.kevinmd.com/blog/2014/04/caught-patient-satisfaction-prescription-drug-abuse.html. Accessed 14 April 2014
Institute of Medicine (2011) Relieving pain in America: a blueprint for transforming prevention, care, education, and research. National Academies Press, Washington, DC
Paulozzi LJ, Budnitz DS, Xi Y (2006) Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf 15:618–627
Governale L (2009) Outpatient prescription opioid utilization in the U.S., years 2000–2009. US Food and Drug Administration web site
Hoppe JA, Nelson LS, Perrone J et al (2015) Opioid prescribing in a cross section of US emergency departments. Ann Emerg Med 66(3):253.e1–259.e1
Mazer-Amirshahi M, Mullins PM, Rasooly I et al (2014) Rising opioid prescribing in adult U.S. emergency department visits: 2001–2010. Acad Emerg Med 21(3):236
Zgierska A, Miller M, Rabago D (2012) Patient satisfaction, prescription drug abuse, and potential unintended consequences. JAMA 307(13):1377–1378
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board of Beth Israel Deaconess Hospital—Plymouth.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Smulowitz, P.B., Cary, C., Boyle, K.L. et al. Variation in opioid prescribing patterns between ED providers. Intern Emerg Med 11, 1121–1124 (2016). https://doi.org/10.1007/s11739-016-1505-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-016-1505-8