Abstract
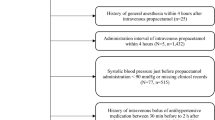
Propacetamol, a water-soluble prodrug form of paracetamol, is hydrolyzed by esterase to generate paracetamol in the blood. Each gram of propacetamol is equal to 0.5 g of paracetamol. It has been reported to cause hypotension in critically ill patients with a fever. We aimed to investigate the hemodynamic effects of propacetamol for the control of fever in patients with diverse severities of illness who were managed in the emergency department (ED). We also aimed to identify clinical factors related to significant hemodynamic alterations in ED patients. This was a retrospective study of 1507 ED patients who received propacetamol. Significant hemodynamic alterations were defined as systolic blood pressure (SBP) <90 mmHg or diastolic blood pressure (DBP) <60 mmHg, or a drop in SBP >30 mmHg, which required treatments with a bolus of fluid or vasopressor administration. Postinfusion SBP and DBP were significantly lower than the preinfusion SBP and DBP. A clinically significant drop in BP occurred in 162 (10.7 %) patients, and interventions were necessary. Among the predictors assessed, congestive heart failure (OR 6.21, 95 % CI 2.67–14.45) and chills (OR 3.10, 95 % CI 2.04–4.70) were independent factors for a significant hemodynamic change. Administration of propacetamol can provoke a reduction in BP in ED patients. This reduction was clinically significant for 10 % of infusions. Clinicians should be aware of this potential deleterious effect, especially in patients with congestive heart failure or who experience chills prior to the administration of propacetamol.


Similar content being viewed by others
References
Chiam E, Weinberg L, Bellomo R (2015) Paracetamol: a review with specific focus on the haemodynamic effects of intravenous administration. Heart Lung Vessel 7(2):121–132
Van Aken H, Thys L, Veekman L, Buerkle H (2004) Assessing analgesia in single and repeated administrations of propacetamol for postoperative pain: comparison with morphine after dental surgery. Anesth Analg 98(1):159–165 (table of contents)
Depre M, van Hecken A, Verbesselt R, Tjandra-Maga TB, Gerin M, de Schepper PJ (1992) Tolerance and pharmacokinetics of propacetamol, a paracetamol formulation for intravenous use. Fundam Clin Pharmacol 6(6):259–262
Boyle M, Nicholson L, O’Brien M, Flynn GM, Collins DW, Walsh WR, Bihari D (2010) Paracetamol induced skin blood flow and blood pressure changes in febrile intensive care patients: an observational study. Aust Crit Care 23(4):208–214. doi:10.1016/j.aucc.2010.06.004
de Maat MM, Tijssen TA, Bruggemann RJ, Ponssen HH (2010) Paracetamol for intravenous use in medium–and intensive care patients: pharmacokinetics and tolerance. Eur J Clin Pharmacol 66(7):713–719. doi:10.1007/s00228-010-0806-5
Krajcova A, Matousek V, Duska F (2013) Mechanism of paracetamol-induced hypotension in critically ill patients: a prospective observational cross-over study. Aust Crit Care 26(3):136–141. doi:10.1016/j.aucc.2012.02.002
Picetti E, De Angelis A, Villani F, Antonini MV, Rossi I, Servadei F, Caspani ML (2014) Intravenous paracetamol for fever control in acute brain injury patients: cerebral and hemodynamic effects. Acta Neurochir (Wien) 156(10):1953–1959. doi:10.1007/s00701-014-2129-2 (discussion 1959)
Vera P, Zapata L, Gich I, Mancebo J, Betbese AJ (2012) Hemodynamic and antipyretic effects of paracetamol, metamizol and dexketoprofen in critical patients. Med Intensiva 36(9):619–625. doi:10.1016/j.medin.2012.02.003
Hersch M, Raveh D, Izbicki G (2008) Effect of intravenous propacetamol on blood pressure in febrile critically ill patients. Pharmacotherapy 28(10):1205–1210. doi:10.1592/phco.28.10.1205
Bektas F, Eken C, Karadeniz O, Goksu E, Cubuk M, Cete Y (2009) Intravenous paracetamol or morphine for the treatment of renal colic: a randomized, placebo-controlled trial. Ann Emerg Med 54(4):568–574. doi:10.1016/j.annemergmed.2009.06.501
Craig M, Jeavons R, Probert J, Benger J (2012) Randomised comparison of intravenous paracetamol and intravenous morphine for acute traumatic limb pain in the emergency department. Emerg Med J 29(1):37–39. doi:10.1136/emj.2010.104687
Eken C, Serinken M, Elicabuk H, Uyanik E, Erdal M (2014) Intravenous paracetamol versus dexketoprofen versus morphine in acute mechanical low back pain in the emergency department: a randomised double-blind controlled trial. Emerg Med J 31(3):177–181. doi:10.1136/emermed-2012-201670
Serinken M, Eken C, Turkcuer I, Elicabuk H, Uyanik E, Schultz CH (2012) Intravenous paracetamol versus morphine for renal colic in the emergency department: a randomised double-blind controlled trial. Emerg Med J 29(11):902–905. doi:10.1136/emermed-2011-200165
Turkcuer I, Serinken M, Eken C, Yilmaz A, Akdag O, Uyan E, Kiray C, Elicabuk H (2014) Intravenous paracetamol versus dexketoprofen in acute migraine attack in the emergency department: a randomised clinical trial. Emerg Med J 31(3):182–185. doi:10.1136/emermed-2013-203044
Avellaneda C, Gomez A, Martos F, Rubio M, Sarmiento J, de la Cuesta FS (2000) The effect of a single intravenous dose of metamizol 2 g, ketorolac 30 mg and propacetamol 1 g on haemodynamic parameters and postoperative pain after heart surgery. Eur J Anaesthesiol 17(2):85–90
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Briasoulis A, Silver A, Yano Y, Bakris GL (2014) Orthostatic hypotension associated with baroreceptor dysfunction: treatment approaches. J Clin Hypertens (Greenwich) 16(2):141–148. doi:10.1111/jch.12258
Vincent JL, De Backer D (2013) Circulatory shock. N Engl J Med 369(18):1726–1734. doi:10.1056/NEJMra1208943
Boyle M, Hundy S, Torda TA (1997) Paracetamol administration is associated with hypotension in the critically ill. Aust Crit Care 10(4):120–122
Needleman SM (2013) Safety of rapid intravenous of infusion acetaminophen. Proc (Bayl Univ Med Cent) 26(3):235–238
Van Dissel JT, Schijf V, Vogtlander N, Hoogendoorn M, van’t Wout J (1998) Implications of chills. Lancet 352(9125):374
Tokuda Y, Miyasato H, Stein GH (2005) A simple prediction algorithm for bacteraemia in patients with acute febrile illness. QJM 98(11):813–820. doi:10.1093/qjmed/hci120
Lee CC, Wu CJ, Chi CH, Lee NY, Chen PL, Lee HC, Chang CM, Ko NY, Ko WC (2012) Prediction of community-onset bacteremia among febrile adults visiting an emergency department: rigor matters. Diagn Microbiol Infect Dis 73(2):168–173. doi:10.1016/j.diagmicrobio.2012.02.009
Tokuda Y, Miyasato H, Stein GH, Kishaba T (2005) The degree of chills for risk of bacteremia in acute febrile illness. Am J Med 118(12):1417. doi:10.1016/j.amjmed.2005.06.043
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
The study was approved by the local institutional committee for human research.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Bae, Ji., Ahn, S., Lee, YS. et al. Clinically significant hemodynamic alterations after propacetamol injection in the emergency department: prevalence and risk factors. Intern Emerg Med 12, 349–355 (2017). https://doi.org/10.1007/s11739-016-1460-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-016-1460-4