Abstract
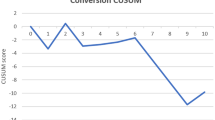
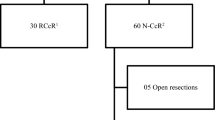
Robotic-assisted surgery is evolving, with improving clinical and cancer outcomes. The aim of this study was to present the clinical and cancer outcomes of patients undergoing robotic-assisted colorectal surgery (RAS-CR) at University Hospital Limerick (UHL) since its introduction to the 100th case, using the daVinci Xi dual-console surgical system. The RAS-CR programme at UHL commenced in June 2016 and the 100th case was performed in July 2019. All patient-related data were recorded prospectively during the perioperative period by the RAS-CR team. Statistical analysis was performed using SPSS, version 22. One hundred patients were operated on, comprising of 47 males and 53 females. The median age was 65 years (IQR 13.0; range 25–84) with 69% of cases performed for cancer [N = 39 rectal cancer, N = 30 colon cancer], 20% for benign disease and 11% for dysplasia. Median length of stay for cancer operations was 6.5 days for colon cancer cases (5.0 days when cases with complications were excluded) and 7.0 days for rectal cancer cases. Median operative time was 255 mins (IQR 130 min; all cases), median docking time was 33 mins (IQR 20 mins) and median intra-operative blood loss was 80 ml (IQR 70 ml). Thirty-one patients developed a post-operative complication (5% anastomotic leak; 13% SSI). In cancer cases, median nodal harvest was 14 nodes (IQR10) and an R0 resection was achieved in 98.6% (n = 68) of cancer cases. Three patients (4.3%) developed metastatic disease at a median interval of 16.5 months. Clinical and operative outcomes remained stable over time from case 1 to 100. Structured introduction of a RAS-CR programme with appropriate governance and continuous audit results in favourable clinical and cancer outcomes and provides an excellent training opportunity for surgical residents.
Similar content being viewed by others
References
Kelley WE (1990s) The evolution of laparoscopy and the revolution in surgery in the decade of the 1990s. J Soc Laparoendosc Surg 12(4):351–357
Pascual M, Salvans S, Pera M (2016) Laparoscopic colorectal surgery: Current status and implementation of the latest technological innovations. World J Gastroenterol 22(2):704–717
Noguera JF (2012) NOTES, MANOS, SILS and other new laparoendoscopic techniques. World J Gastrointest Endosc 4(6):212
Pigazzi A, Baek SK, Carmichael JC (2013) Robotic surgery: colon and rectum. Cancer J 19(2):140–146
Sivathondan PC, Jayne DG (2018) The role of robotics in colorectal surgery. Ann R Coll Surg Engl 100:42–53
Miskovic D et al (2019) European consensus on the standardization of robotic total mesorectal excision for rectal cancer. Color Dis 21(3):270–276
Heald R (1988) The ‘Holy Plane’ of rectal surgery. J R Soc Med 81(9):503–508
Connelly TM, Malik Z, Sehgal R, Byrnes G, Coffey JC, Peirce C (2019) The 100 most influential manuscripts in robotic surgery: a bibliometric analysis. J Robot Surg 14(1):155–165
Jayne D et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer the rolarr randomized clinical trial. JAMA 318(16):1569–1580
Khan JS, Banerjee AK, Kim S-H, Rockall TA, Jayne DG (2018) Robotic rectal surgery has advantages over laparoscopic surgery in selected patients and centres. Color Dis 20(10):845–853
Luca F et al (2018) Sexual and urinary outcomes in robotic rectal surgery: review of the literature and technical considerations. Updates Surg 70(3):415–421
Kim NK, Kim YW, Cho MS (2015) Total mesorectal excision for rectal cancer with emphasis on pelvic autonomic nerve preservation: expert technical tips for robotic surgery. Surg Oncol 24(3):172–180
Rouanet P et al (2018) Robotic versus laparoscopic total mesorectal excision for sphincter-saving surgery: results of a single-center series of 400 consecutive patients and perspectives. Ann Surg Oncol 25(12):3572–3579
Kim HJ, Choi GS, Park JS, Park SY, Yang CS, Lee HJ (2018) The impact of robotic surgery on quality of life, urinary and sexual function following total mesorectal excision for rectal cancer: a propensity score-matched analysis with laparoscopic surgery. Color Dis 20(5):O103–O113
RC, Deleon MF, Maloney Patel N (2015) Robotic colorectal surgery: outcomes and cost analysis at a single institution. In: American Society of Colon and Rectal Surgeons Annual Scientific Meeting, p MA2015
RC Deleon (2015) The economics of robotic colorectal surgery. In: American society of colon and rectal surgeons annual scientific meeting, Boston, p MA2015
Kim J et al (2017) Robotic resection is a good prognostic factor in rectal cancer compared with laparoscopic resection: long-term survival analysis using propensity score matching. Dis Colon Rectum 60(3):266–273
I. Surgical Xi User Manual. [Online]. https://www.intuitive.com/en-us/products-and-services/da-vinci
Berriós-Torres SI et al (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 152(8):784–791
Strasberg S, Clavien PA, Sanabria JR (1992) Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery 111(5):518–526
Wittekind C, Sobin LH, Gospodarowicz MK (2009) TNM classification of malignant tumours, 7th edn. Wiley-Blackwell, USA
Panteleimonitis S, Ahmed J, Harper M, Parvaiz A (2016) Critical analysis of the literature investigating urogenital function preservation following robotic rectal cancer surgery. World J Gastrointest Surg 8(11):744
Kim MJ et al (2018) Robot-assisted versus laparoscopic surgery for rectal cancer: a phase II open label prospective randomized controlled trial. Ann Surg 267(2):243–251
ISRC (2019) PERioperative Fluid Management in Elective ColecTomy (PERFECT)—a national prospective cohort study. Irish J Med Sci. https://doi.org/10.1007/s11845-019-02003-w
Gill M, Fligelstone L, Keating J, Jayne DG, Renton S, Shearman CP (2019) Avoiding, diagnosing and treating well leg compartment syndrome after pelvic surgery. Br J Surg 106(9):1156–1166
Becerra A, Justiniano CF, Aquina CT, Fleming FJ, Xu Z, Boscoe FP, Schymura MJ, Temple LK (2019) Hospital and surgeon variation in positive circumferential resection margin among rectal cancer patients. Am J Surg pii:S0002
Bolger JC et al (2017) Initial experience with a dual-console robotic-assisted platform for training in colorectal surgery. Tech Coloproctol 21(9):721–727
Acknowledgements
I would like to acknowledge the dedicated work of all members of the robotic-assisted surgery programme at University Hospital Limerick for their contribution to the clinical practice upon which this manuscript is based.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Christina A Fleming, Daniel B Westby, Muhammad F Ullah, Helen M Mohan, Rishabh Sehgal, Jarlath C Bolger, Donal P O’Leary, Emma McNamara, Grzegorz Korpanty, Mazen El Bassiouni, Eoghan Condon, J Calvin Coffey, Colin Peirce declares that s/he has no conflict of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fleming, C.A., Westby, D., Ullah, M.F. et al. A review of clinical and oncological outcomes following the introduction of the first robotic colorectal surgery programme to a university teaching hospital in Ireland using a dual console training platform. J Robotic Surg 14, 889–896 (2020). https://doi.org/10.1007/s11701-020-01073-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-020-01073-8