Abstract
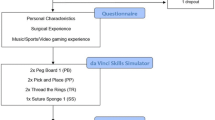
To investigate whether the learning curve of robotic surgery simulator training depends on the probands’ characteristics, such as age and prior experience, we conducted a study of six distinct proband groups, using the da Vinci Skills Simulator: experienced urological robotic surgeons, surgeons with experience as da Vinci tableside assistants, urological surgeons with laparoscopic experience, urological surgeons without laparoscopic experience, and complete novices aged 25 and younger and 40 and older. The results showed that all experienced robotic surgeons reached expert level (>90 %, as defined previously in the literature) within the first three repetitions and remained on a high level of performance. All other groups performed worse. Tableside assistants, laparoscopically experienced surgeons, and younger novices showed a better performance in all exercises than surgeons without laparoscopic experience and older novices. A linear mixed-effects model analysis demonstrated no significant difference in learning curves between proband groups in all exercises except the RW1 exercise for the younger proband group. In summary, we found that performance in robotic surgery, measured by performance scores in three virtual simulator modules using the EndoWrist techniques, was dependent on age and prior experience with robotic and laparoscopic surgery. However, and most importantly, the learning curve was not significantly affected by these factors. This suggests that the da Vinci Skills Simulator™ is a useful practice tool for everyone learning or performing robotic surgery, and that early selection of talented surgeons is neither possible nor necessary.




Similar content being viewed by others
References
Yates DR, Vaessen C, Roupret M (2011) From Leonardo to da Vinci: the history of robot-assisted surgery in urology. BJU Int 108:1708–1713. doi:10.1111/j.1464-410X.2011.10576.x (discussion 1714)
Rassweiler J, Hruza M, Teber D, Su L-M (2006) Laparoscopic and robotic assisted radical prostatectomy—critical analysis of the results. Eur Urol 49:612–624. doi:10.1016/j.eururo.2005.12.054
Ou YC, Yang CR, Wang J et al (2010) Robotic-assisted laparoscopic radical prostatectomy: learning curve of first 100 cases. Int J Urol Off J Jpn Urol Assoc 17:635–640. doi:10.1111/j.1442-2042.2010.02546.x
Weinberg L, Rao S, Escobar PF (2011) Robotic surgery in gynecology: an updated systematic review. Obstet Gynecol Int 2011:852061. doi:10.1155/2011/852061
Salö M, Sjöberg Altemani T, Anderberg M (2016) Pyeloplasty in children: perioperative results and long-term outcomes of robotic-assisted laparoscopic surgery compared to open surgery. Pediatr Surg Int. doi:10.1007/s00383-016-3869-2
Meyer M, Gharagozloo F, Tempesta B et al (2012) The learning curve of robotic lobectomy. Int J Med Robot Comput Assist Surg MRCAS 8:448–452. doi:10.1002/rcs.1455
Orvieto MA, Marchetti P, Castillo OA et al (2011) Robotic technologies in surgical oncology training and practice. Surg Oncol 20:203–209. doi:10.1016/j.suronc.2010.08.005
Hu D, Gong Y, Hannaford B, Seibel EJ (2015) Path planning for semi-automated simulated robotic neurosurgery. Proc IEEERSJ Int Conf Intell Robots Syst 2015:2639–2645. doi:10.1109/IROS.2015.7353737
Bourcier T, Chammas J, Becmeur P-H et al (2015) Robotically assisted pterygium surgery: first human case. Cornea 34:1329–1330. doi:10.1097/ICO.0000000000000561
Health Quality Ontario (2010) Robotic-assisted minimally invasive surgery for gynecologic and urologic oncology: an evidence-based analysis. Ont Health Technol Assess Ser 10:1–118
Amodeo A, Linares Quevedo A, Joseph JV et al (2009) Robotic laparoscopic surgery: cost and training. Minerva Urol E Nefrol Ital J Urol Nephrol 61:121–128
Moore LJ, Wilson MR, McGrath JS et al (2015) Surgeons’ display reduced mental effort and workload while performing robotically assisted surgical tasks, when compared to conventional laparoscopy. Surg Endosc 29:2553–2560. doi:10.1007/s00464-014-3967-y
Kho RM (2011) Comparison of robotic-assisted laparoscopy versus conventional laparoscopy on skill acquisition and performance. Clin Obstet Gynecol 54:376–381. doi:10.1097/GRF.0b013e31822b46f6
Lavery HJ, Small AC, Samadi DB, Palese MA (2011) Transition from laparoscopic to robotic partial nephrectomy: the learning curve for an experienced laparoscopic surgeon. JSLS J Soc Laparoendosc Surg Soc Laparoendosc Surg 15:291–297. doi:10.4293/108680811X13071180407357
Patel VR, Tully AS, Holmes R, Lindsay J (2005) Robotic radical prostatectomy in the community setting—the learning curve and beyond: initial 200 cases. J Urol 174:269–272. doi:10.1097/01.ju.0000162082.12962.40
Diana M, Marescaux J (2015) Robotic surgery. Br J Surg 102:e15–e28. doi:10.1002/bjs.9711
Hung AJ, Patil MB, Zehnder P et al (2012) Concurrent and predictive validation of a novel robotic surgery simulator: a prospective, randomized study. J Urol 187:630–637. doi:10.1016/j.juro.2011.09.154
Seixas-Mikelus SA, Kesavadas T, Srimathveeravalli G et al (2010) Face validation of a novel robotic surgical simulator. Urology 76:357–360. doi:10.1016/j.urology.2009.11.069
Seixas-Mikelus SA, Stegemann AP, Kesavadas T et al (2011) Content validation of a novel robotic surgical simulator. BJU Int 107:1130–1135. doi:10.1111/j.1464-410X.2010.09694.x
Kesavadas T, Stegemann A, Sathyaseelan G et al (2011) Validation of robotic surgery simulator (RoSS). Stud Health Technol Inform 163:274–276
Lerner MA, Ayalew M, Peine WJ, Sundaram CP (2010) Does training on a virtual reality robotic simulator improve performance on the da Vinci surgical system? J Endourol Endourol Soc 24:467–472. doi:10.1089/end.2009.0190
Ramos P, Montez J, Tripp A et al (2014) Face, content, construct and concurrent validity of dry laboratory exercises for robotic training using a global assessment tool. BJU Int 113:836–842. doi:10.1111/bju.12559
Kenney PA, Wszolek MF, Gould JJ et al (2009) Face, content, and construct validity of dV-trainer, a novel virtual reality simulator for robotic surgery. Urology 73:1288–1292. doi:10.1016/j.urology.2008.12.044
Perrenot C, Perez M, Tran N et al (2012) The virtual reality simulator dV-Trainer(®) is a valid assessment tool for robotic surgical skills. Surg Endosc 26:2587–2593. doi:10.1007/s00464-012-2237-0
Korets R, Mues AC, Graversen JA et al (2011) Validating the use of the Mimic dV-trainer for robotic surgery skill acquisition among urology residents. Urology 78:1326–1330. doi:10.1016/j.urology.2011.07.1426
Lee JY, Mucksavage P, Kerbl DC et al (2012) Validation study of a virtual reality robotic simulator—role as an assessment tool? J Urol 187:998–1002. doi:10.1016/j.juro.2011.10.160
Lendvay TS, Casale P, Sweet R, Peters C (2008) VR robotic surgery: randomized blinded study of the dV-Trainer robotic simulator. Stud Health Technol Inform 132:242–244
Walliczek U, Förtsch A, Dworschak P et al (2015) Effect of training frequency on the learning curve on the da Vinci Skills Simulator. Head Neck. doi:10.1002/hed.24312
Hagen ME, Wagner OJ, Inan I, Morel P (2009) Impact of IQ, computer-gaming skills, general dexterity, and laparoscopic experience on performance with the da Vinci surgical system. Int J Med Robot Comput Assist Surg MRCAS 5:327–331. doi:10.1002/rcs.264
Yoo BE, Kim J, Cho JS et al (2015) Impact of laparoscopic experience on virtual robotic simulator dexterity. J Minimal Access Surg 11:68–71. doi:10.4103/0972-9941.147696
Kim HJ, Choi G-S, Park JS, Park SY (2014) Comparison of surgical skills in laparoscopic and robotic tasks between experienced surgeons and novices in laparoscopic surgery: an experimental study. Ann Coloproctol 30:71–76. doi:10.3393/ac.2014.30.2.71
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Meier M, Horton K, and John H declare that they have no conflict of interest.
Ethics
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed written consent was obtained from all individual participants included in the study. The participants were informed that the researchers were not affiliated with the manufacturer of the da Vinci Surgical System and the da Vinci Skills Simulator™ and that all data were to be analyzed anonymously.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Meier, M., Horton, K. & John, H. Da Vinci© Skills Simulator™: is an early selection of talented console surgeons possible?. J Robotic Surg 10, 289–296 (2016). https://doi.org/10.1007/s11701-016-0616-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-016-0616-6