Abstract
Leakage at the urethrovesical anastomosis in the post-operative period can result in morbidity including ileus. We examined the effectiveness of using a fibrin sealant at the anastomosis to limit urine leakage thereby facilitating earlier Jackson–Pratt drain and Foley catheter removal following robotic assisted laparoscopic prostatectomy (RALRP). Forty consecutive patients underwent RALRP by one surgeon at our institution. The first 20 patients underwent standard operation and served as the control group. The subsequent 20 patients underwent the same operation with addition of fibrin sealant following a running absorbable sutured urethrovesical anastomosis. The two groups were compared for age (60.5 vs. 58.2 years), pre-operative PSA (5.23 vs. 4.71), Gleason score (6.3 vs. 6.5), stage at resection, and prostate size at resection (51.7 vs. 47.7 g). Wilcoxon rank sum test determined no statistically significant differences in the groups. Patients in the fibrin sealant group had 1.3 versus 2.1 days with a Jackson–Pratt drain, 9.75 versus 12.1 days with a catheter, and an average of 38.6 versus 63.2 cc of drainage per shift. Catheters were removed when a cystogram demonstrated no extravasation of contrast. Two patients in the control group and no patients in the fibrin sealant group had large-volume leakage and ileus post-operatively. In patients undergoing RALRP, application of fibrin sealant at the urethrovesical anastomosis appears to facilitate sealing, thereby allowing earlier removal of the JP drain, by 0.8 days, and the Foley catheter, by 2.35 days, than in controls. No patients in the fibrin sealant group suffered post-operative ileus. This adjunct may be especially useful early in the learning process to reduce morbidity.
Similar content being viewed by others
Introduction
First approved for use in 1988 [1] the applications of liquid fibrin sealant are expanding with current guidelines indicating improved safety and efficacy of two-component fibrin sealant products such as Tisseel VH (Baxter, Westlake Village, CA, USA) [2, 3]. Current applications in urology utilize both the hemostatic and sealant properties. [4, 5] Fibrin sealants have been used for urologic application including partial nephrectomy (laparoscopic and open surgical procedures), which takes advantage of the hemostatic properties [5–7], and during hypospadias surgery, fistula repair, and urethroplasty, which employ the sealant properties. [6, 8, 9] More recently, use of fibrin sealant at the urethrovesical anastomosis in radical retropubic prostatectomy has been employed to facilitate earlier catheter removal [10] and decreased urinary leakage [11]. No studies have been done to date expanding this use into robotic surgery but, by inference, application of fibrin sealant at the urethrovesical anastomosis during RALRP may offer advantages.
At our institution, patients undergoing robotic assisted laparoscopic radical prostatectomy are routinely discharged on post-operative day one with minimal morbidity. The protocol for post-operative care is adjusted to account for the minimally invasive nature of the procedure. Jackson–Pratt drains are removed prior to discharge if volumes remain less than 60 cc after ambulation. Foley catheters are removed at one week if a cystogram shows no leak. In our study, we questioned whether the application of Tisseel VH, a two component fibrinogen and activated thrombin sealant, at the anastomosis of the urethra and bladder after radical robotic prostatectomy confers any advantages.
Materials and methods
After completion of the first 100 cases, to minimize the effect of the learning curve [12], 40 consecutive men underwent RALP by one surgeon (WDS) at our institution. All patients were referred for elevated PSA and biopsy-proven prostate cancer.
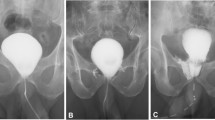
Robotic assisted laparoscopic radical prostatectomy was performed in the standard transperitoneal fashion in the manner described in 2002 by Menon [13, 14] After prostate removal, the urethrovesical anastomosis is sutured in a running fashion with 3-0 monocryl. An 18 French silicone foley catheter is placed prior to the completion of the anastomosis and the balloon inflated with 12 cc of normal saline. The bladder neck and urethra are approximated over the catheter prior to the final anastomotic sutures and any slack in the running suture is removed. The first 20 men had the running sutured anastomosis without addition of fibrin sealant and served as the control group. The second group of 20 men underwent the running anastomosis in the same standard fashion with addition of 6 cc fibrin sealant Tisseel VH in an omega pattern starting at the right posterior and moving to the left posterior border. The laparoscopic applicator is passed through the right assistant 12 French port. (Fig. 1). Both groups of patients had a 15 French round JP drain placed at the urethrovesical anastomosis, via the 5 mm suction port, at the completion of the case.
Patients were discharged to the post anesthesia care unit and then to the surgical floor where output from the JP drain was measured for eight-hour intervals. Drains were removed when output was less than 60 cc per shift after ambulation. Volume of JP output per shift, date of JP removal, and date of discharge were recorded for each patient and obtained from the medical record and bedside chart. Patients were scheduled for follow up at seven days with a cystogram. Hundred and fifty milliliters of dilute Omnipaque contrast material were instilled under gravity per catheter under fluoroscopic guidance. If leak was demonstrated the procedure was repeated a week later. Date of removal of Foley catheter was recorded as was presence or absence of anastomotic leak.
Data were collected in a retrospective chart review for factors that would influence tissue healing, including smoking history, use of steroids, and presence of diabetes. Presence of ileus, readmission data, and follow up were also obtained retrospectively. The University of Virginia Institutional Review Board approved the study.
Prostate specimens were sent to pathology for analysis upon removal. Prostate size was measured in grams. Final pathologic staging was determined by the pathologist at the time of accessioning as was Gleason grade on the prostate specimen.
Mean, standard deviation, and standard error were calculated for the data in each group. Wilcoxon rank sum test was used to determine statistical significance for the comparison.
Results
The control group and the Tisseel VH group were matched for age, preoperative PSA, Gleason grade, prostate size, and pathologic stage at removal. There were no statistically significant differences between the two groups (Table 1).
The Jackson–Pratt drain was removed on mean POD 2.1 (range 1–13 SE 0.632) in the control group and mean POD 1.3 (range 1–3 SE 0.147) in the Tisseel group (P = 0.23). This was equivalent to a mean of 3.8 nursing shifts (range 2–8 SE 0.484) in the control and a mean of 3.1 nursing shifts (range 2–8 SE 0.347) in the Tisseel group (P = 0.24). Patients were discharged on POD 1.4 (range 1–3 SE 0.152) in the control, and POD 1.3 (range 1–3 SE 0.147) in the Tisseel group (P = 0.64). For the control group the cc per shift JP output was 63.24 (range 8–435 SE 20.75). For the Tisseel group the cc per shift JP output was 38.65 (range 0–100 SE 4.84) (P = 0.26). Catheter removal was on POD 12.1 (range 7–26 SE 1.397) in the control group. In the Tisseel group the catheter was removed on POD 9.75 (range 7–18 SE 0.602) (P = 0.13) (Table 2).
One patient in the Tisseel group failed one cystogram trial, and no patient was readmitted with large-volume leak or ileus. In the control group, two patients failed one cystogram trial, one patient failed two cystogram trials, and two patients were readmitted with large-volume drain/drain site output and ileus Table 3.
Factors potentially contributing to poor wound healing and thereby affecting results were also taken into account (Table 3). Smoking history, steroid use, and diabetes diagnosis were all retrospectively reviewed. In the control group: one patient had diet-controlled diabetes, no patient had a history of steroid use, eight patients were former smokers, and one patient was a current smoker. In the Tisseel group: no patient had diabetes, no patient had a history of steroid use, ten patients were former smokers, and one patient was a current smoker. No statistically significant differences were noted in these parameters for the two groups.
Discussion
First introduced for use in cardiothoracic surgery in 1988 [1], the use of fibrin sealant and other tissue sealant and hemostatic products has expanded across surgical disciplines in the last two decades. In urology, fibrin sealants are the most commonly employed, and though many applications are off-label uses, there has been mounting evidence for their usefulness in urology [6–11]. Diner et al. [11] report that use in radical retropubic prostatectomy decreases perioperative drain output, and suggest that in some patients undergoing traditional open radical prostatectomy application of fibrin sealant could accelerate discharge. Morey et al. have applied fibrin sealant in simple retropubic prostatectomy and those patients required no perioperative drain [15]. Evans et al. [8] report success with use of fibrin sealant in trauma and fistula repair. Novel uses of fibrin sealant in urology utilize its use as a hemostatic adjunct in partial nephrectomy and renal trauma, and as a sealant in hypospadias, ureteral anastomoses, and urethroplasty [6, 8]. Several case reports and small series exist supporting the use in pyeloplasty, vasovasostomy, ureteral anastomosis, and open radical prostatectomy. In our study we expand the potential use to include reinforcing the urethrovesical anastomosis in RALRP. Already shown to reduce drain output in the open radical prostatectomy [11] and to assist in the two-sutured anastomotic technique described by Gallo et al [16], Tisseel’s use in this realm seems a natural progression given the minimally invasive nature of the procedure and reduced hospital stay.
In our study, the main outcome difference noted was in leakage prior to catheter removal. We were not able to find a statistically significant difference in JP drain output or days with JP drain, likely because most patients with JP drains have them removed after a relatively short interval. JP was removed in 2.1 versus 1.3 days in the control and Tisseel groups (P = 0.23). Similarly discharge home was not statistically different with most patients able to leave on POD 1. Days in the hospital were 1.4 in the control group and 1.3 in the Tisseel group. Catheter removal was earlier in the study group 9.75 versus 12.1 days, with a trend toward statistical difference (P = 0.13) (Table 2).
Where the use of fibrin sealant was most noticeable was at follow up cystogram and catheter removal. Once Tisseel was introduced, only one patient had leak on cystogram and had to return for a repeat cystogram compared to six in the control group. No patient was readmitted with leak or ileus in the study population while two in the control group were readmitted with ileus. We examined other factors that could account for poor tissue healing including smoking, steroid use, and diabetes and found no significant differences. We conclude that application of the fibrin sealant aids in healing and sealing the anastomosis and accounts for the reduced leakage.
Conclusion
Use of fibrin sealant in urology can be expanded to include reinforcing the suture line in the urethrovesical anastomosis in RALRP. Application of fibrin sealant at the urethrovesical anastomosis appears to facilitate sealing, thereby allowing earlier removal of the JP drain by 0.8 days and the Foley catheter by 2.35 days in patients undergoing RALRP. No patients in the fibrin sealant group suffered post-operative ileus. This adjunct may be especially useful early in the learning process to reduce morbidity. Further study to validate the procedure should be undertaken and a cost-effective approach to use should be employed.
References
US Department of Health and Human Services, New fibrin sealant approved to help control bleeding in surgery. FDA Talk paper T98–22 May 1988
KH Siedentop et al (2001) Safety and Efficacy of Currently available Fibrin tissue Adhesives. Am J Otolaryngol 22(4):230–235
S Basu, CP Marini, FG Bauman et al (1995) Comparative study of biological glues: cryoprecipitate glue, two-component fibrin sealant, and “French glue.” Ann Thorac Surg 60(5):1255–1262
B Shekarriz, ML Stoller (2002) The use of fibrin sealant in urology. J Urol 167(3):1218–1225
YM Hong, KR Louglhlin (2006) The use of hemostatic agents and sealants in urology. J Urol 176:2367–2374
LA Evans, AF Morey (2006) Current applications of Fibrin Sealant in Urologic Surgery. Int Braz J Urol 32:131–141
U Kumar, DM Albala (2001) Fibrin glue applications in urology. Curr Urol Rep 2(1):79–82
LA Evans, KH Ferguson, JP Foley, TA Rozanski, AF Morey (2003) Fibrin sealant for the management of genitourinary injuries, fistulas, and surgical complications. J Urol 169(4):1360–1362
MF MacDonald, RA Santucci (2006) Adjunctive use of fibrin sealant in urethroplasty for early catheter removal. Issues Urol 36–40
EJ Hick, AF Morey (2004) Initial experience with fibrin sealant in pendulous urethral reconstruction. Is early catheter removal possible? J Urol 171:1547–1549
EK Diner, SV Patel, AM Kwart (2005) Does fibrin sealant decrease immediate urinary leakage following radical retropubic prostatectomy? J Urol 173:1147–1149
TE Ahlering, D Skarecky et al (2003) Successful transfer of open surgical skills to a laparoscopic environment using a robotic interface: initial experience with laparoscopic radical prostatectomy. J Urol 170(5):1738–1741
M Menon, A Shrivastava, A Tewari et al (2002) Laparoscopic and robot assisted radical prostatectomy: establishment of a structured program and preliminary outcomes. J Urol 168(3):945–949
M Menon et al (2003) Vattikuti institute prostatectomy: technique. J Urol 169(6):2289–2292
AF Morey, RC McDonough et al (2002) Drain free simple retropubic prostatectomy using fibrin sealant. J Urol 168:627
L Gallo, S Perdone et al (2007) Vesicourethral anastomosis during radical retropubic prostatectomy: does the number of sutures matter? Urology 69(3)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Flury, S.C., Starnes, D.N. & Steers, W.D. Application of fibrin sealant at the urethrovesical anastomosis in robotic assisted radical prostatectomy: does it enable earlier Foley catheter and Jackson–Pratt drain removal?. J Robotic Surg 1, 303–306 (2008). https://doi.org/10.1007/s11701-007-0061-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-007-0061-7