Abstract
Introduction
The inflammatory state that accompanies adiposity and the metabolic syndrome (MetS) is called “low-grade” inflammation. White blood cell count (WBC) has been proposed as an emerging biomarker for predicting future cardiovascular events, MetS and mortality. Bariatric surgery (BS) improves comorbidities associated with obesity and the MetS and the surgically induced weight loss is known to improve inflammatory status.
Objectives
To analyze the improvement of low-grade inflammation associated to obesity in patients with metabolically healthy severe obesity (MHSO) and patients with metabolically unhealthy obesity (MUSO) (severe obesity with MetS) after primary bariatric surgery as well as the protective effect of BS against the development of MetS in patients with MHSO by reducing the WBC.
Materials and methods
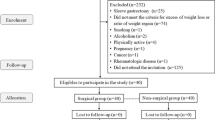
Retrospective analysis of prospectively collected data of patients undergoing laparoscopic primary BS (gastric by-pass or sleeve gastrectomy) from January 2004-December 2015. Outcomes included changing of low-grade inflammation in terms of leukocytes, neutrophils, lymphocytes, and platelets.
Results
Twenty-one patients with MHSO and 167 patients with MUSO underwent laparoscopic primary BS. The preoperative values of leukocyte and platelet were statistically higher in the group of patients with MHSO. In both groups, there was significant postoperative decrease of inflammatory markers. The greatest drop in WBC occurred in the second postoperative year. No patient of the group of patients with MHSO developed MetS within five postoperative years.
Conclusions
Surgically induced weight loss plays an important role for improvement in chronic inflammation associated to obesity because of reduction of visceral fat mass. MHSO associates a low-grade chronic inflammatory status comparable to MUSO. The improvement or decrease of low-grade inflammation in patients with metabolically healthy severe obesity after bariatric surgery could have a protective effect against the development of MetS and medical conditions associated with severe obesity.
Graphical abstract




Similar content being viewed by others
Abbreviations
- IR:
-
insulin resistance
- MetS:
-
metabolic syndrome
- WAT:
-
white adipose tissue
- TNF-a:
-
tumor necrosis alpha
- IL-6:
-
interleukin-6
- WBC:
-
white blood cell count
- CRP:
-
C reactive protein
- BS:
-
bariatric and metabolic surgery
- MHSO:
-
metabolically healthy severe obesity
- MUSO:
-
metabolically unhealthy obesity
- LGBP:
-
laparoscopic gastric by-pass
- LSG:
-
laparoscopic sleeve gastrectomy
- BMI:
-
body mass index
- T2D:
-
type 2 diabetes
- AHT:
-
arterial hypertension
- DL:
-
dyslipidemia
- OSAS:
-
obstructive sleep apnea syndrome
- % EBMIL:
-
% Excess BMI Loss
- % TWL:
-
% Total Weight Loss
- FU:
-
follow-up
- PO:
-
postoperative
- T0:
-
preoperative time
- T1:
-
first postoperative year
- T2:
-
second postoperative year
- T5:
-
fifth postoperative year
References
Sjöström L, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93. https://doi.org/10.1056/nejmoa035622.
Chiappetta S, et al. The impact of obesity and metabolic surgery on chronic inflammation. Obes Surg. 2018;28:3028–40. https://doi.org/10.1007/s11695-018-3320-y.
Askarpour M, Khani D, Sheikhi A, Ghaedi E, Alizadeh S. Effect of bariatric surgery on serum inflammatory factors of obese patients: a systematic review and meta-analysis. Obes Surg. 2019;29:2631–47. https://doi.org/10.1007/s11695-019-03926-0.
Odagiri K, Uehara A, Mizuta I, Yamamoto M, Kurata C. Longitudinal study on white blood cell count and the incidence of metabolic syndrome. Intern Med. 2011;50:2491–8. https://doi.org/10.2169/internalmedicine.50.5877.
Babio N, et al. White blood cell counts as risk markers of developing metabolic syndrome and its components in the PREDIMED study. PLoS One. 2013;8:e58354. https://doi.org/10.1371/journal.pone.0058354.
Dixon JB, O’Brien PE. Obesity and the white blood cell count: changes with sustained weight loss. Obes Surg. 2006;16:251–7. https://doi.org/10.1381/096089206776116453.
Tsai JCR, Sheu S-H, Chiu H-C, Chung F-M, Chang D-M, Chen M-P, Shin S-J, Lee Y-J. Association of peripheral total and differential leukocyte counts with metabolic syndrome and risk of ischemic cardiovascular diseases in patients with type 2 diabetes mellitus. Diabetes Metab Res Rev. 2007;23:111–8. https://doi.org/10.1002/dmrr.647.
Zimmet P, Alberti KGMM, Serrano Ríos M. Una nueva definición mundial del síndrome metabólico propuesta por la Federación Internacional de Diabetes: fundamento y resultados. Rev Española Cardiol. 2005;58:1371–6. https://www.revespcardiol.org/es-una-nueva-definicion-mundial-del-articulo-13082533.
Hotamisligil GS. Foundations of immunometabolism and implications for metabolic health and disease. Physiol Behav. 2017;47:406–20. https://doi.org/10.1016/j.immuni.2017.08.009.
De Luca M, et al. Indications for surgery for obesity and weight-related diseases: position statements from the international federation for the surgery of obesity and metabolic disorders (IFSO). Obes Surg. 2016;26:1659–96.
Minervino D, et al. Leukocyte activation in obese patients: effect of bariatric surgery. Med (United States). 2015;94:1–7. https://doi.org/10.1097/md.0000000000001382.
Stefan N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 2020;8:616–27. https://doi.org/10.1016/s2213-8587(20)30110-8.
Bahadır A, et al. Is the neutrophil-to-lymphocyte ratio indicative of inflammatory state in patients with obesity and metabolic syndrome? Anadolu Kardiyol Derg. 2015;15:816–22. https://doi.org/10.5152/akd.2014.5787.
Biobaku F, Ghanim H, Monte SV, Caruana JA, Dandona P. Bariatric surgery: remission of inflammation, cardiometabolic benefits, and common adverse effects. J Endocr Soc. 2020;4:1–17. https://doi.org/10.1210/jendso/bvaa049.
Fenske WK, et al. Effect of bariatric surgery-induced weight loss on renal and systemic inflammation and blood pressure: a 12-month prospective study. Surg Obes Relat Dis. 2013;9:559–68. https://doi.org/10.1016/j.soard.2012.03.009.
Recarte M, Corripio R, De Cos AI, Vesperinas G, Díaz, and Joaquín. Low-grade systemic inflammation: gastric bypass and sleeve gastrectomy. Obes Surg. 2019;29, 347–1720: 180–181. https://doi.org/10.1007/s11695-019-04101-1
Santos J, et al. Effect of bariatric surgery on weight loss, inflammation, iron metabolism, and lipid profile. Scand J Surg. 2014;103:21–5. https://doi.org/10.1177/1457496913490467.
Acín GD, Baltar J. Capítulo 1: Conceptos básicos. Manual del VIII Curso On-line para Residentes: Iniciación a la Cirugía Bariátrica y Metabólica. (Editor: Asociación Española de Cirujanos, 2021).
Twig G, et al. White blood cell count and the risk for coronary artery disease in young adults. PLoS ONE. 2012;7:1–8. https://doi.org/10.1371/journal.pone.0047183.
Stepanova M, Rodriguez E, Birerdinc A, Baranova A. Age-independent rise of inflammatory scores may contribute to accelerated aging in multi-morbidity. Oncotarget. 2015;6:1414–21. https://doi.org/10.18632/oncotarget.2725.
Sabench F, et al. Criterios de calidad en cirugía bariátrica: revisión de conjunto y recomendaciones de la Asociación Española de Cirujanos y de la Sociedad Española de Cirugía de la Obesidad. Cir Esp. 2017;95:4–16. https://doi.org/10.1016/j.ciresp.2016.09.007.
Chiappetta S, Stier C, Weiner RA. The Edmonton Obesity Staging System predicts perioperative complications and procedure choice in obesity and metabolic surgery—a German Nationwide Register-Based Cohort Study (StuDoQ|MBE). Obes Surg. 2019;29:3791–9. https://doi.org/10.1007/s11695-019-04015-y.
Acknowledgements
Gregorio Vesperinas participated in collecting data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent to Participate
“For this type of study, formal consent is not required.”
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Low-grade inflammation associated to obesity
•Metabolically healthy severe obesity
• Metabolically unhealthy severe obesity
• Primary bariatric and metabolic surgery.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Recarte, M., Corripio, R., Palma, S. et al. Improvement of Low-Grade Inflammation in Patients with Metabolically Healthy Severe Obesity After Primary Bariatric Surgery. OBES SURG 33, 38–46 (2023). https://doi.org/10.1007/s11695-022-06345-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06345-w