Abstract
Introduction
Endoscopic sleeve gastroplasty (ESG) is a novel endoscopic bariatric therapy that complements current medical and surgical therapeutic offerings for weight management and fills an unmet need. Few meta-analyses compared ESG to laparoscopic sleeve gastrectomy (LSG). However, these studies relied on indirect evidence derived from non-comparative studies. Comparative effectiveness data derived from direct comparative studies is needed. We performed a meta-analysis of studies that directly compared ESG with LSG.
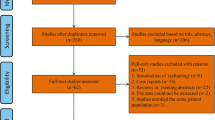
Methods
A comprehensive search of PubMed, Embase, and Cochrane databases was conducted. Single-arm studies were excluded. Pooled mean difference (MD) and risk ratio (RR) with 95% confidence intervals (CIs) were obtained within a random-effect model.
Results
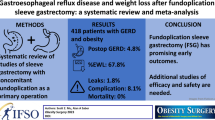
Seven studies with 6,775 patients (3,413 with ESG vs. 3,362 with LSG) were included. There were significant differences in 6-month (MD − 7.48; 95% CI − 10.44, − 4.52; P < 0.00001), 12-month (MD − 9.90; 95% CI − 10.59, − 9.22; P < 0.00001), and 24-month (MD − 7.63; 95% CI − 11.31, − 3.94; P < 0.0001) TBWL% favoring LSG over ESG. There was a trend toward lower incidence of adverse events with ESG compared to LSG but did not reach statistical significance (RR 0.51, 95% CI 0.23–1.11, P = 0.09). The incidence of new-onset gastroesophageal reflux disease (GERD) was significantly lower after ESG compared to LSG, 1.3% vs. 17.9%, respectively (RR 0.10, 95% CI 0.02–0.53, P = 0.006).
Conclusions
ESG achieved clinically adequate but lower short- and mid-term weight loss when compared to LSG, with fewer adverse events, including GERD. Given the stomach-sparing nature of ESG and acceptable safety profile, it provides an acceptable alternative to LSG for patients with mild-to-moderate obesity.
Graphical abstract





Similar content being viewed by others
References
Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012;31:219–30.
Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–7.
World Health Organization. Obesity and overweight. Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed December 6, 2019.
Pi-Sunyer X. The medical risks of obesity. Postgrad Med. 2009;121:21–33.
Cochrane AJ, Dick B, King NA, et al. Developing dimensions for a multicomponent multidisciplinary approach to obesity management: a qualitative study. BMC Public Health. 2017;17:814.
A pathway to endoscopic bariatric therapies. Surg Obes Relat Dis. 2011;7:672–82.
English WJ, DeMaria EJ, Brethauer SA, et al. American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis. 2018;14:259–63.
Kheirvari M, Dadkhah Nikroo N, Jaafarinejad H, et al. The advantages and disadvantages of sleeve gastrectomy; clinical laboratory to bedside review. Heliyon. 2020;6:e03496.
Qumseya BJ, Qumsiyeh Y, Ponniah SA, et al. Barrett’s esophagus after sleeve gastrectomy: a systematic review and meta-analysis. Gastrointest Endosc. 2021;93:343-352.e2.
Yeung KTD, Penney N, Ashrafian L, et al. Does sleeve gastrectomy expose the distal esophagus to severe reflux?: a systematic review and meta-analysis. Ann Surg. 2020;271:257–65.
Abu Dayyeh BK, Rajan E, Gostout CJ. Endoscopic sleeve gastroplasty: a potential endoscopic alternative to surgical sleeve gastrectomy for treatment of obesity. Gastrointest Endosc. 2013;78:530–5.
Abu Dayyeh BK, Acosta A, Camilleri M, et al. Endoscopic sleeve gastroplasty alters gastric physiology and induces loss of body weight in obese individuals. Clin Gastroenterol Hepatol. 2017;15:37-43.e1.
Alqahtani A, Al-Darwish A, Mahmoud AE, et al. Short-term outcomes of endoscopic sleeve gastroplasty in 1000 consecutive patients. Gastrointest Endosc. 2019;89:1132–8.
Fayad L, Adam A, Schweitzer M, et al. Endoscopic sleeve gastroplasty versus laparoscopic sleeve gastrectomy: a case-matched study. Gastrointest Endosc. 2019;89:782–8.
Hedjoudje A, Abu Dayyeh BK, Cheskin LJ, et al. Efficacy and safety of endoscopic sleeve gastroplasty: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2020;18:1043-1053.e4.
Mohan BP, Asokkumar R, Khan SR, et al. Outcomes of endoscopic sleeve gastroplasty; how does it compare to laparoscopic sleeve gastrectomy? A systematic review and meta-analysis. Endosc Int Open. 2020;8:E558–65.
Jalal MA, Cheng Q, Edye MB. Systematic review and meta-analysis of endoscopic sleeve gastroplasty with comparison to laparoscopic sleeve gastrectomy. Obes Surg. 2020;30:2754–62.
Marincola G, Gallo C, Hassan C, et al. Laparoscopic sleeve gastrectomy versus endoscopic sleeve gastroplasty: a systematic review and meta-analysis. Endosc Int Open. 2021;9:E87-e95.
Carr P, Keighley T, Petocz P, et al. Efficacy and safety of endoscopic sleeve gastroplasty and laparoscopic sleeve gastrectomy with 12+ months of adjuvant multidisciplinary support. BMC Prim Care. 2022;23:26.
Alqahtani AR, Elahmedi M, Aldarwish A, Abdurabu HY, Alqahtani S. Endoscopic gastroplasty versus laparoscopic sleeve gastrectomy: a noninferiority propensity score-matched comparative study. Gastrointest Endosc. 2022;96(1):44–50. https://doi.org/10.1016/j.gie.2022.02.050.
Lopez-Nava G, Asokkumar R, Bautista-Castaño I, et al. Endoscopic sleeve gastroplasty, laparoscopic sleeve gastrectomy, and laparoscopic greater curve plication: do they differ at 2 years? Endoscopy. 2021;53:235–43.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283:2008–12.
Luo D, Wan X, Liu J, et al. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27:1785–805.
Borenstein M, Hedges LV, Higgins JP, et al. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111.
Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Fiorillo C, Quero G, Vix M, et al. 6-Month gastrointestinal quality of life (QoL) results after endoscopic sleeve gastroplasty and laparoscopic sleeve gastrectomy: a propensity score analysis. Obes Surg. 2020;30:1944–51.
Lopez-Nava G, Negi A, Bautista-Castaño I, et al. Gut and metabolic hormones changes after endoscopic sleeve gastroplasty (ESG) vs. laparoscopic sleeve gastrectomy (LSG). Obes Surg. 2020;30:2642–51.
Novikov AA, Afaneh C, Saumoy M, et al. Endoscopic sleeve gastroplasty, laparoscopic sleeve gastrectomy, and laparoscopic band for weight loss: how do they compare? J Gastrointest Surg. 2018;22:267–73.
Sullivan S, Kumar N, Edmundowicz SA, et al. ASGE position statement on endoscopic bariatric therapies in clinical practice. Gastrointest Endosc. 2015;82:767–72.
Sinclair P, Brennan DJ, le Roux CW. Gut adaptation after metabolic surgery and its influences on the brain, liver and cancer. Nat Rev Gastroenterol Hepatol. 2018;15:606–24.
Khidir N, Al Dhaheri M, El Ansari W, et al. Outcomes of laparoscopic gastric greater curvature plication in morbidly obese patients. J Obes. 2017;2017:7989714–7989714.
Dayyeh BA, Rizk M, El-Mohsen MA, et al. Laparoscopic greater curvature plication (LGCP) vs. endoscopic sleeve gastroplasty (ESG): similar efficacy with different physiology. Surg Obes Relat Dis. 2017;13:S205.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study, formal consent is not required.
Conflict of Interest
Barham K. Abu Dayyeh: consulting for Endogenex, Endo-TAGSS, Metamodix, and BFKW; consultant and grant/research support from USGI, Spatz Medical, Boston Scientific; speaker roles with Olympus, Johnson and Johnson; speaker and grant/research support from Medtronic, Endogastric solutions; and research support from Apollo Endosurgery, Cairn Diagnostics, Aspire Bariatrics. All other authors (Azizullah Beran, Reem Matar, Veeravich Jaruvongvanich, Babusai B. Rapaka, Abdullah Alalwan, Ray Portela, and Omar Ghanem) do not have conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Compared to LSG, ESG achieved clinically adequate but lower short-term weight loss.
• The adverse events profile trended in favor of ESG with lower incidence of new-onset GERD in the ESG cohort.
• ESG is an acceptable minimally invasive option for poor surgical candidates or those pursuing alternative options to bariatric surgeries.
Supplementary Information
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 43.2 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Beran, A., Matar, R., Jaruvongvanich, V. et al. Comparative Effectiveness and Safety Between Endoscopic Sleeve Gastroplasty and Laparoscopic Sleeve Gastrectomy: a Meta-analysis of 6775 Individuals with Obesity. OBES SURG 32, 3504–3512 (2022). https://doi.org/10.1007/s11695-022-06254-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06254-y