Abstract
Purpose
Interest has grown regarding the impact of social media platforms on mental health including body image and internalized weight bias (IWB) in those who have struggled with weight issues. However, few studies have addressed social media usage in bariatric patient samples. The objective of this study was to understand how the amount of time spent on social media could serve as a predictor for IWB in both pre- and post-operative bariatric patients.
Materials and Methods
Pre- and post-operative patients at one academic medical center completed self-report measures assessing patients’ IWB, depression, anxiety, body dissatisfaction, sociodemographic variables, and social media usage. Data were collected from March 2019 to April 2020. Statistical methods that included correlations, logistical regression models, and ANOVA analysis were used to determine the relationship between time spent on social media and other covariates.
Results
A total of 148 responses were collected from the pre-surgical population, with 81 responses from the post-surgical sample. At baseline, the majority of respondents used social media for approximately 1 h per day (n = 37; 27.82%). Time spent on social media was negatively associated with age (r = − 0.24 [− 0.40, − 0.08]), and positively associated with IWB (r = 0.20 [0.02, 0.36]) and anxiety (r = 0.21 [0.01, 0.39]). In the post-operative group, only the 6-month BMI (r = 0.29 [0.05, 0.49]) was positively associated with time spent on social media.
Conclusion
Given this study’s findings, providers are encouraged to become aware of patients’ use of social media, and to understand the impact social media usage can have on the mental well-being of patients.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, bariatric surgery has provided the most effective and durable outcomes for successful weight loss [1]. However, psychological outcomes following bariatric surgery have been shown to vary significantly, with studies showing improvements in psychosocial quality of life only lasting for 2 years after the surgery, while others showing improvements in depression and mental health overall post-surgery[2, 3]. Factors contributing to bariatric patients’ psychosocial quality of life may include internalized weight bias (IWB), which refers to the belief that negative stereotypes about weight apply to oneself [4].
IWB is particularly concerning in the context of bariatric surgery as IWB has been negatively associated with weight loss following surgery [5], adherence to dietary and vitamin recommendations, and quality of life regarding mental health [6]. Additionally, IWB has been consistently correlated with significant body image disturbance, shape and weight concerns, and eating pathology, as well as depression in those with overweight including pre- and post-bariatric surgery patients [6,7,8,9].
Recently, there has been public interest in the use of social media platforms by those who may be experiencing mental health issues, as well as eating disorders, dysregulated eating, IWB, and poor body image. Social media platforms such as Facebook®, Twitter®, and Tumblr® allow users to interact with others’ content. Over the past decade, SM platforms have begun to focus primarily on sharing pictures or videos. Instagram®, Snapchat®, and TikTok® all have visual elements that involve users sharing pictures and videos that elicit comments from other users. Such media platforms change not only how people internalize appearance ideals, but also how they portray themselves online, and how they receive feedback from both friends and strangers about their appearance [10].
Platforms such as Instagram® allow users access to celebrities and models whose “perfect” body types are no longer restricted to movie screens and television. Users are able to view a plethora of body types, but most commonly, the body types that are “skinny” and “fit.” These selected photos on Instagram® are typically posted only after much scrutiny and perhaps even editing, as Instagram users tend to upload only their “best” and “perfect” photos, ones that would maximize attractiveness [11, 12]. Seeing such idealized images can lead to appearance comparisons, which have been shown to be linked to IWB and negative body image [5, 13, 14].
Despite the potential negative impact that social media can have on users, some evidence suggests there are beneficial applications of social media, particularly for those seeking to lose weight. Social media platforms may be helpful for those trying to lose weight, as these platforms connect like-minded individuals who encourage and support each other on their weight-loss journey. A study of the Weight Watchers Facebook® page found that the majority of members received both informational and emotional support through the site [15]. Robinson and colleagues conducted a literature review of eight studies of pre-operative bariatric patients’ use of online platforms. The authors used thematic analysis to develop five themes that emerged across studies including (1) managing expectations of a new life, (2) decision-making, (3) information seeking, (4) facilitating peer-to-peer connectedness and emotional support, and (5) enabling accessibility and connectivity with healthcare professionals. The authors called for further research on how best to design and moderate online forums for effectiveness and accuracy. Koball and colleagues conducted a content analysis of bariatric surgery support groups and pages on Facebook®, and found similar themes [16]. The authors suggested that providers should become familiar with the content found in these groups and recommend platforms with caution. While seeing healthy and fit persons may serve as motivation, for some patients these platforms may trigger negative comparisons, especially in those with IWB.
There is limited research regarding time spent using social media, and the association with mental health concerns. Much of the current research has focused on usage by adolescents and young adults, with mixed results regarding the impact of time spent on social media in terms of mental health [17]. Ferguson and colleagues studied social media use of 237 pre-adolescent girls and found that baseline use was positively associated with perceptions of peer competition [18]. These perceptions were positively associated with body dissatisfaction and eating disorder symptoms [18].
The objective of this study was to better understand how the amount of time spent on social media could serve as a predictor for internalized weight bias in pre- and post-surgical bariatric patients [19]. We hypothesized that greater time spent on social media would be associated with self-reported weight bias internalization. Additionally, we looked at social determinants of time spent on social media, including the relationship between social media usage and body mass index (BMI).
Methods
Participants and Procedures
Data for this analysis were obtained from voluntary self-report measures completed by pre-operative and post-operative patients participating in the Surgical Weight Loss Program at one academic medical center. Pre- and post-surgical assessments are delivered as a part of standard of care for patient evaluation prior to surgery and for those who ultimately undergo surgical intervention. The pre-surgical assessments were administered from March to November of 2019 while post-operative data was collected from March 2019 to April 2020 at around the 6-month post-operative time point for patients who underwent surgery. Criteria for patient evaluation into the program included a BMI of greater than or equal to 40 kg/m2, or greater than 35 kg/m2 along with a qualifying co-morbid condition such as diabetes or sleep apnea. Inclusion for analysis in this study included having received the use of a social media questionnaire during the pre-surgical assessments and being 18 years of age or older. Informed consent was obtained from all individual participants included in the study. This study was reviewed and approved by Penn State University’s institutional review board.
Measures
Weight Bias Internalization Scale
The Weight Bias Internalization Scale consists of 11 questions and assesses agreement with specific negative stereotypes among individuals who are overweight on a 7-point Likert scale [20]. This instrument is intended to measure the degree to which individuals with overweight or obesity internalize larger social stereotypes or biases related to obesity. Previous research evaluating the validity of this instrument in a bariatric sample has suggested the removal of the first item of the scale to improve internal consistency, leaving the instrument with a 10-item measure [8]. Thus, for the purposes of this research, item 1 was removed from the total average score.
Burns Anxiety Inventory
Patients were assessed for anxious symptoms using the Burns Anxiety Inventory (BAI), which is a survey consisting of 33 questions with 3 three subscales: anxious feelings, anxious thoughts, and physical symptoms [21]. After summing the scores from each item, the final score is utilized to evaluate the individual’s degree of anxiety. Final scores ranging from 0 to 4 translates to minimal or no anxiety; 5 to 10 is borderline anxiety; 11 to 20 is mild anxiety; 21 to 30 is moderate anxiety; 31 to 50 is severe anxiety; and finally, 51 to 99 is extreme anxiety or panic. The BAI has previously been used in research that has included patients seeking and following bariatric surgery [22,23,24]. In the current sample, the pre-operative BAI had a Cronbach’s alpha of 0.88 indicating high internal consistency.
Beck Depression Inventory-II
Patients were assessed for depressive symptoms using the Beck Depression Inventory-II (BDI-II), which is a 21-item instrument that measures depressive symptomatology [25]. Each item is rated on a 4-point scale, which can be totaled for a final score. Scores from 1 to 10 translates to normal feelings; 11 to 16 is mild mood disturbance; 17 to 20 is borderline clinical depression; 21 to 30 is moderate depression; 31 to 40 is severe depression; and finally, over 40 is extreme depression. The BDI-II has also previously been used in some studies that have included patients seeking and following bariatric surgery [22,23,24, 26]. In the current sample, the pre-operative BDI-II had a Cronbach’s alpha of 0.91 indicating high internal consistency.
Body Shape Questionnaire
Body image impairment was assessed using the Body Shape Questionnaire (BSQ-8C) [27]. The aim of this questionnaire is to evaluate the negative thoughts and feelings that individuals have in regard to their body shape or size. This instrument is an 8-item questionnaire that uses a 6-point Likert scale from “never” to “always.” In the current sample, the pre-operative BSQ-8C had a Cronbach’s alpha of 0.90 indicating high internal consistency.
Sociodemographic Variables
Our collected sociodemographic variables included age, sex, BMI, and education. Age and sex of the patient was collected at the time of the pre-surgical assessment. The patient’s BMI was collected at the time of surgery as well as at the 6-month post-surgical follow-up. The patient’s educational level was collected at the time of surgery and was categorized into three levels: high school or less, some or all of college, and graduate school.
Use of Social Media
A short 11-item questionnaire that was created by the study team. Respondents were asked if they used social media platforms such as Facebook®, Instagram®, Pinterest®, Snapchat®, and LinkedIn®, along with how often they checked these platforms and total time spent on social media daily. Questions also included what type of content respondents typically view, use of support groups via these platforms, and if the respondents compare themselves to the content they view in terms of appearance, weight, and/or body shape. A full copy of the questionnaire is provided in Supplement 1.
Statistical Analysis
Descriptive statistics were used to characterize the sample populations. Continuous variables are presented using means and standard deviations (SD) while categorical variables are presented in frequencies and percentages. Correlations between measures were calculated using Spearman correlation coefficients and 95% confidence limits. Logistical regression models were built to identify if any of the psychosocial health measures predicted total daily time spent on social media. Female sex was used as the reference group in the logistic regression models and continuous variables were standardized using the sample standard deviations. Differences in mean scores across different amounts of time spent on social media were assessed using ANOVA. Analyses were conducted on the pre- and post-surgical data as independent samples.
Results
In total, 257 pre-surgical patients were offered the social media questionnaire and 148 (57.59%) offered completed responses. Sample characteristics and instrument scores are presented in Table 1. Respondents had a mean (SD) age of 45.15 (12.23) with an average baseline BMI of 47.83 (8.74). The majority of respondents were female (n = 117; 79.05%), identified as White/Caucasian (n = 113; 76.35%), and nearly half had a high school degree or less (n = 69, 47.26%). Average depression scores were minimal with a mean (SD) score of 8.72 (8.52) and average anxiety scores were borderline with an average (SD) score of 10.35 (10.71). Both IWB and BSQ scores were elevated with mean scores of 4.10 (1.34) and 25.63 (8.89), respectively. In the post-surgical sample, 141 patients were sent invitations and 81 (57.45%) patients offered completed responses and had similar ages and baseline BMIs. Average (SD) 6-month BMI was 38.11 (7.73) for an average reduction of 9.71 (5.53). Additionally, all mental health and body image assessment scores were lower in the post-operative sample indicating improvement for these select metrics.
At baseline, the vast majority of respondents (n = 133; 89.86%) indicated that they used social media platforms with 37 (27.82%) using social media for approximately 1 h per day and 36 (27.07%) using social media for more than 2 h a day. One-quarter (n = 37) of the pre-surgical respondents indicated they use social media for food or recipe photos, videos, or posts with 32 (21.62%) engaging with or viewing weight-loss related accounts and another 29 (19.59%) engaging with or viewing bariatric surgery related accounts (Table 2).
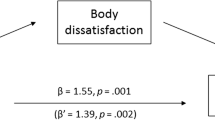
Baseline correlations between time spent on social media and the other variables are presented in Table 3. Between age, BMI, IWB, depression, anxiety, and body image, time spent on social media was significantly negatively associated with age (r = − 0.24 [− 0.40, − 0.08]), and positively associated with IWB (r = 0.20 [0.02, 0.36]) and anxiety (r = 0.21 [0.01, 0.39]). While these correlations were significant, the magnitude of these correlations was only fair. A base logistic regression model was built including age, sex, and BMI predicting time spent on social media. In this model, age was the only significant predictor with a protective odds ratio (OR) and 95% confidence limits of 0.67 [0.47, 0.95] (p = 0.03), indicating that those with younger age were more likely to spend more time on social media. IWB and anxiety were added to the base model. Within the expanded model, both age and IWB were significant predictors with OR [95% CL] of 0.58 [0.38, 0.89] and 1.79 [1.08, 2.97], respectively. With age being a significant predictor in both the base and expanded models, the distribution of age across the different levels of time spent on social media was evaluated (Fig. 1). This analysis showed a significant reduction in age as the level of time spent increased (p = 0.01).
Post-operatively, the baseline BMI was replaced with the 6-month BMI. Univariable correlations revealed that only 6-month BMI was significantly positively associated (r = 0.29 [0.05, 0.49]) with time spent on social media (Table 3). This fair correlation indicates that those with increased BMIs at the 6-month mark post-operatively were more likely to spend longer periods of time on social media. Unlike the pre-operative sample, age, IWB, and anxiety were no longer significantly correlated with time spent on social media. In the post-operative logistic regression model, age was no longer a significant predictor of time spent on social media while the patient’s 6-month BMI was predictive with an OR of 2.21 [1.33, 3.68] (Table 4), indicating again that those with higher BMIs were more likely to more time on social media.
Discussion
Only a few studies have examined the use of social media in bariatric populations [16, 28, 29]. The unique features of social media may allow bariatric patients to connect with others who can provide support for those who have struggled with obesity. In 1983, Benedict Anderson proposed the theory of “Imagined Communities” as groups of individuals connected by similar ideologies and sense of purpose to form socially constructed communities though they may never occupy the same physical space [30]. This particular construct can be applied to social media groups that have the ability to connect large numbers of individuals across the globe and can have a significant impact on the creation of self-identity [31].
While social media platforms can provide a safe forum for individuals to connect virtually, stigmatization of obesity in both social media videos and user comments occurs repeatedly [32]. The downside of social media includes the relationship between social media usage (particularly on forums such as Facebook®, YouTube®, and Instagram®) and body image dissatisfaction [33], which is associated with IWB [34]. Therefore, appearance comparisons resulting from social media use may play a role in body image concerns, as well as IWB.
Our findings that younger bariatric patients spent more time on social media is consistent with previous studies in non-bariatric populations that found a negative association between social media usage and age [35]. The Pew Research Center report on social media use in 2021 indicated that the majority of 18–29-year-olds reported using Instagram®, Snapchat®, and TikTok® in contrast with older groups [36]. In a study of public and personal social exposure to images of obesity, only personal exposure including normalization of beliefs that thinner body types are more attractive was associated with IWB[37]. The association between time on social media and IWB in our study suggests that bariatric patients who have adopted and internalized messages that a smaller body type is ideal may seek confirmation of these beliefs as well as comparisons of their body with peers on social media.
The secondary association between higher post-operative BMI and time on social media suggests that patients may be seeking comparison or confirmation of the pace and amount of weight loss in contrast to peers on social media, particularly if these patients have not reached a personal goal for weight loss, or if weight loss has slowed. Despite statistically significant weight loss, a portion of post-operative bariatric patients remain in the obese weight category with potential for a disparity between patient expectations for weight loss and the reality of the limits of surgery to achieve “thinness.” Consequently, patients may be using social media as a method to gauge their post-surgical progress and to seek reassurance and support for their continuing efforts.
Interestingly, while higher IWB scores were significantly associated with longer time spent on social media among pre-operative patients, there was a noticeable shift in scores post-operatively. Post-operatively, there was a near-significant negative (B: − 0.52; OR: 0.60 [0.35, 1.02]; p = 0.06) association with lower IWB scores and time spent on social media. This association suggests that those who experience higher feelings of IWB may utilize or engage with social media to a lesser degree following surgery. One possible explanation for this switch could be that those with higher perceptions of IWB may elect to avoid longer time spent on social media as to not experience poor mental health triggers.
Limitations
This study does present with a number of limitations including limited sample size and may be difficult to generalize to a larger sample or population. While the self-report evaluations were issued as a part of standard of care, they were still voluntary in nature and could be skipped per the desire of the patient. Additionally, due to the self-report nature of the study, there could be response bias resulting from impression management, which has been documented in other self-report evaluations of patients in a pre-surgical program [22]. Further, as the social media use questionnaire was only recently introduced into the pre-operative assessments, not all participants answered both the pre- and post-operative evaluation. Consequently, pre- and post-operative scores could not be linked. Additionally, there was a significant amount of loss to follow-up, which reduced the post-operative sample further. Moreover, a small portion (n = 14) of the post-operative responses were submitted during the COVID-19 pandemic. During the COVID-19 pandemic, social media usage trends may have shifted as quarantines restricted daily activity. Examination of #quarantine15 posts, referring to weight gain over the pandemic, suggests that increased social media usage may have further exposed those struggling with weight and obesity to negative content regarding weight gain, as well as perpetuation of the “thin ideal” frequently associated with IWB [38, 39]. In a study of adult usage of social media across four countries including the USA during the COVID-19 pandemic, increased daily time on social media was associated with poorer mental health [40]. While these trends may have only slightly impacted the results of this study, future research is needed to evaluate the extent to which the COVID-19 lockdowns impacted these associations. Lastly, as this study was cross-sectional in nature, the causal associations in the regression models could not be inferred.
Conclusion
Study findings suggest the need for bariatric provider awareness of patient social media use, especially in those with weight bias internalization. Providers may want to assess the role that social media may play in patient body image, and satisfaction with weight loss post-surgery. Interventions may include exploration of cognition and affect related to the use of social media, as well as behavioral interventions including setting time limits on usage. More research is needed in larger sample sizes as well as longitudinally to assess the overall impact of social media use by patients who have undergone weight loss surgery. Additional research is also needed regarding the efficacy of interventions for those patients whose social media usage may be detrimental to their mental health and overall satisfaction with surgical outcomes.
References
Sherman V. Bariatric surgery. Tex Heart Inst J. 2013;40(3):296.
Jumbe S, Bartlett C, Jumbe SL, et al. The effectiveness of bariatric surgery on long term psychosocial quality of life–a systematic review. Obes Res Clin Pract. 2016;10(3):225–42.
Mack I, Ölschläger S, Sauer H, et al. Does laparoscopic sleeve gastrectomy improve depression, stress and eating behaviour? A 4-year follow-up study. Obes Surg. 2016;26(12):2967–73.
Butt M, Wagner A, Rigby A. “I Thought That Being Thin Was Going to Solve All My Problems”: a qualitative study of body image in patients before and after bariatric surgery. Bariatr Surg Pract P. 2021;16(1):21–9.
Lent MR, Napolitano MA, Wood GC, et al. Internalized weight bias in weight-loss surgery patients: psychosocial correlates and weight loss outcomes. Obes Surg. 2014;24(12):2195–9.
Feig EH, Amonoo HL, Onyeaka HK, et al. Weight bias internalization and its association with health behaviour adherence after bariatric surgery. Clin Obes. 2020;10(4):e12361.
Durso LE, Latner JD, Ciao AC. Weight bias internalization in treatment-seeking overweight adults: psychometric validation and associations with self-esteem, body image, and mood symptoms. Eat Behav. 2016;21:104–8.
Wagner A, Butt M, Rigby A. Internalized weight bias in patients presenting for bariatric surgery. Eat Behav. 2020;39:101429.
Lawson JL, LeCates A, Ivezaj V, et al. Internalized weight bias and loss-of-control eating following bariatric surgery. Eat Disord. 2021;29(6):630–43.
Mills JS, Shannon A, Hogue J. Beauty, body image, and the media. Perception of beauty: IntechOpen; 2017. p. 145–57.
Chua THH, Chang L. Follow me and like my beautiful selfies: Singapore teenage girls’ engagement in self-presentation and peer comparison on social media. Comput Hum Behav. 2016;55:190–7.
Dumas TM, Maxwell-Smith M, Davis JP, et al. Lying or longing for likes? Narcissism, peer belonging, loneliness and normative versus deceptive like-seeking on Instagram in emerging adulthood. Comput Hum Behav. 2017;71:1–10.
Vartanian LR, Dey S. Self-concept clarity, thin-ideal internalization, and appearance-related social comparison as predictors of body dissatisfaction. Body Image. 2013;10(4):495–500.
Selensky JC, Carels RA. Weight stigma and media: an examination of the effect of advertising campaigns on weight bias, internalized weight bias, self-esteem, body image, and affect. Body Image. 2021;36:95–106.
Ballantine PW, Stephenson RJ. Help me, I’m fat! Social support in online weight loss networks. J Consum Behav. 2011;10(6):332–7.
Koball AM, Jester DJ, Domoff SE, et al. Examination of bariatric surgery Facebook support groups: a content analysis. Surg Obes Relat Dis. 2017;13(8):1369–75.
Schonning V, Hjetland GJ, Aaro LE, et al. Social media use and mental health and well-being among adolescents - a scoping review. Front Psychol. 2020;11:1949.
Ferguson CJ, Munoz ME, Garza A, et al. Concurrent and prospective analyses of peer, television and social media influences on body dissatisfaction, eating disorder symptoms and life satisfaction in adolescent girls. J Youth Adolesc. 2014;43(1):1–14.
Robinson A, Husband AK, Slight RD, et al. Digital support for patients undergoing bariatric surgery: narrative review of the roles and challenges of online forums. JMIR Perioper Med. 2020;3(2):e17230.
Durso LE, Latner JD. Understanding self-directed stigma: development of the weight bias internalization scale. Obesity. 2008;16(S2):S80–6.
Burns D. Feeling good handbook. Revised Edition ed. New York, NY: Plume; 1999.
Butt M, Wagner A, Rigby A. Associations of social desirability on psychological assessment outcomes for surgical weight loss patients. J Clin Psychol Med Settings. 2021;28(2):384–93.
Wagner AF, Butt M, Rigby A. Internalized weight bias in patients presenting for bariatric surgery. Eat Behav. 2020;39:101429.
Won EJ, Tran TT, Rigby A, et al. A comparative study of three-year weight loss and outcomes after laparoscopic gastric bypass in patients with “yellow light” psychological clearance. Obes Surg. 2014;24(7):1117–9.
Beck A, Steer R, Brown G. BDI-II: Beck Depression Inventory Manual. 2nd Edition ed. San Antonio, TX: Psychological Corporation; 1996.
Alabi F, Guilbert L, Villalobos G, et al. Depression before and after bariatric surgery in low-income patients: the utility of the Beck Depression Inventory. Obes Surg. 2018;28(11):3492–8.
Evans C, Dolan B. Body Shape Questionnaire: derivation of shortened “alternate forms.” Int J Eat Disord. 1993;13(3):315–21.
Koball AM, Jester DJ, Pruitt MA, et al. Content and accuracy of nutrition-related posts in bariatric surgery Facebook support groups. Surg Obes Relat Dis. 2018;14(12):1897–902.
Rammohan R, Dhanabalsamy N, Cheeyandira A, et al. Impact of social media on bariatric surgery. Surg Obes Relat Dis. 2016;12(7):S129–30.
Anderson B. Imagined communities: reflections on the origin and spread of nationalism. Revised edition ed: Verso; 2016.
Phillips T. Imagined communities and self-identity: an exploratory quantitative analysis. Sociology. 2002;36(3):597–617.
Hussin M, Frazier S, Thompson JK. Fat stigmatization on YouTube: a content analysis. Body Image. 2011;8(1):90–2.
Blowers LC, Loxton NJ, Grady-Flesser M, et al. The relationship between sociocultural pressure to be thin and body dissatisfaction in preadolescent girls. Eat Behav. 2003;4(3):229–44.
Carels R, Wott C, Young K, et al. Implicit, explicit, and internalized weight bias and psychosocial maladjustment among treatment-seeking adults. Eat Behav. 2010;11(3):180–5.
Chou W-YS, Hunt YM, Beckjord EB, et al. Social media use in the United States: implications for health communication. J Med Internet Res. 2009;11(4):e48.
Auxier B, Anderson M. Social media use in 2021. Pew Research Center. 2021. https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/. Accessed 2022 Mar 31
Stewart S-JF, Ogden J. The role of social exposure in predicting weight bias and weight bias internalisation: an international study. Int J Obes. 2021;45(6):1259–70.
Lucibello KM, Vani MF, Koulanova A, et al. #quarantine15: A content analysis of Instagram posts during COVID-19. Body Image. 2021;38:148–56.
Pearl RL. Weight stigma and the “Quarantine-15.” Obesity (Silver Spring). 2020;28(7):1180–1.
Thygesen H, Bonsaksen T, Schoultz M, et al. Social media use and its associations with mental health 9 months after the COVID-19 outbreak: a cross-national study. Front Public Health. 2021;9:752004.
Acknowledgements
We would like to thank Dr. Yaeeun “Joy” Lee for her contributions to this research.
Funding
Dr. Melissa Butt was supported in part by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $381,932 with 14% financed with non-governmental sources. Data collection for this research was supported by the Brad Hollinger Eating Disorders Research 22 Endowment at Penn State Health/Penn State College of Medicine Research Grant 2019–2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Considerations
This study was reviewed and approved by the institutional Human Research Protection Program. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Disclaimer
The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
•Social media (SM) connects patients seeking or having underwent bariatric surgery.
•Exposure to socially constructed beauty norms can negatively impact mental health.
•Post-operative 6-month body mass index was associated with time spent on SM.
•Providers must be aware of patients’ SM use and its impact on their mental health.
Previous Presentations
This work was presented at the 2021 American Psychological Association Convention.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Butt, M., Su, L. & Rigby, A. Associations of Use of Social Media and Psychopathology and Body Image in Pre- and Post-surgical Bariatric Samples: a Cross-sectional Analysis. OBES SURG 32, 3047–3055 (2022). https://doi.org/10.1007/s11695-022-06206-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06206-6