Abstract
Purpose
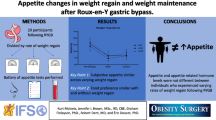
Suboptimal weight loss (SWL) and weight regain (WR) following bariatric surgery are common. The exact reasons for this phenomenon remain to be fully elucidated. To compare hedonic hunger, food preferences, food reward and eating behaviour traits between participants with SWL and optimal weight loss (OWL) 13 years after Roux-en-Y gastric bypass (RYGB).
Materials and Method
Cross-sectional case control study where participants experiencing SWL or OWL (< or ≥ 50% of excess weight, respectively) post-RYGB were compared to a non-surgical control group matched for pre-operative body mass index. Hedonic hunger (Power of Food Scale), implicit and explicit liking and wanting for high-fat and low-fat savoury and sweet food (Leeds Food Preference Questionnaire) and eating behaviour (Dutch Eating Behavior Questionnaire, Three-Factor Eating Questionnaire and the Food Cravings Questionnaires State and Trait-reduced) were assessed.
Results
In total, 75 participants were recruited from the bariatric surgery observation study (BAROBS). Disinhibition, hunger, emotional, external and restrained eating, frequency of cravings and hedonic hunger were lower in the OWL, compared with the SWL and/or control groups. Implicit wanting and explicit liking and wanting for high-fat savoury and high-fat sweet food were lower, and implicit wanting for low-fat savoury food higher, in the OWL, compared with the SWL and/or control groups.
Conclusion
SWL 13 years after RYGB is associated with dysfunctional eating behaviours, increased preference and reward for high-fat food and increased hedonic hunger. Future longitudinal studies are needed to establish the cause-effect relationship between these variables.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery is the most effective treatment for severe obesity [1,2,3], with a total weight loss (TWL) of approximately 40% at 2-year follow-up [4]. Roux-en-Y gastric bypass (RYGB) was, until recently, one of the most common bariatric procedures performed worldwide [5, 6]. Unfortunately, approximately 30% of patients experience suboptimal weight loss (SWL) and/or weight regain (WR) post-RYGB [7,8,9]. Significant WR is defined as ≥ 15% regain from nadir, and a longer interval after RYGB has been associated with weight regain (as been reported in 17% of the patients after 2-year follow-up) [10]. Unfortunately, a clear-cut definition of post-bariatric surgery WR and WL failure is missing [11, 12].
The mechanisms by which RYGB induces weight loss are not fully understood. However, the anatomical exclusion of the foregut, and subsequent upregulation of the secretion of glucagon-like peptide-1 and peptide YY, known to promote satiety and reduce food intake, is likely to be involved [13]. The aetiology of SWL and WR post-bariatric surgery remains to be fully elucidated [7, 14,15,16,17,18,19,20,21]. The available evidence suggests that hedonic hunger [22, 23], food preferences [18] and eating behaviour [17, 19] also modulate WL outcomes post-RYGB and might contribute to SWL and WR. Dysfunctional eating, defined as loss of control over eating, eating for emotional reasons, exerting strict control or eating without actually being hungry [24], is often seen in candidates for bariatric surgery [24, 25], and changes in this behaviour have been shown to modulate WL outcomes post-bariatric surgery [26]. RYGB is associated with an overall reduction in hedonic hunger and the drive to consume palatable foods [22, 23], and an increased desire for less energy dense foods [22, 27, 28]. More importantly, a positive association has been found between explicit liking for high-fat sweet (HFSW) food and WR post-RYGB [29].
Despite the evidence previously described, little is known regarding how inter-individual differences in hedonic hunger, food preferences and reward and eating behaviour post-RYGB contribute to SWL and WR in the long term. Therefore, the main aim of this study was to compare food preferences and reward, hedonic hunger and eating behaviour traits between participants with SWL and optimal WL (OWL) 13 years post-RYGB, and a non-surgical control group matched for the pre-operative body mass index (BMI) of the bariatric groups. A secondary aim was to explore the association between food preferences and reward, hedonic hunger and eating behaviour traits and percent of total WL (%TWL) and excess WL (%EWL) 13 years post-RYGB.
Materials and Method
Study Design
This is a cross-sectional case control study. Participants who had undergone RYGB between 2003 and 2009 (average 13 years earlier) were invited to participate in this study and were compared to a control group who had not undergone RYGB and presented with a similar pre-operative BMI. SWL was defined as < 50% of EWL and OWL as > 50% of EWL [30, 31]. The RYGB procedure was performed laparoscopically according to the Lönroth technique, with a pouch of 15–30 ml, biliopancreatic limb of 40–60 cm, antegastric, antecolic Roux limb of 100 cm if preoperative BMI ≤ 40 kg/m2, and 150 cm if preoperative BMI > 50 kg/m2, and linear stapled gastrojejunostomy and jejunojejunostomy. The mesenteric defects were not closed at that time [32]. The main indication for surgery in this population was weight loss.
Participants
Participants were recruited from the Bariatric Surgery Observation Study (BAROBS), a follow-up health survey in three local hospitals in the Central Norway Health Region. A total of 936 males and females were invited (28–75 years), operated between 2003 and 2009. The pre-operative control group included participants enrolled in the DISGAP-study (‘Effect of DIet versus Sleeve Gastrectomy and gastric bypass on APpetite’), who were on the waiting list for obesity treatment. Participants who had revisional bariatric surgery, eating disorders, were pregnant or breastfeeding, or were taking medications known to affect body weight or appetite (such as thyroid hormones and weight loss drugs) were excluded from the study.
Both the BAROBS and DISGAP studies were approved by the local ethics committee (REK 2017/1828-21and 2019/252, respectively). Additionally, the DISGAP study was registered in Clinical trials (NCT04051190). All participants provided written informed consent in line with the Helsinki Declaration, before entering the studies.
Measurements
All measurements were taken in average 13 years after surgery. Anthropometric measurements were taken in the fasting state (12 h), and after that participants answered the Leeds Food Preference Questionnaire (LFPQ) [33]. A liquid test meal was then offered, and participants asked to drink the shake over a 20-min period to avoid dumping symptoms. The test meal consisted of 200 ml of Diben shake (Fresenius Kabi, Fredrikstad, Norway) (Nutritional composition per 200 ml: 300 kcal, 15 g protein, 14 g fat and 26 g carbohydrates). Following this, participants answered the LFPQ again and filled out a battery of questionnaires. Detailed information about all measurements is described below.
Anthopometrics
Height was measured with a Seca 217 stadiometer (Seca, Hamburg, Germany) to the nearest 0.5 cm and weight was measured with a Seca 877 digital flat scale (Seca, Hamburg, Germany) to the nearest 0.1 kg. Body composition was assessed with air-displacement plethysmography (BodPod, Cosmed, Concord, CA, USA). The Brozeq equation was used to determine fat mass (FM) [34].
Pre-operative weight was the weight closest to the time of surgery. Ideal weight was the weight corresponding to a BMI of 25 kg/m2. %EWL, %WR and %TWL were estimated using standard equations [4, 12, 35].
Eating Behaviour
Eating behaviour traits were assessed after the test meal with four different questionnaires: Three-Factor Eating Questionnaire (TFEQ) [36], Dutch Eating Behavior Questionnaire (DEBQ) [37] and Food Cravings Questionnaires Trait-reduced and State (FCQ-T-r and FCQ-S) [38, 39]. TFEQ measures three different dimensions: restraint, disinhibition and hunger. TFEQ was developed for application in obesity research and has been found to be suitable in identifying subjects with eating behaviours that are associated with higher BMI [40, 41]. DEBQ measures cognitive restrained eating, external eating and emotional eating. Emotional eating can be divided into two sub-categories: diffuse emotions and clearly labelled emotions. FCQ-T-r measures frequency of cravings, while FCQ-S measures intensity of cravings [42]. The FCQ-S has been validated for use in both clinical and nonclinical populations [43, 44].
Hedonic Hunger
Power of Food Scale (PFS) was used to measure hedonic hunger in fed state. It has three different categories: food tasted, food present and food available, in addition to an aggregated score for all the categories combined [45]. PFS has been found to have good reliability for measuring hedonic hunger in both the general population and in individuals with obesity [45, 46].
Liking and Wanting for Food
LFPQ was used to measure ‘liking’ and ‘wanting’ for food, before and after the test meal [47]. Implicit measures of wanting and explicit measures of liking and wanting were measured by completing computer tasks lasting approximately 10 min. Food preference and food reward were assessed by pictures of common food items adjusted to the Norwegian diet. In addition, the pictures were modified when necessary (for participants with allergies and/or intolerances to the food pictures presented). The food pictures have two dimensions: fat (high or low) and taste (sweet or savoury) and can be divided into four categories: high fat savoury (HFSA), low fat savoury (LFSA), high fat sweet (HFSW) or low fat sweet (LFSW) [33]. LFPQ has been modified and adapted several times since it was created by Finlayson et al. (2007) [47, 48].
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics 26 (SPSS In., Chicago, IL, USA), and data presented as mean ± SEM, unless stated otherwise. Statistical significance was assumed at P < 0.05. Differences between groups (SWL, OWL and control) were assessed with one-way ANCOVA after adjusting for age and preoperative BMI. Bonferroni correction was used for multiple pairwise comparisons. Differences between groups for liking and wanting for food were assessed with Kruskal–Wallis followed by Mann–Whitney U-test, as these variables were not normally distributed. Correlation between scores from questionnaires and liking and wanting from LFPQ, and %EWL, %TWL and %WR, in the bariatric groups, was performed with Pearson or Spearman correlation, depending on the normality of the data.
Results
Participants’ characteristics are reported in Table 1. Seventy-five participants (79% women) participated in this study, 25 participants in each group, with a similar sex distribution. The control group was younger than both the SWL and OWL groups (P < 0.01 and P < 0.05, respectively). The OWL group had a lower BMI, weight and %FM compared with both the SWL and control groups (P < 0.01 for all). There were no significant differences in BMI between the SWL group and control group. Despite no significant differences in pre-operative BMI between the control and the bariatric groups combined, the SWL group presented with a higher preoperative BMI compared with both control and OWL groups (P < 0.01). The SWL group also presented with higher nadir weight, and %WR (P < 0.01 for both) and lower %TWL and %EWL (P < 0.01 for both) compared with the OWL group. Nineteen participants (76%) in the SWL group also had > 15% WR. Only two (8%) participants in each group (SWL and OWL) were on medication for type 2 diabetes.
Results for eating behaviour traits are presented in Table 2. The OWL group presented with a lower score for disinhibition and hunger (TFEQ) compared with both the SWL and control groups (P < 0.01 for all). Dietary restraint score was also lower in the OWL compared with the control group (P < 0.05). Emotional eating, external eating and diffuse and clearly labelled emotions from DEBQ were lower in the OWL compared with both the SWL and control groups (P < 0.05 and P < 0.01). Restrained eating from DEBQ was also lower in the OWL compared with the control group only (P < 0.01). Frequency of cravings (FCQ-T-r) was higher in the SWL and control groups compared with the OWL group (P < 0.01 for both), but there were no differences among groups for intensity of cravings (FCQ-S). Significant differences among groups were seen in all four categories of PFS. Aggregated score, food present and food available were lower in the OWL group compared with both the SWL (P < 0.05) and control groups (P < 0.01). The score for food tasted was also lower in the OWL compared with the control group only (P < 0.05).
Liking and wanting for food in the different study groups are shown in Table 3. The OWL group presented with a lower implicit wanting for HFSA and HFSW food, in both fasting and fed states, compared to the control group (P < 0.05 for all). It also presented with higher implicit wanting for LFSA food, in both fasting and fed states, compared with the control group and in fed state also compared with the SWL group (P < 0.05 for both). The OWL group also had a lower explicit liking and wanting for HFSA food, both in the fasting and fed state, compared to the control group (P < 0.05 and P < 0.01) and for HFSW food compared with both the SWL (P < 0.05) and control (P < 0.01) groups.
Correlation Analysis
A moderate inverse association was found between %TWL and %EWL (and positive association with %WR) and the following variables: disinhibition and hunger (TFEQ), emotional eating, diffuse emotions and clearly labelled emotions (DEBQ), frequency of cravings (FCQ-T-r), and food available, food present and aggregated score (PFS). Moreover, a weak inverse correlation was found between external eating from DEBQ and %EWL (see Table 4). Additionally, the higher the implicit wanting for LFSA in fasting, the larger the %EWL and %TWL. A weak inverse association was also found between explicit liking and wanting for HFSW food in the fasting state and %TWL and %EWL (see Supplementary table 1).
Discussion
The present study aimed to compare eating behaviour traits, hedonic hunger, food preferences and reward between participants with SWL and OWL 13 years post-RYGB, in addition to a non-surgical group control, matched for pre-operative BMI. The results indicate a more dysfunctional eating behaviour in both the SWL and control groups compared with the OWL group. More specifically a higher disinhibition and hunger, emotional eating and its subcategories, external eating, a higher frequency of cravings and a higher hedonic hunger was seen in the SWL and control groups, compared with the OWL group. Higher scores in these eating behaviour variables were also associated with lower %EWL and %TWL, and a larger %WR. Interestingly, no differences were seen between the SWL and the control group regarding eating behaviour traits or hedonic hunger. The SWL group also presented with a higher explicit liking and wanting for HFSW foods compared with the OWL group. The OWL group had a lower explicit liking and wanting, and implicit wanting for HFSA and HFSW foods compared with control. In addition, the OWL group had a higher implicit wanting for LFSA food compared with controls, both in fasting and fed states, and compared with the SWL group in the fed state.
In the present study, a lower disinhibition and hunger were found in the OWL compared with the SWL group and these variables were inversely associated with %EWL. These findings are in line with those from Amundsen et al. who found a higher degree of disinhibition in those experiencing SWL 5 years after RYGB [16]. Another study by Konttinen et al. found that WL post-bariatric surgery was predicted by low levels of disinhibition and hunger, assessed with TFEQ, at different time points after surgery, and that those with lower levels shortly after surgery had greater WL after 10 years [49].
Higher levels of emotional eating were also found in the SWL group in the present analysis. This is in line with a recent study where higher levels of emotional eating were found to be associated with higher WR and less WL 4 years after RYGB [19]. However, Amundsen et al. found no differences in emotional eating between SWL and OWL groups 4 years post-surgery [16]. Another study found that women with a higher degree of emotional eating had, in fact, more successful WL 8 years post-surgery [50]. However, only 15% of the patients had RYGB. Therefore, differences in follow-up time may explain the divergent results.
Both the SWL and control groups presented with significantly higher frequency of cravings, compared with the OWL group. Food cravings, in particular preoccupations with food, are common in bariatric surgery candidates [51] and those with higher scores on the subscale ‘guilt from cravings’ have been shown to experience less WL post-bariatric surgery [52].
The present study showed that higher hedonic hunger was associated with less TWL and EWL and that the SWL group had significant higher scores than the OWL group in most categories. The domains ‘food available’ and ‘food present’ have been shown to be inversely associated with percentage excess BMI loss post-gastric bypass, in a cross-sectional analysis [23]. Moreover, Ullrich et al., using a longitudinal design, reported a marked reduction in hedonic hunger aggregated scores, as well as the subdomains ‘food available’ and ‘food tasted’ post-surgery, and absolute WL was inversely associated with ‘food tasted’ score [22]. Differences in study designs, methods of assessing eating behaviour and time between surgery and follow-up assessments could explain some of the differences among studies.
In the present analysis, implicit wanting and explicit liking and wanting for HFSA and HFSW food were lower, and implicit wanting for LFSA food higher, in the OWL group, compared with the SWL and/or control groups. Less liking for sweet foods has previously been shown to be associated with a larger WL post-bariatric surgery in women [53]. The majority of the evidence shows that RYGB reduces hedonic hunger and changes food preferences towards foods low in fat and sugar [22, 23, 27, 54, 55]. It is therefore possible that a portfolio of dysregulated eating behaviours leads to increased preference for high-fat food, putting some individuals at risk of overeating and SWL following bariatric surgery. On the other hand, Søndergaard et al. reported that bariatric surgery did not change food preferences, but that altered food preferences were predictive of WL [28]. However, food preferences were measured with an ad libitum buffet. Even though food preferences may predict WL, WL has also been shown to alter food preferences [56]. Further research is needed to ascertain the direction of causality.
This study presents with both strengths and limitations. First, participants had RYGB 13 years earlier, and, therefore, our findings are likely to represent long-term results. Second, the study had a control group, allowing for comparisons with a group that resembles pre-operative conditions. Third, the food pictures shown in the LFPQ were adapted to the Norwegian diet [33]. Lastly, TFEQ was developed for obesity research, and both the TFEQ and the PFS have been validated in individuals with obesity [41, 45, 46, 57]. The main limitation of this study is its cross-sectional design and, as such, no inference of causality can be done. Also, the sex distribution was skewed with very few men, preventing the generalisation of the results to the whole bariatric population. Even though we aimed to have a non-bariatric control group matched for the pre-surgical BMI of the bariatric groups, the control group had a significantly lower BMI compared with the SWL (but not the OWL) group. However, we adjusted for pre-operative BMI in our analysis, so this difference is unlikely to have affected the results. Finally, EWL % was used to define the SWL and OWL groups.
There are many possible mechanisms not discussed in this paper that can be associated with WL failure and WR post-bariatric surgery, namely gut microbiota [58]. Nevertheless, RYGB is thought to promote WL mainly by reducing appetite, likely due to exaggerated release of satiety hormones, particularly glucagon-like peptide Y (GLP-1), and to a lower extent also peptide YY (PYY) in the post-prandial period [59]. It has been proposed that SWL and WR following RYGB can be a result of a blunted release of satiety peptides, but results are inconsistent and long-term results are lacking [60, 61]. In addition, behavioural, dietary, psychological and medical factors can all play a role in long-term WL following bariatric surgery [11, 62]. The use of GLP-1 analogues, as a weight loss aid, in patients with SWL or WR post-bariatric surgery has started to be investigated with promising results [63].
Successful WL maintenance in the long-term remains the biggest challenge in obesity management, also after bariatric surgery [8, 9]. In the present study, the SWL group was more comparable to the non-surgical control group in most variables, suggesting that SWL could be a result of dysfunctional eating behaviours. However, due the cross-sectional nature of this study, it cannot be ascertained if this is a cause or a consequence of SWL and/or WR post-RYGB. If dysfunctional eating behaviours are found to be the cause of SWL and WR in longitudinal studies, then pre-operative screening for eating behaviour, food preferences and hedonic hunger should be recommended [64, 65], as well as long-term follow-ups aiming at improving these behaviours in order to ensure progressive WL and prevent weight regain [66].
In conclusion, SWL 13 years after RYGB is associated with dysfunctional eating behaviours, greater liking and wanting for high-fat food and greater hedonic hunger. Future longitudinal studies are needed to clarify the direction of causality.
References
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Shin AC, Berthoud HR. Food reward functions as affected by obesity and bariatric surgery. Int J Obes. 2005;2011(35 Suppl 3):S40–4.
Nance K, Acevedo MB, Pepino MY. Changes in taste function and ingestive behavior following bariatric surgery. Appetite. 2020;146:104423.
King WC, Hinerman AS, Belle SH, et al. Comparison of the performance of common measures of weight regain after bariatric surgery for association with clinical outcomes. JAMA. 2018;320(15):1560–9.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427–36.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–32.
Lutfi R, Torquati A, Sekhar N, et al. Predictors of success after laparoscopic gastric bypass: a multivariate analysis of socioeconomic factors. Surg Endosc. 2006;20(6):864–7.
Higa K, Ho T, Tercero F, et al. Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis. 2011;7(4):516–25.
Magro DO, Geloneze B, Delfini R, et al. Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg. 2008;18(6):648–51.
Shantavasinkul PC, Omotosho P, Corsino L, et al. Predictors of weight regain in patients who underwent Roux-en-Y gastric bypass surgery. Surg Obes Relat Dis. 2016;12(9):1640–5.
Karmali S, Brar B, Shi X, et al. Weight recidivism post-bariatric surgery: a systematic review. Obes Surg. 2013;23(11):1922–33.
Athanasiadis DI, Martin A, Kapsampelis P, et al. Factors associated with weight regain post-bariatric surgery: a systematic review. Surg Endosc. 2021;35(8):4069–84.
Ochner CN, Gibson C, Shanik M, et al. Changes in neurohormonal gut peptides following bariatric surgery. Int J Obes. 2011;35(2):153–66.
Nickel F, de la Garza JR, Werthmann FS, et al. Predictors of risk and success of obesity surgery. Obes Facts. 2019;12(4):427–39.
Homan J, Boerboom A, Aarts E, et al. A longer biliopancreatic limb in Roux-en-Y gastric bypass improves weight loss in the first years after surgery: results of a randomized controlled trial. Obes Surg. 2018;28(12):3744–55.
Amundsen T, Strømmen M, Martins C. Suboptimal weight loss and weight regain after gastric bypass surgery-postoperative status of energy intake, eating behavior, physical activity, and psychometrics. Obes Surg. 2017;27(5):1316–23.
Novelli IR, Fonseca LG, Gomes DL, et al. Emotional eating behavior hinders body weight loss in women after Roux-en-Y gastric bypass surgery. Nutrition. 2018;49:13–6.
Husted M, Ogden J. Emphasising personal investment effects weight loss and hedonic thoughts about food after obesity surgery. J Obes. 2014;2014:810374.
Monpellier VM, Janssen IMC, Antoniou EE, et al. Weight change after Roux-en Y gastric bypass, physical activity and eating style: is there a relationship? Obes Surg. 2019;29(2):526–33.
Sweeney TE, Morton JM. Metabolic surgery: action via hormonal milieu changes, changes in bile acids or gut microbiota? A summary of the literature. Best Pract Res Clin Gastroenterol. 2014;28(4):727–40.
Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg. 2012;22(1):70–89.
Ullrich J, Ernst B, Wilms B, et al. Roux-en Y gastric bypass surgery reduces hedonic hunger and improves dietary habits in severely obese subjects. Obes Surg. 2013;23(1):50–5.
Schultes B, Ernst B, Wilms B, et al. Hedonic hunger is increased in severely obese patients and is reduced after gastric bypass surgery. Am J Clin Nutr. 2010;92(2):277–83.
Gade H, Friborg O, Rosenvinge JH, et al. The impact of a preoperative cognitive behavioural therapy (CBT) on dysfunctional eating behaviours, affective symptoms and body weight 1 year after bariatric surgery: a randomised controlled trial. Obes Surg. 2015;25(11):2112–9.
Zimmerman M, Francione-Witt C, Chelminski I, et al. Presurgical psychiatric evaluations of candidates for bariatric surgery, part 1: reliability and reasons for and frequency of exclusion. J Clin Psychiatry. 2007;68(10):1557–62.
Alshus, Ingvild Austad. Spiseatferd og psykisk helse hos fedmekirurgipasienter.En prospektiv studie av forekomst og påvirkning av problematisk spiseatferd samt angst- og depresjonssymptomer før og etter fedmeoperasjon. Master thesis, University of Oslo, 2018. http://hdl.handle.net/10852/62465.
le Roux CW, Bueter M. The physiology of altered eating behaviour after Roux-en-Y gastric bypass. Exp Physiol. 2014;99(9):1128–32.
Søndergaard Nielsen M, Rasmussen S, Just Christensen B, et al. Bariatric surgery does not affect food preferences, but individual changes in food preferences may predict weight loss. Obesity. 2018;26(12):1879–87.
Brown J. Relationship of appetite, olfaction and food reward after Roux-en-y gastric bypass surgery: could this explain weight regain? (Doctoral dissertation). Université d’Ottawa/University of Ottawa; 2015.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25(4):587–606.
Zalesin KC, Franklin BA, Miller WM, et al. Preventing weight regain after bariatric surgery: an overview of lifestyle and psychosocial modulators. AJLM. 2010;4(2):113–20.
Olbers T, Lönroth H, Fagevik-Olsén M, et al. Laparoscopic gastric bypass: development of technique, respiratory function, and long-term outcome. Obes Surg. 2003;13(3):364–70.
Oustric P, Thivel D, Dalton M, et al. Measuring food preference and reward: application and cross-cultural adaptation of the Leeds Food Preference Questionnaire in human experimental research. Food Qual Prefer. 2020;80:103824.
Ginde SR, Geliebter A, Rubiano F, et al. Air displacement plethysmography: validation in overweight and obese subjects. Obes Res. 2005;13(7):1232–7.
Corcelles R, Boules M, Froylich D, et al. Total weight loss as the outcome measure of choice after Roux-en-Y gastric bypass. Obes Surg. 2016;26(8):1794–8.
Stunkard AJ, Messick S. The Three-Factor Eating Questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71–83.
Brunault P, Rabemampianina I, Apfeldorfer G, et al. The Dutch Eating Behavior Questionnaire: further psychometric validation and clinical implications of the French version in normal weight and obese persons. Presse Med. 2015;44(12 Pt 1):e363–72.
Nijs IM, Franken IH, Muris P. The modified Trait and State Food-Cravings Questionnaires: development and validation of a general index of food craving. Appetite. 2007;49(1):38–46.
Meule A, Hermann T, Kubler A. A short version of the Food Cravings Questionnaire-Trait: the FCQ-T-reduced. Front Psychol. 2014;5:190.
Löffler A, Luck T, Then FS, et al. Eating behaviour in the general population: an analysis of the factor structure of the German version of the Three-Factor-Eating-Questionnaire (TFEQ) and its association with the body mass index. PLoS One. 2015;10(7):0133977.
Karlsson J, Persson LO, Sjöström L, et al. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish obese subjects (SOS) study. Int J Obes Relat Metab Disord. 2000;24(12):1715–25.
Meule A, Heckel D, Jurowich C, et al. Correlates of food addiction in obese individuals seeking bariatric surgery. Clin Obes. 2014;4(4):228–36.
Cepeda-Benito A, Gleaves DH, Williams TL, et al. The development and validation of the State and Trait Food-Cravings Questionnaires. Behav Ther. 2000;31(1):151–73.
Cepeda-Benito A, Gleaves DH, Fernandez MC, et al. The development and validation of Spanish versions of the State and Trait Food Cravings Questionnaires. Behav Res Ther. 2000;38(11):1125–38.
Cappelleri JC, Bushmakin AG, Gerber RA, et al. Evaluating the Power of Food Scale in obese subjects and a general sample of individuals: development and measurement properties. Int J Obes (Lond). 2009;33(8):913–22.
Andreeva E, Neumann M, Nöhre M, et al. Validation of the German version of the Power of Food Scale in a general population sample. Obes Facts. 2019;12(4):416–26.
Finlayson G, King N, Blundell JE. Is it possible to dissociate ‘liking’ and ‘wanting’ for foods in humans? A novel experimental procedure. Physiol Behav. 2007;90(1):36–42.
Charlot K, Malgoyre A, Bourrilhon C. Proposition for a shortened version of the Leeds Food Preference Questionnaire (LFPQ). Physiol Behav. 2019;199:244–51.
Konttinen H, Peltonen M, Sjostrom L, et al. Psychological aspects of eating behavior as predictors of 10-y weight changes after surgical and conventional treatment of severe obesity: results from the Swedish obese subjects intervention study. Am J Clin Nutr. 2015;101(1):16–24.
Mathus-Vliegen EM. Long-term health and psychosocial outcomes from surgically induced weight loss: results obtained in patients not attending protocolled follow-up visits. Int J Obes. 2007;31(2):299–307.
Crowley N, Madan A, Wedin S, et al. Food cravings among bariatric surgery candidates. Eat Weight Disord. 2014;19(3):371–6.
Crowley NM, LePage ML, Goldman RL, et al. The Food Craving Questionnaire-Trait in a bariatric surgery seeking population and ability to predict post-surgery weight loss at six months. Eat Behav. 2012;13(4):366–70.
Hubert PA, Papasavas P, Stone A, et al. Associations between weight loss, food likes, dietary behaviors, and chemosensory function in bariatric surgery: a case-control analysis in women. Nutrients. 2019;11(4):804.
Hansen TT, Jakobsen TA, Nielsen MS, et al. Hedonic changes in food choices following Roux-en-Y gastric bypass. Obes Surg. 2016;26(8):1946–55.
Guyot E, Dougkas A, Nazare J-A, et al. A systematic review and meta-analyses of food preference modifications after bariatric surgery. Obes Rev. 2021;22(10):e13315
Grafenauer SJ, Tapsell LC, Beck EJ, et al. Changes in food choice patterns in a weight loss intervention. Nutr Diet. 2015;72(4):309–15.
Löffler A, Luck T, Then FS, et al. Eating behaviour in the general population: an analysis of the factor structure of the German version of the Three-Factor-Eating-Questionnaire (TFEQ) and its association with the body mass index. PLoS ONE. 2015;10(7):e0133977.
Ejtahed HS, Angoorani P, Hasani-Ranjbar S, et al. Adaptation of human gut microbiota to bariatric surgeries in morbidly obese patients: a systematic review. Microb Pathog. 2018;116:13–21.
Schmidt JB, Pedersen SD, Gregersen NT, et al. Effects of RYGB on energy expenditure, appetite and glycaemic control: a randomized controlled clinical trial. Int J Obes (Lond). 2016;40(2):281–90.
Santo MA, Riccioppo D, Pajecki D, et al. Weight regain after gastric bypass: influence of gut hormones. Obes Surg. 2016;26(5):919–25.
le Roux CW, Welbourn R, Werling M, et al. Gut hormones as mediators of appetite and weigth loss after Roux-en-Y gastric bypass. Ann Surg. 2007;246(5):780–5.
McGrice M, Don PK. Interventions to improve long-term weight loss in patients following bariatric surgery: challenges and solutions. Diabetes Metab Syndr Obes Targets Ther. 2015;8:263–74.
Horber FF, Steffen R. Reversal of long-term weight regain after Roux-en-Y gastric bypass using liraglutide or surgical revision. A Prospective Study. Obes Surg. 2021;31(1):93–100.
Sarwer DB, Allison KC, Wadden TA, et al. Psychopathology, disordered eating, and impulsivity as predictors of outcomes of bariatric surgery. Surg Obes Relat Dis. 2019;15(4):650–5.
Sogg S, Lauretti J, West-Smith L. Recommendations for the presurgical psychosocial evaluation of bariatric surgery patients. Surg Obes Relat Dis. 2016;12(4):731–49.
Coulman KD, MacKichan F, Blazeby JM, et al. Patient experiences of outcomes of bariatric surgery: a systematic review and qualitative synthesis. Obes Rev. 2017;18(5):547–59.
Acknowledgements
We would like to thank all participants for their time and commitment, and the staff at the obesity out-patient clinics for invaluable effort in data collection. Turid Follestad for help with statistical analysis at the Department of Clinical and Molecular Medicine, NTNU.
Funding
Open access funding provided by NTNU Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital). This study was supported by a postdoctoral grant funded by the Liaison Committee for education, research and innovation in Central Norway and Nord-Trøndelag Hospital Trust, Norway.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Sub-optimal weight loss (SWL) is associated with dysfunctional eating behaviours.
• Increased preference and reward for high-fat food.
• Increased hedonic hunger.
• Longitudinal studies are needed to ascertain direction of causality between dysfunctional eating behaviours and SWL.
Siren Nymo and Oda Børresen Skjølsvold shared first authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nymo, S., Børresen Skjølsvold, O., Aukan, M. et al. Suboptimal Weight Loss 13 Years After Roux-en-Y Gastric Bypass: Is Hedonic Hunger, Eating Behaviour and Food Reward to Blame?. OBES SURG 32, 2263–2271 (2022). https://doi.org/10.1007/s11695-022-06075-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06075-z