Abstract
Background
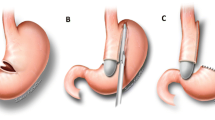
Sleeve gastrectomy (SG) has become one of the most performed bariatric procedures worldwide. Its main weaknesses are weight regain and gastroesophageal reflux disease (GERD). Conversion to Roux-en-Y gastric bypass (RYGB) is considered the gold standard to manage GERD and related symptoms.
Methods
Retrospective evaluation from a prospective bariatric surgery database of all our institution’s patients converted from SG to RYGB due to GERD between January 2010 and December 2018. Clinical characteristics and workups before SG and before and after RYGB were analyzed.
Results
During the study period, 35 patients needed a conversion to RYGB, due to GERD or GERD-related symptoms. Mean age was 48.6 years, 85.7% were women, and mean BMI was 31.4 kg/m2. The interval between SG and RYGB was in a range 7 to 70 months (mean 33 months). All conversions were completed laparoscopically, associating a hiatoplasty in 45.7% of cases. A complete remission of symptoms was observed in 74% of patients, some improvement in 20%, and no relief in 6%. There were 3 cases of hiatal hernia persistence and 2 of recidivism. Only 1 patient presented pathological pHmetry, while moderate esophagitis was demonstrated in 2 patients.
Conclusions
Conversion to RYGB was effective in almost all patients. Pathological acid exposure and hiatal hernias seem to be the main findings prior to conversion, justifying an exhaustive examination and aggressive approach to the hiatus. Due to the insufficient correlation between symptoms and findings on morphological and functional tests, actively searching for signs of GERD is advisable.
Graphical abstract



Similar content being viewed by others
References
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the Fourth IFSO Global Registry Report 2018. Obes Surg, Springer New York LLC. 2019;29:782–95.
Ali M, El Chaar M, Ghiassi S, et al. American Society for Metabolic and Bariatric Surgery updated position statement on sleeve gastrectomy as a bariatric procedure. Surg Obes Relat Dis. 2017;13:1652–7.
Landreneau JP, Strong AT, Rodriguez JH, et al. Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass. Obes Surg. 2018;28:3843–50.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Annals of surgery. 2010;252:319–24.
Braghetto I, Csendes A. Prevalence of Barrett’s Esophagus in Bariatric Patients Undergoing Sleeve Gastrectomy. Obesity surgery. 2016;26:710–4.
Genco A, Soricelli E, Casella G, et al. Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg Obes Relat Dis. 2017;13:568–74.
Lucas Guerrero V, Luna A, Rebasa P, Montmany S, Navarro S. Degeneration of Barrett’s esophagus after sleeve gastrectomy. Cir Esp. Elsevier Doyma; 2020
Sebastianelli L, Benois M, Vanbiervliet G, et al. Systematic endoscopy 5 years after sleeve gastrectomy results in a high rate of Barrett’s esophagus: results of a multicenter study. Obes Surg. 2019;29:1462–9.
Soricelli E, Casella G, Baglio G, Maselli R, Ernesti I, Genco A. Lack of correlation between gastroesophageal reflux disease symptoms and esophageal lesions after sleeve gastrectomy. Surgery for obesity and related diseases. 2018;14:751–6.
Parmar CD, Mahawar KK, Boyle M, Schroeder N, Balupuri S, Small PK. Conversion of Sleeve Gastrectomy to Roux-en-Y Gastric Bypass is Effective for Gastro-Oesophageal Reflux Disease but not for Further Weight Loss. Obesity Surgery. 2017;27:1651–8.
Felsenreich DM, Langer FB, Bichler C, Eilenberg M, Jedamzik J, Kristo I, et al. Roux-en-Y Gastric Bypass as a Treatment for Barrett’s Esophagus after Sleeve Gastrectomy. Obesity Surgery. 2020;30:1273–9.
Braghetto I, Csendes A, Korn O, Valladares H, Gonzalez P, Henríquez A. Gastroesophageal Reflux Disease After Sleeve Gastrectomy. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques. 2010;20:148–53.
Barajas-Gamboa JS, Landreneau J, Abril C, et al. Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass for complications: outcomes from a tertiary referral center in the Middle East. Surg Obes Relat Dis. Elsevier Inc. 2019;15:1690–5. https://doi.org/10.1016/j.soard.2019.07.027.
Vilallonga R, Hidalgo M, Garcia Ruiz de Gordejuela A, Caubet E, Gonzalez O, Ciudin A, et al. Operative and Postoperative Complications of Laparoscopic Sleeve Gastrectomy in Super and Nonsuper Obese Patients: A Center of Excellence Experience Comparative Study. Journal of Laparoendoscopic & Advanced Surgical Techniques [Internet]. 2020;30:501–7
Gyawali CP, Kahrilas PJ, Savarino E, Zerbib F, Mion F, Smout AJPMPM, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. BMJ Publishing Group; 2018;67:1351–62.
Akil N, van Zanten S, Kahrilas P, Dent J, Jones R. Die Montreal-Definition und -Klassifikation der gastroösophagealen Refluxkrankheit: Ein globales evidenzbasiertes Konsensus-Papier. Zeitschrift für Gastroenterologie. 2007;45:1125–40.
Carandina S, Soprani A, Montana L, Murcia S, Valenti A, Danan M, et al. Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass in patients with gastroesophageal reflux disease: results of a multicenter study. Surg Obes Relat Dis. 2020;1–6.
Poghosyan T, Lazzati A, Moszkowicz D, et al. Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass: an audit of 34 patients. Surg Obes Relat Dis. 2016;12:1646–51.
Yeung KTD, Penney N, Ashrafian L, Darzi A, Ashrafian H. Does Sleeve Gastrectomy Expose the Distal Esophagus to Severe Reflux? Annals of Surgery. 2020;271:257–65.
Felsenreich DM, Kefurt R, Schermann M, et al. Reflux, sleeve dilation, and Barrett’s esophagus after laparoscopic sleeve gastrectomy: long-term follow-up. Obes Surg Obes Surg. 2017;27:3092–101.
Sucandy I, Chrestiana D, Bonanni F, Antanavicius G. Gastroesophageal reflux symptoms after laparoscopic sleeve gastrectomy for morbid obesity. The importance of preoperative evaluation and selection. N Am J Med Sci. 2015;7:189–93.
Burgerhart JS, Schotborgh CAI, Schoon EJ, Smulders JF, van de Meeberg PC, Siersema PD, et al. Effect of Sleeve Gastrectomy on Gastroesophageal Reflux. Obesity Surgery. 2014;24:1436–41.
Lyon A, Gibson SC, De-Loyde K, Martin D. Gastroesophageal reflux in laparoscopic sleeve gastrectomy: hiatal findings and their management influence outcome. Surgery for obesity and related diseases. 2014;11:530–7.
Sharma A, Aggarwal S, Ahuja V, Bal C. Evaluation of gastroesophageal reflux before and after sleeve gastrectomy using symptom scoring, scintigraphy, and endoscopy. Surgery for Obesity and Related Diseases. 2014;10:600–5.
Kavanagh R, Smith J, Bashir U, Jones D, Avgenakis E, Nau P. Optimizing bariatric surgery outcomes: a novel preoperative protocol in a bariatric population with gastroesophageal reflux disease. Surgical Endoscopy. 2020;34:1812–8.
Assalia A, Gagner M, Nedelcu M, Ramos AC, Nocca D. Gastroesophageal Reflux and Laparoscopic Sleeve Gastrectomy: Results of the First International Consensus Conference. Obesity surgery. 2020;30:3695–705.
Felsenreich DM, Langer FBFB, Kefurt R, Panhofer P, Schermann M, Beckerhinn P, et al. Weight loss, weight regain, and conversions to Roux-en-Y gastric bypass: 10-year results of laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;0:427–36.
Quezada N, Hernández J, Pérez G, et al. Laparoscopic sleeve gastrectomy conversion to Roux-en-Y gastric bypass: experience in 50 patients after 1 to 3 years of follow-up. Surg Obes Relat Dis. Elsevier. 2016;12:1611–5.
Arman GA, Himpens J, Dhaenens J, Ballet T, Vilallonga R, Leman G, et al. Long-term (11þ years) outcomes in weight, patient satisfaction, comorbidities, and gastroesophageal reflux treatment after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;12:1778–86.
Soong TC, Almalki OM, Lee WJ, et al. Revision of sleeve gastrectomy with hiatal repair with gastropexy for gastroesophageal reflux disease. Obes Surg Obes Surg. 2019;29:2381–6.
Soong TC, Almalki OM, Lee WJ, et al. Revision of sleeve gastrectomy with hiatal repair with gastropexy for gastroesophageal reflux disease. Obes Surg Obes Surg. 2019;29:2381–6.
Hawasli A, Tarakji M, Tarboush M. Laparoscopic management of severe reflux after sleeve gastrectomy using the LINX ® system: Technique and one year follow up case report. International Journal of Surgery Case Reports. 2017;30:148–51.
Vilallonga R, Sanchez-Cordero S, Alberti P, Blanco-Colino R, Garcia Ruiz de Gordejuela A, Caubet E, et al. Ligamentum Teres Cardiopexy as a Late Alternative for Gastroesophageal Reflux Disease in a Patient with Previous Reversal of Gastric Bypass to Sleeve Gastrectomy and Hiatal Hernia Repair. Obesity Surgery. 2019;29:3765–8.
Mattar SG, Qureshi F, Taylor D, Schauer PR. Treatment of refractory gastroesophageal reflux disease with radiofrequency energy (Stretta) in patients after Roux-en-Y gastric bypass. Surgical Endoscopy. 2006;20:850–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed Consent Statement
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• GERD symptoms after sleeve gastrectomy do not correlate to physical nor functional examinations.
• Hiatal hernia is the most common finding in our patients.
• Hiatal hernia should be examined and treated during conversions.
• Systematic searching for GERD should be considered after sleeve gastrectomy.
Rights and permissions
About this article
Cite this article
Curell, A., Beisani, M., García Ruiz de Gordejuela, A. et al. Outcomes of Conversion from Sleeve Gastrectomy to Roux-en-Y Gastric Bypass Due to GERD—a Retrospective Analysis of 35 Patients. OBES SURG 31, 4100–4106 (2021). https://doi.org/10.1007/s11695-021-05541-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05541-4