Abstract
Purpose
The aim of this study was to compare myocardial mechanics using global longitudinal strain (GLS) before and after single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S).
Materials and Methods
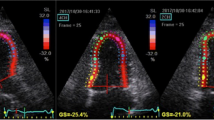
A total of 21 obese patients undergoing SADI-S were prospectively included. Transthoracic echocardiography was performed before and after the procedure, and left ventricle (LV) and right ventricle (RV) strain was assessed by two-dimensional speckle-tracking imaging (2DST).
Results
Mean time between pre-procedural and post-procedural echocardiograms was 9.2 ± 3.3 months. Postoperatively, %total weight loss (%TWL) was 33.0 ± 1.7 and % excess weight loss (%EWL) was 75.5 ± 3.6. Body mass index (BMI) significantly decreased after surgery (45.6 ± 1.2 vs 29.6 ± 1.0; p < 0.001). Postoperatively, LV GLS experienced a significant improvement (−19.8% ± 0.5 vs −22.2% ± 0.4; p < 0.001). Regarding other relevant functional parameters, RV free-wall strain was equally recovered (−19.1% ± 0.7 vs −21.0% ± 0.8; p 0.047).
Conclusions
This study demonstrates important and favourable changes in cardiac deformation parameters after performing SADI-S. Malabsorptive bariatric techniques such as SADI-S induce significant weight loss, leading to an improvement in subclinical myocardial function in patients with obesity.



Similar content being viewed by others
References
Gadde KM, Martin CK, Berthoud HR, et al. Pathophysiology and management of obesity. JACC. 2018;71(1):79–84.
Mottillo S, Filion KB, Genest J, et al. The metabolic syndrome and cardiovascular risk: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56:1113–32.
Cañon-Montañez W, Santos A, Nunes LA, et al. Central obesity is the key component in the association of metabolic syndrome with left ventricular global longitudinal strain impairment. Rev Esp Cardiol. 2018;71(7):524–30.
Collier P, Phelan D, Klein A. A test in context: myocardial strain measured by speckle-tracking echocardiography. J Am Coll Cardiol. 2017;69(8):1043–56.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes: 5-year outcomes. N Engl J Med. 2017;376:641–51.
Sanchez-Pernaute A, Rubio MA, Perez Aguirre E, et al. Single-anastomosis duodenoileal bypass with sleeve gastrectomy: metabolic improvement and weight loss in first 100 patients. Surg Obes Relat Dis. 2013;9(5):731–5.
Sanchez-Pernaute A, Rubio MA, Cabrerizo L, et al. Single-anastomosis duodenoileal by-pass with sleeve gastrectomy (SADI-S) for obese diabetic patients. Surg Obes Relat Dis. 2015;11(5):1092–8.
Santos ECL, Del Castillo JM, Parente GBO, et al. Changes in left ventricular mechanics after sleeve gastrectomy. Obes Surg. 2020;30(2):580–6.
Frea S, Andreis A, Scarlatta V, et al. Subclinical left ventricular dysfunction in severe obesity and reverse cardiac remodeling after bariatric surgery. J Cardiovasc Echogr. 2020;30(1):22–8.
Tuluce K, Kara C, Tuluce SY, et al. Early reverse cardiac remodeling effect of laparoscopic sleeve gastrectomy. Obes Surg. 2017;27(2):364–75.
Kemaloğlu Öz T, Ünal Dayı S, Seyit H, et al. The effects of weight loss after sleeve gastrectomy on left ventricular systolic function in men versus women. J Clin Ultrasound. 2016;44(8):492–9.
Leung M, Xie M, Durmush E, et al. Weight loss with sleeve gastrectomy in obese type 2 diabetes mellitus: impact on cardiac function. Obes Surg. 2016;26(2):321–6.
Kaier TE, Morgan D, Grapsa J, et al. Ventricular remodelling post-bariatric surgery: Is the type of surgery relevant? A prospective study with 3D speckle tracking. Eur Heart J Cardiovasc Imaging. 2014;15(11):1256–62.
Koshino Y, Villarraga HR, Somers VK, et al. Changes in myocardial mechanics in patients with obesity following major weight loss after bariatric surgery. Obesity (Silver Spring). 2013;21(6):1111–8.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Ashrafian H, le Roux CW, Darzi A, et al. Effects of bariatric surgery on cardiovascular function. Circulation. 2008;118:2091–102.
Cuspidi C, Rescaldani M, Tadic M, et al. Effects of bariatric surgery on cardiac structure and function: a systematic review and meta-analysis. Am J Hypertens. 2014;27(2):146–56.
Alpert MA, Omran J, Bostick BP. Effects of obesity on cardiovascular hemodynamics, cardiac morphology, and ventricular function. Curr Obes Rep. 2016;5(4):424–34.
Lee SC, Daimon M, Di Tullio MR, et al. Beneficial effect of body weight control on left ventricular diastolic function in the general population: an analysis of longitudinal data from a health check-up clinic. Eur Heart J Cardiovasc Imaging. 2018;19:136–42.
Wang LC, Gopal DM. Preclinical systolic and diastolic dysfunctions in metabolically healthy and unhealthy obese individuals. Circ Heart Fail. 2015;8:897–904.
Dalen H, Thorstensen A, Romundstad PR, et al. Cardiovascular risk factors and systolic and diastolic cardiac function: a tissue Doppler and speckle tracking echocardiographic study. J Am Soc Echocardiogr. 2011;24(3):322–32.
Luaces M, Cachofeiro V, Garcia-Munoz-Najar A, et al. Anatomical and functional alterations of the heart in morbid obesity. Changes after bariatric surgery. Rev Esp Cardiol (Engl Ed). 2012;65(1):14–21.
Nagy E, Jermendy AL, Merkely B, et al. Clinical importance of epicardial adipose tissue. Arch Med Sci. 2017;13(4):864–74.
Sanchez-Pernaute A, Rubio Herrera MA, Perez-Aguirre E, et al. Proximal duodenal-ileal end-to-side bypass with sleeve gastrectomy: proposed technique. Obes Surg. 2007;17(12):1614–8.
Surve A, Rao R, Cottam D, et al. Early outcomes of primary SADI-S: an Australian experience. Obes Surg. 2020;30(4):1429–36.
Moon RC, Gaskins L, Teixeira AF, et al. Safety and effectiveness of single-anastomosis duodenal switch procedure: 2-year result from a single US institution. Obes Surg. 2018;6:1571–7.
Torres A, Rubio MA, Ramos-Leví AM, et al. Cardiovascular risk factors after single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S): a new effective therapeutic approach? Curr Atheroscler Rep. 2017;19(12):58.
Curcio F, Testa G, Liguori I, et al. Sarcopenia and heart failure. Nutrients. 2020;12(1):211.
Carbone S, Billingsley HE, Rodriguez-Miguelez P, et al. Lean mass abnormalities in heart failure: the role of sarcopenia, sarcopenic obesity, and cachexia. Curr Probl Cardiol. 2020;45(11):100417.
Yang TWW, Johari Y, Burton PR, et al. Bariatric surgery in patients with severe heart failure. Obes Surg. 2020;30(8):2863–9.
Taylor TV, Bozkurt B, Shayani P, et al. End-stage cardiac failure in a morbidly obese patient treated by biliopancreatic diversion and cardiac transplantation. Obes Surg. 2002;12(3):416–8.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88.
Diamantis T, Apostolou KG, Alexandrou A, et al. Review of long-term weight loss results after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2014;10(1):177–83.
Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16:233–71.
Kardassis D, Bech-Hanssen O, Schönander M, et al. The influence of body composition, fat distribution, and sustained weight loss on left ventricular mass and geometry in obesity. Obesity (Silver Spring). 2012;20:605–11.
Farsalinos KE, Daraban AM, Ünlü S, et al. Head-to-head comparison of global longitudinal strain measurements among nine different vendors: the EACVI/ASE Inter-Vendor Comparison Study. J Am Soc Echocardiogr. 2015;28(10):1171–81.
Acknowledgements
Alejandro Cruz-Utrilla holds a research-training contract ¨Rio Hortega¨ (CM20/00164) from the Spanish Ministry of Science and Innovation (Instituto de Salud Carlos III).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
Adriana Ruano-Campos has no conflict of interest to declare. Alejandro Cruz-Utrilla has no conflict of interest to declare. Leyre López-Antoñanzas has no conflict of interest to declare. Maria Luaces has no conflict of interest to declare. Leopoldo Pérez de Isla has no conflict of interest to declare. Miguel Angel Rubio Herrera has no conflict of interest to declare. Antonio Torres García has no conflict of interest to declare. Andres Sanchez-Pernaute has no conflict of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ruano-Campos, A., Cruz-Utrilla, A., López-Antoñanzas, L. et al. Evaluation of Myocardial Function Following SADI-S. OBES SURG 31, 3109–3115 (2021). https://doi.org/10.1007/s11695-021-05349-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05349-2