Abstract
Purpose
The present study purposed to investigate the effects of weight loss with LSG on echocardiographic parameters of diastolic dysfunction in subjects with morbid obesity.
Methods
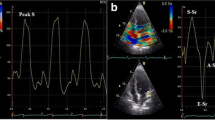
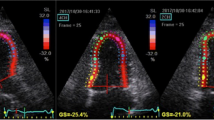
Sixty-one subjects undergoing LSG for standard indications were enrolled. All subjects underwent a physical examination, electrocardiography, and transthoracic echocardiography before and 6 months after the LSG. Peak early diastolic velocity (E), deceleration time (DT), and peak late diastolic velocity (A) were measured from the transmitral flow signal. Peak early (e′) diastolic mitral annular velocity was measured at the two acquisition sites (basal septal and basal lateral) using the tissue Doppler recordings.
Results
A significant improvement was observed in echocardiographic measures of the diastolic function including E/A ratio, E/e′ ratio, DT, and isovolumic relaxation time (IVRT) from baseline to the postoperative 6 months. Left atrial volume index (LAVI) reduced from 30.3 ± 3.9 ml/m2 to 28.0 ± 3.3 ml/m2 (p < 0.001). In addition, interventricular septum diameter (IVSD) significantly decreased from 11.3 ± 1.3 mm to 10.2 ± 1.1 mm (p < 0.001). The change in BMI was significantly correlated with the improvements in DT (r = 0.334, p = 0.012), E/e′ (r = 0.440, p = 0.001), E/A (r = − 0.317, p = 0.017), and IVRT (r = 0.348, p = 0.008).
Conclusion
LSG leads to a significant improvement in echocardiographic measures of the left ventricular diastolic function in subjects with obesity. Our findings also show that LSG leads to a reverse remodeling indicated by the decrease in interventricular septum thickness and left atrial volume index in this population.
Similar content being viewed by others
References
Kuznetsova T, Herbots L, Lopez B, et al. Prevalence of left ventricular diastolic dysfunction in a general population. Circ Heart Fail. 2009;2:105–12.
Galinier M, Pathak A, Roncalli J, et al. Obesity and cardiac failure. Arch Mal Coeur Vaiss. 2005;98:39–45.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–200.
Jeong EM, Dudley Jr SC. Diastolic dysfunction. Circ J. 2015;79:470–7.
Del Buono MG, Buckley L, Abbate A. Primary and secondary diastolic dysfunction in heart failure with preserved ejection fraction. Am J Cardiol. 2018;122:1578–87.
Rider OJ, Francis JM, Tyler D, et al. Effects of weight loss on myocardial energetics and diastolic function in obesity. Int J Cardiovasc Imaging. 2013;29:1043–50.
Kossaify A, Nicolas N. Impact of overweight and obesity on left ventricular diastolic function and value of tissue Doppler echocardiography. Clin Med Insights Cardiol. 2013;7:43–50.
Juodeikis Z, Brimas G. Long-term results after sleeve gastrectomy: a systematic review. Surg Obes Relat Dis. 2017;13:693–9.
Brethauer SA, Aminian A, Romero-Talamas H, et al. Can diabetes be surgically cured? Long-term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus. Ann Surg. 2013;258:628–36. discussion 36-7
Fried M, Yumuk V, Oppert JM, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24:42–55.
Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
(2) Classification and diagnosis of diabetes. Diabetes Care. 2015;38 Suppl:S8-s16.
Aljaroudi W, Alraies MC, Halley C, et al. Impact of progression of diastolic dysfunction on mortality in patients with normal ejection fraction. Circulation. 2012;125:782–8.
Kazik A, Wilczek K, Polonski L. Management of diastolic heart failure. Cardiol J. 2010;17:558–65.
Pascual M, Pascual DA, Soria F, et al. Effects of isolated obesity on systolic and diastolic left ventricular function. Heart. 2003;89:1152–6.
Willens HJ, Chakko SC, Lowery MH, et al. Tissue Doppler imaging of the right and left ventricle in severe obesity (body mass index >35 kg/m2). Am J Cardiol. 2004;94:1087–90.
Powell BD, Redfield MM, Bybee KA, et al. Association of obesity with left ventricular remodeling and diastolic dysfunction in patients without coronary artery disease. Am J Cardiol. 2006;98:116–20.
Russo C, Jin Z, Homma S, et al. Effect of obesity and overweight on left ventricular diastolic function: a community-based study in an elderly cohort. J Am Coll Cardiol. 2011;57:1368–74.
Zibadi S, Cordova F, Slack EH, et al. Leptin’s regulation of obesity-induced cardiac extracellular matrix remodeling. Cardiovasc Toxicol. 2011;11:325–33.
Negi SI, Jeong EM, Shukrullah I, et al. Association of low plasma adiponectin with early diastolic dysfunction. Congest Heart Fail. 2012;18:187–91.
Shimabukuro M, Higa N, Asahi T, et al. Impaired glucose tolerance, but not impaired fasting glucose, underlies left ventricular diastolic dysfunction. Diabetes Care. 2011;34:686–90.
Rider OJ, Francis JM, Ali MK, et al. Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J Am Coll Cardiol. 2009;54:718–26.
Miranda WR, Batsis JA, Sarr MG, et al. Impact of bariatric surgery on quality of life, functional capacity, and symptoms in patients with heart failure. Obes Surg. 2013;23:1011–5.
Mikhalkova D, Holman SR, Jiang H, et al. Bariatric surgery-induced cardiac and lipidomic changes in obesity-related heart failure with preserved ejection fraction. Obesity (Silver Spring). 2018;26:284–90.
Ekinci T, Stein MW, Mazzariol FS, et al. Laparoscopic sleeve gastrectomy: everything the radiologist needs to know. Clin Imaging. 2017;43:36–41.
Hayes K, Eid G. Laparoscopic sleeve gastrectomy: surgical technique and perioperative care. Surg Clin North Am. 2016;96:763–71.
Vix M, Diana M, Liu KH, et al. Evolution of glycolipid profile after sleeve gastrectomy vs. Roux-en-Y gastric bypass: results of a prospective randomized clinical trial. Obes Surg. 2013;23:613–21.
Benaiges D, Mas-Lorenzo A, Goday A, et al. Laparoscopic sleeve gastrectomy: more than a restrictive bariatric surgery procedure? World J Gastroenterol. 2015;21:11804–14.
Himpens J, Dapri G, Cadiere GB. A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. Obes Surg. 2006;16:1450–6.
Packer M, Kitzman DW. Obesity-related heart failure with a preserved ejection fraction: the mechanistic rationale for combining inhibitors of aldosterone, neprilysin, and sodium-glucose cotransporter-2. JACC Heart Fail. 2018;6:633–9.
Pandey A, Patel KV, Vaduganathan M, et al. Physical activity, fitness, and obesity in heart failure with preserved ejection fraction. JACC Heart Fail. 2018;6:975–82.
Hall JE, do Carmo JM, da Silva AA, et al. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116:991–1006.
Laffin LJ, Majewski C, Liao C, et al. Relationship between obesity, hypertension, and aldosterone production in postmenopausal African American Women: a pilot study. J Clin Hypertens (Greenwich, Conn). 2016;18:1216–21.
Huby AC, Antonova G, Groenendyk J, et al. Adipocyte-derived hormone leptin is a direct regulator of aldosterone secretion, which promotes endothelial dysfunction and cardiac fibrosis. Circulation. 2015;132:2134–45.
Wang TJ, Larson MG, Levy D, et al. Impact of obesity on plasma natriuretic peptide levels. Circulation. 2004;109:594–600.
Das SR, Drazner MH, Dries DL, et al. Impact of body mass and body composition on circulating levels of natriuretic peptides: results from the Dallas Heart Study. Circulation. 2005;112:2163–8.
Singh A, Addetia K, Maffessanti F, et al. LA strain for categorization of LV diastolic dysfunction. JACC Cardiovasc Imaging. 2017;10:735–43.
Chacko BR, Karur GR, Connelly KA, et al. Left ventricular structure and diastolic function by cardiac magnetic resonance imaging in hypertrophic cardiomyopathy. Indian Heart J. 2018;70:75–81.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Patient Selection
The present prospective cohort study was conducted on patients with morbid obesity who were scheduled for LSG in Sanliurfa Mehmet Akif Inan Research and Training Hospital between December 2018 and June 2019.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaya, B.C., Elkan, H. Impact of Weight Loss with Laparoscopic Sleeve Gastrectomy on Left Ventricular Diastolic Function: a Prospective Study. OBES SURG 30, 3280–3286 (2020). https://doi.org/10.1007/s11695-020-04573-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04573-6